Monday Poster Session
Category: Colon
P2496 - Sigmoid Stent Migration: When the Solution Becomes the Problem
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MB
Ma. Angela Baquiran, MD, MBA (she/her/hers)
Mary Washington Healthcare
Alexandria, VA
Presenting Author(s)
Ma. Angela Baquiran, MD, MBA1, Ganesh Ramaprasad, MD2, Akash Ajmera, MD2
1Mary Washington Healthcare, Alexandria, VA; 2Mary Washington Healthcare, Fredericksburg, VA
Introduction: Colonic stenting is often used as a minimally invasive procedure to relieve obstructive symptoms commonly caused by colorectal cancer. This clinical case explores the complications arising from stent migration in the setting of a reduction in tumor size resulting in the very symptom it was intended to alleviate.
Case Description/
Methods: A 76-year-old female with an extensive medical history significant for recurrent oligo-metastatic sigmoid colon adenocarcinoma on chemotherapy with a 9cm palliative sigmoid stent placement due to severe stricture in the sigmoid colon from recurrent pelvic masses who presented 8 months after stent placement due to abdominal pain with associated diarrhea for a one-week duration leading to her admission for colitis. During her hospital stay, hemoglobin dropped from 8.3 to 6.6 prompting blood transfusion. CT GI bleed was ordered and noted interval migration of the previous sigmoid colon stent now located at the rectum with the proximal portion noted against the right lateral rectal wall in the distal end located at the possible anal canal, which is the likely cause of the patient’s overflow diarrhea. Gastroenterology planned for colonoscopy and removal of migrated stent, however due to institutional guidelines, colorectal surgery was consulted for flex sigmoidoscopy and stent removal leading to patient’s prompt resolution of symptoms.
Discussion: As one of the leading malignancies, management of colorectal cancer has evolved. Prior to colorectal stenting, obstructive colorectal cancer was often treated with emergency surgery that resulted in patients with a colostomy. The introduction of metallic stents has allowed patients to have a minimally invasive route that can address acute symptoms until they are able to undergo further surgeries if needed. In our patient’s case, a stent was initially placed for palliative purposes. After which, the patient underwent chemotherapy, which led to a decrease in tumor size resulting in the eventual stent migration. In review of literature, most stent migration occurs within the first 4 months of placement with stent protrusion. However, our patient presented on the 8th month without the typical presentation of anorectal protrusion, but rather with ulceration and bleeding which are less common, accounting for up to 4% of cases, of which only 1% of the cases requiring transfusion. We present this case to increase vigilance of stent migration and its complications in patients who are actively on tumor reducing therapies.
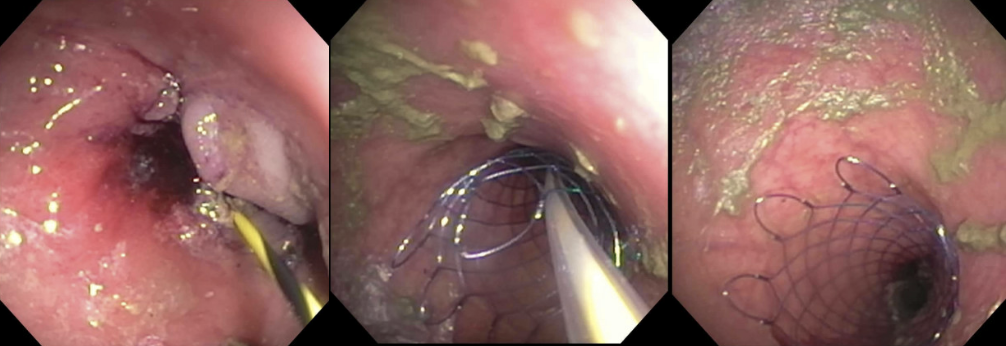
Figure: Image 1. Initial 9cm palliative sigmoid stent deployment under endoscopy prior chemotherapy initiation.

Figure: Image 2. Oblique orientation of the stent with marked distention of the rectum and sigmoid colon concerning for fecal impaction causing colitis.
Disclosures:
Ma. Angela Baquiran indicated no relevant financial relationships.
Ganesh Ramaprasad indicated no relevant financial relationships.
Akash Ajmera indicated no relevant financial relationships.
