Monday Poster Session
Category: Colon
P2503 - All Those “Mastzelle:” Not a Montezuma's Revenge
- MP
Maryam Pourjalil, MSN, DNP (she/her/hers)
Providence Cedars-Sinai Tarzana Medical Center
Encino, CA
Presenting Author(s)
1Providence Cedars-Sinai Tarzana Medical Center, Encino, CA; 2Valley Presbyterian Hospital, Van Nuys, CA; 3Providence Cedars-Sinai Tarzana Medical Center, Torrance, CA
Introduction:
Evaluation of diarrhea can be challenging and fascinating as this can be the most common and only presentation of a long-standing systemic illness.
Case Description/
Methods:
A 38 yrs old female presented with chronic watery diarrhea preceded by lower abdominal cramps of 3 months duration. The diarrhea was non bloody, occurs 5-6 liquid brown bowel movements/day, with few nocturnal accidents and weight loss. No fever, hematochezia, rash, flushing or pruritus. Denied any recent travel outside United states.
She had no history of prior surgeries. Family history was pertinent for colon cancer diagnosed in her father at the age of 56yrs old. No history of smoking, alcohol, marijuana or other substances of abuse. She is allergic to shellfish & alcohol leading to rash, itchiness and hives.
Physical exam revealed a well-developed female with a normal exam. Stool culture, Clostridium difficile screening, stool ova and parasite, fecal elastase, alpha fetal protein were within normal limits. Routine labs were within the normal range
Computerized tomography of the abdomen didn’t reveal any abnormalities. A diagnosis of irritable bowel syndrome was entertained and was referred to gastroenterology for colonoscopy.
Colonoscopy was uneventful, mucosa appeared normal with normal vasculature. No erythema, erosions, ulcerations or mass lesions seen. Random colon biopsies were obtained during colonoscopy.
