Monday Poster Session
Category: Colon
P2517 - Beyond the Stricture: Unexpected Dual Malignancy in the Colon
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- NA
Nick Adimi, MD, MS, BS
Advocate Lutheran General
Park Ridge, IL
Presenting Author(s)
Nick Adimi, MD, MS, BS, Madeline Sesselmann, DO, Ahmed Khattab, MD, MRCP
Advocate Lutheran General, Park Ridge, IL
Introduction: Gastrointestinal (GI) symptoms in patients with known malignancy may result from tumor progression, metastasis, or treatment complications. Mantle cell lymphoma (MCL), a rare and aggressive B-cell non-Hodgkin lymphoma, frequently involves the GI tract. Invasive lobular carcinoma (ILC) of the breast, while more prone to GI metastasis than ductal carcinoma, rarely affects the colon. Although isolated colonic involvement by either MCL or metastatic ILC has been reported, synchronous colonic involvement by both has not, to our knowledge, been previously described. This case highlights a rare dual pathology and underscores the importance of histopathologic evaluation in oncologic patients with new GI symptoms.
Case Description/
Methods: An 84-year-old woman with MCL on zanubrutinib, metastatic ILC with osseous involvement, and chronic leukocytosis (attributed to splenectomy and BTK inhibitor therapy) was admitted with several weeks of profuse, non-bloody diarrhea and intermittent low-grade fevers. Infectious stool studies were negative.
Contrast-enhanced CT revealed multiple hypodense hepatic lesions, marked rectosigmoid thickening, and pericolonic lymphadenopathy (figure 1). Flexible sigmoidoscopy showed diffuse moderate inflammation and a non-traversable sigmoid stricture despite use of a pediatric colonoscope (figure 2). Rectosigmoid colon biopsies confirmed dual pathology: infiltration by MCL and metastatic carcinoma of breast origin. A liver biopsy performed two days earlier also demonstrated metastatic ILC with focal MCL involvement.
Following multidisciplinary discussion and a goals-of-care conversation, the patient declined further systemic therapy. Her GI symptoms were managed conservatively.
Discussion: MCL commonly involves the GI tract; ILC may rarely metastasize to the colon. However, concurrent colonic involvement by both malignancies has not been previously reported. This case exemplifies the diagnostic complexity of multifocal malignancy and reinforces the importance of histologic and immunophenotypic confirmation when evaluating new GI lesions in oncology patients. To our knowledge, this is the first reported case of simultaneous colonic involvement by MCL and metastatic ILC. It underscores the need for diagnostic vigilance and tissue confirmation in patients with multiple malignancies and new GI symptoms. Portions of this abstract were revised with the assistance of generative artificial intelligence (ChatGPT, OpenAI). All content was reviewed, verified, and finalized by the authors.

Figure: Figure 1. Coronal contrast-enhanced CT image of the abdomen and pelvis demonstrating marked circumferential thickening of the rectosigmoid colon with surrounding pericolonic lymphadenopathy. Multiple hypodense hepatic lesions are also noted, concerning for metastatic disease.
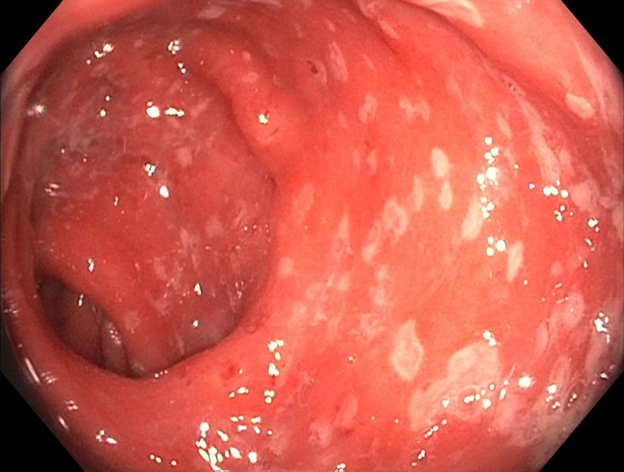
Figure: Figure 2. Endoscopic image from flexible sigmoidoscopy showing moderate diffuse inflammation of the rectosigmoid mucosa with loss of vascular pattern, mucosal friability, and luminal narrowing.
Disclosures:
Nick Adimi indicated no relevant financial relationships.
Madeline Sesselmann indicated no relevant financial relationships.
Ahmed Khattab indicated no relevant financial relationships.