Ma. Angela Baquiran, MD, MBA1, Ganesh Ramaprasad, MD2, Akash Ajmera, MD2. P2496 - Sigmoid Stent Migration: When the Solution Becomes the Problem, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mary Washington Healthcare, Alexandria, VA; 2Mary Washington Healthcare, Fredericksburg, VA
Introduction: Colonic stenting is often used as a minimally invasive procedure to relieve obstructive symptoms commonly caused by colorectal cancer. This clinical case explores the complications arising from stent migration in the setting of a reduction in tumor size resulting in the very symptom it was intended to alleviate.
Case Description/
Methods: A 76-year-old female with an extensive medical history significant for recurrent oligo-metastatic sigmoid colon adenocarcinoma on chemotherapy with a 9cm palliative sigmoid stent placement due to severe stricture in the sigmoid colon from recurrent pelvic masses who presented 8 months after stent placement due to abdominal pain with associated diarrhea for a one-week duration leading to her admission for colitis. During her hospital stay, hemoglobin dropped from 8.3 to 6.6 prompting blood transfusion. CT GI bleed was ordered and noted interval migration of the previous sigmoid colon stent now located at the rectum with the proximal portion noted against the right lateral rectal wall in the distal end located at the possible anal canal, which is the likely cause of the patient’s overflow diarrhea. Gastroenterology planned for colonoscopy and removal of migrated stent, however due to institutional guidelines, colorectal surgery was consulted for flex sigmoidoscopy and stent removal leading to patient’s prompt resolution of symptoms.
Discussion: As one of the leading malignancies, management of colorectal cancer has evolved. Prior to colorectal stenting, obstructive colorectal cancer was often treated with emergency surgery that resulted in patients with a colostomy. The introduction of metallic stents has allowed patients to have a minimally invasive route that can address acute symptoms until they are able to undergo further surgeries if needed. In our patient’s case, a stent was initially placed for palliative purposes. After which, the patient underwent chemotherapy, which led to a decrease in tumor size resulting in the eventual stent migration. In review of literature, most stent migration occurs within the first 4 months of placement with stent protrusion. However, our patient presented on the 8th month without the typical presentation of anorectal protrusion, but rather with ulceration and bleeding which are less common, accounting for up to 4% of cases, of which only 1% of the cases requiring transfusion. We present this case to increase vigilance of stent migration and its complications in patients who are actively on tumor reducing therapies.
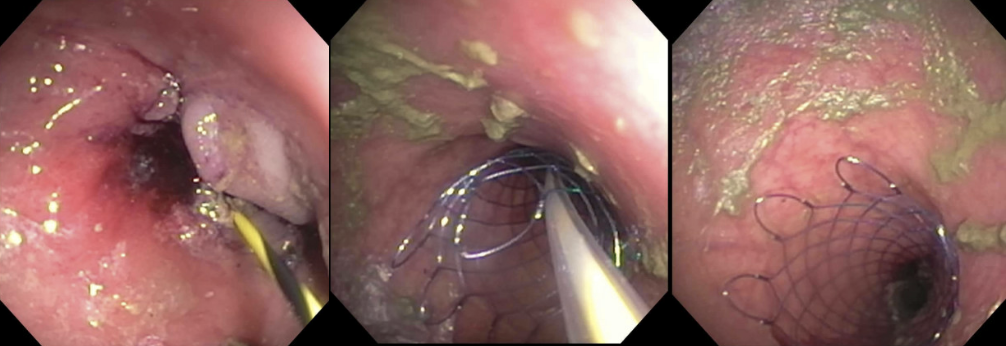
Figure: Image 1. Initial 9cm palliative sigmoid stent deployment under endoscopy prior chemotherapy initiation.

Figure: Image 2. Oblique orientation of the stent with marked distention of the rectum and sigmoid colon concerning for fecal impaction causing colitis.
Disclosures:
Ma. Angela Baquiran indicated no relevant financial relationships.
Ganesh Ramaprasad indicated no relevant financial relationships.
Akash Ajmera indicated no relevant financial relationships.
Ma. Angela Baquiran, MD, MBA1, Ganesh Ramaprasad, MD2, Akash Ajmera, MD2. P2496 - Sigmoid Stent Migration: When the Solution Becomes the Problem, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