Pathology revealed Abnormally hypogranular mast cells in sub-epithelium, clustered, light co-infiltrate of eosinophils, with strong CD117 ckit immunohistochemistry ( Fig.1) and negative Tryptase immunohistochemistry ( fig.2) suggestive of systemic mastocytosis.
She started on proton pump inhibitors and budesonide with some decrease in her watery diarrhea, without a complete remission. She is awaiting a hematology evaluation at present.
Discussion:
Systemic mastocytosis is an uncommon cause for prolonged gastrointestinal symptoms that could go undiagnosed. A high index of suspicion is the key in this subset of patients as the presentation is very nonspecific. There are no validated treatments for GI symptoms of SM. This condition has an unpredictable relapse rate, and patients should be educated about the importance of medication and lifestyle compliance.
If the symptoms are not responding to first line agents, referral to hematology/oncology is imperative as these patients may have concomitant bone marrow involvement and could benefit from KIT & PDGFRA inhibitors.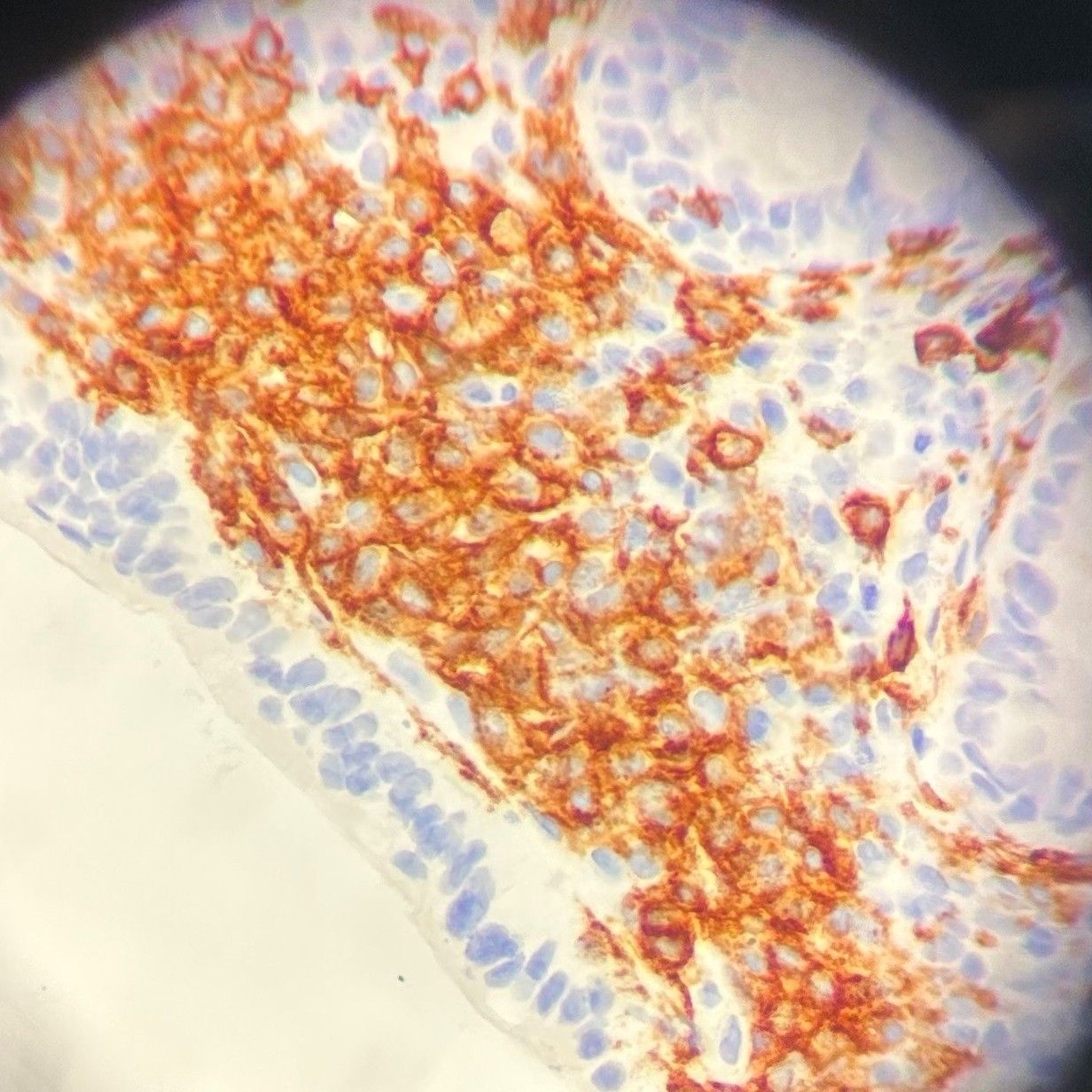
Figure: Colonic mucosa 400x, CD117 ckit immunohistochemistry. Strongly stains abnormal mast cell population.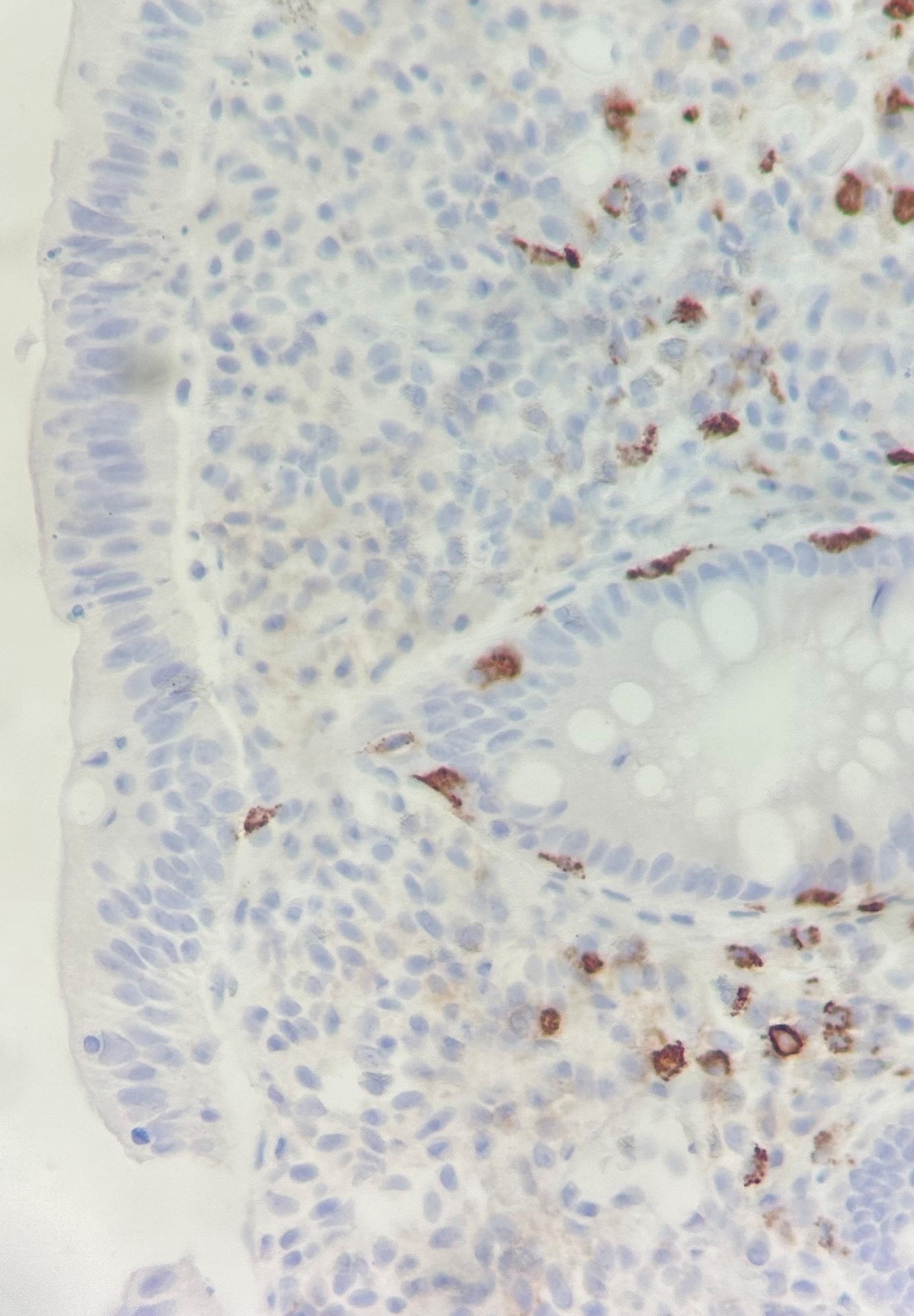
Figure: Colonic mucosa 400x, Tryptase immunohistochemistry. No staining, confirms abnormal and hypo granular mast cell population in clusters; background normal mast cells serve as internal control.
Disclosures:
Maryam Pourjalil indicated no relevant financial relationships.
Victoria DeFelica indicated no relevant financial relationships.
Galen Cortina indicated no relevant financial relationships.
Jay Krishnan indicated no relevant financial relationships.
Maryam Pourjalil, MSN, DNP1, Victoria DeFelica, BSN, NP1, Galen Cortina, MD2, Jay Krishnan, MBBS, MD3. P2503 - All Those “Mastzelle:” Not a Montezuma's Revenge, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