Nick Adimi, MD, MS, BS, Madeline Sesselmann, DO, Ahmed Khattab, MD, MRCP. P2517 - Beyond the Stricture: Unexpected Dual Malignancy in the Colon, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Advocate Lutheran General, Park Ridge, IL
Introduction: Gastrointestinal (GI) symptoms in patients with known malignancy may result from tumor progression, metastasis, or treatment complications. Mantle cell lymphoma (MCL), a rare and aggressive B-cell non-Hodgkin lymphoma, frequently involves the GI tract. Invasive lobular carcinoma (ILC) of the breast, while more prone to GI metastasis than ductal carcinoma, rarely affects the colon. Although isolated colonic involvement by either MCL or metastatic ILC has been reported, synchronous colonic involvement by both has not, to our knowledge, been previously described. This case highlights a rare dual pathology and underscores the importance of histopathologic evaluation in oncologic patients with new GI symptoms.
Case Description/
Methods: An 84-year-old woman with MCL on zanubrutinib, metastatic ILC with osseous involvement, and chronic leukocytosis (attributed to splenectomy and BTK inhibitor therapy) was admitted with several weeks of profuse, non-bloody diarrhea and intermittent low-grade fevers. Infectious stool studies were negative.
Contrast-enhanced CT revealed multiple hypodense hepatic lesions, marked rectosigmoid thickening, and pericolonic lymphadenopathy (figure 1). Flexible sigmoidoscopy showed diffuse moderate inflammation and a non-traversable sigmoid stricture despite use of a pediatric colonoscope (figure 2). Rectosigmoid colon biopsies confirmed dual pathology: infiltration by MCL and metastatic carcinoma of breast origin. A liver biopsy performed two days earlier also demonstrated metastatic ILC with focal MCL involvement.
Following multidisciplinary discussion and a goals-of-care conversation, the patient declined further systemic therapy. Her GI symptoms were managed conservatively.
Discussion: MCL commonly involves the GI tract; ILC may rarely metastasize to the colon. However, concurrent colonic involvement by both malignancies has not been previously reported. This case exemplifies the diagnostic complexity of multifocal malignancy and reinforces the importance of histologic and immunophenotypic confirmation when evaluating new GI lesions in oncology patients. To our knowledge, this is the first reported case of simultaneous colonic involvement by MCL and metastatic ILC. It underscores the need for diagnostic vigilance and tissue confirmation in patients with multiple malignancies and new GI symptoms. Portions of this abstract were revised with the assistance of generative artificial intelligence (ChatGPT, OpenAI). All content was reviewed, verified, and finalized by the authors.

Figure: Figure 1. Coronal contrast-enhanced CT image of the abdomen and pelvis demonstrating marked circumferential thickening of the rectosigmoid colon with surrounding pericolonic lymphadenopathy. Multiple hypodense hepatic lesions are also noted, concerning for metastatic disease.
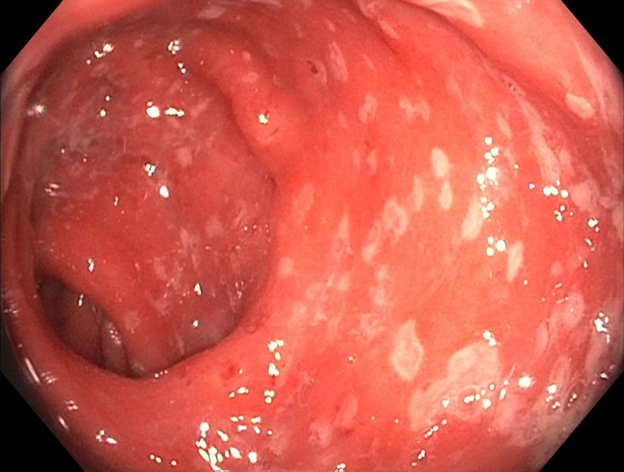
Figure: Figure 2. Endoscopic image from flexible sigmoidoscopy showing moderate diffuse inflammation of the rectosigmoid mucosa with loss of vascular pattern, mucosal friability, and luminal narrowing.
Disclosures:
Nick Adimi indicated no relevant financial relationships.
Madeline Sesselmann indicated no relevant financial relationships.
Ahmed Khattab indicated no relevant financial relationships.
Nick Adimi, MD, MS, BS, Madeline Sesselmann, DO, Ahmed Khattab, MD, MRCP. P2517 - Beyond the Stricture: Unexpected Dual Malignancy in the Colon, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
