Monday Poster Session
Category: Biliary/Pancreas
P2381 - An Uncommon Tract: Gastrohepatic Cutaneous Fistula Due to Chronic Pancreatitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Migara Jayasekera, MD
University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Migara Jayasekera, MD1, Valerie Quach, BS2, Christo Mathew, MD3
1University of Texas Medical Branch, Galveston, TX; 2John Sealy School of Medicine, University of Texas Medical Branch, Galveston, TX; 3University of Texas Medical Branch, Department of Gastroenterology and Hepatology, Galveston, TX
Introduction: A gastrohepatic cutaneous fistula is a rare pathological connection in which an epithelialized tract extends from the external abdominal wall into the gastrohepatic space—a potential space between the left lobe of the liver and the lesser curvature of the stomach. These fistulas typically arise secondary to chronic inflammation, abscess formation, malignancy, or prior surgical intervention. Patients often present with persistent cutaneous drainage, tenderness, or systemic signs of infection. We present a unique case of a gastrohepatic cutaneous fistula that developed secondary to chronic pancreatitis.
Case Description/
Methods: A 35-year-old male with a history of alcoholic chronic pancreatitis and pancreatic pseudocyst presented with one month of worsening abdominal pain. He was afebrile and hemodynamically stable, with leukocytosis and signs of malnutrition. On examination, we noted an abscess-like structure on his right abdominal wall. Computed tomography (CT) imaging revealed peripancreatic inflammation and suggested a gastrocutaneous fistulous tract extending from the upper abdomen to the skin surface. Esophagogastroduodenoscopy (EGD) revealed friable mucosa along the lesser curvature of the stomach, without a visible fistula opening. Paracentesis was not consistent with spontaneous bacterial peritonitis. After the abdominal wall structure ruptured spontaneously, he was discharged with wound care and instructions to follow up with surgical and gastroenterology teams. Repeat CT performed 1 month later for persistent drainage showed a larger fluid collection in the gastrohepatic space. We diagnosed a gastrohepatic cutaneous fistula based on CT and EGD findings, given that no tract was visible on EGD. The patient continues to experience complications from ongoing fistula drainage, requiring regular outpatient monitoring and multiple readmissions.
Discussion: This case highlights a rare presentation of a fistula extending from the gastrohepatic space to the external abdominal wall in a patient with chronic pancreatitis. Chronic left upper quadrant inflammation and enzymatic tissue damage from recurrent alcohol-induced pancreatic flares likely contributed to the fistula’s formation. In the absence of a discrete tract amenable to closure, we prioritized supportive care, including drainage, antibiotics, and nutritional support, as the mainstay of treatment. We reserve surgical intervention for patients with persistent or complicated fistulas that do not respond to conservative measures.

Figure: Gastric body with a focal area of erythema and friability on the lesser curvature
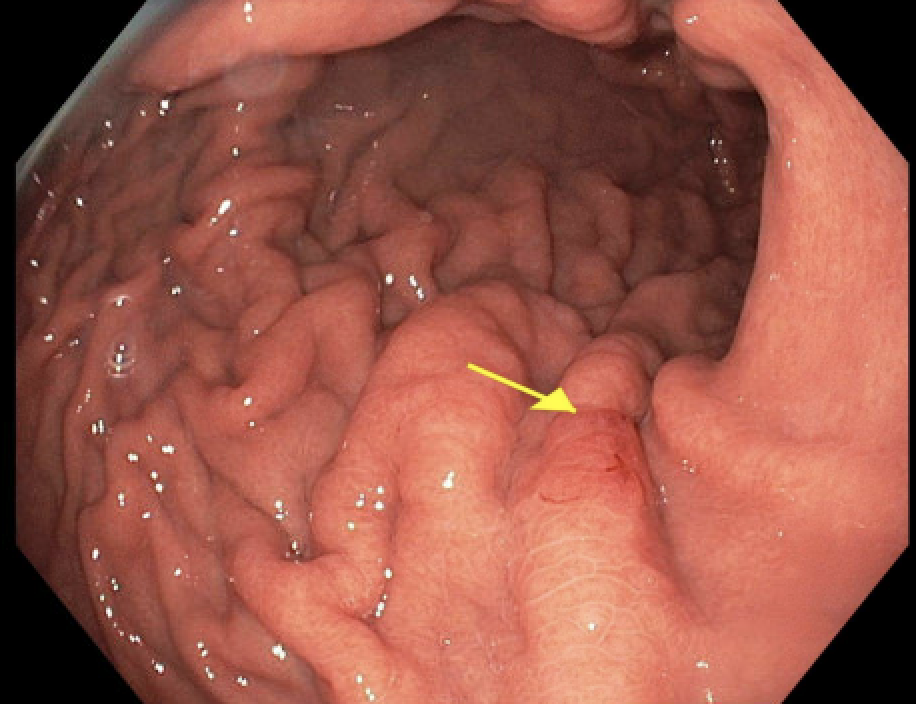
Figure: Abdominal Computed Tomography showing fistula from the gastrohepatic space to the abdominal wall
Disclosures:
Migara Jayasekera indicated no relevant financial relationships.
Valerie Quach indicated no relevant financial relationships.
Christo Mathew indicated no relevant financial relationships.
Migara Jayasekera, MD1, Valerie Quach, BS2, Christo Mathew, MD3. P2381 - An Uncommon Tract: Gastrohepatic Cutaneous Fistula Due to Chronic Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas Medical Branch, Galveston, TX; 2John Sealy School of Medicine, University of Texas Medical Branch, Galveston, TX; 3University of Texas Medical Branch, Department of Gastroenterology and Hepatology, Galveston, TX
Introduction: A gastrohepatic cutaneous fistula is a rare pathological connection in which an epithelialized tract extends from the external abdominal wall into the gastrohepatic space—a potential space between the left lobe of the liver and the lesser curvature of the stomach. These fistulas typically arise secondary to chronic inflammation, abscess formation, malignancy, or prior surgical intervention. Patients often present with persistent cutaneous drainage, tenderness, or systemic signs of infection. We present a unique case of a gastrohepatic cutaneous fistula that developed secondary to chronic pancreatitis.
Case Description/
Methods: A 35-year-old male with a history of alcoholic chronic pancreatitis and pancreatic pseudocyst presented with one month of worsening abdominal pain. He was afebrile and hemodynamically stable, with leukocytosis and signs of malnutrition. On examination, we noted an abscess-like structure on his right abdominal wall. Computed tomography (CT) imaging revealed peripancreatic inflammation and suggested a gastrocutaneous fistulous tract extending from the upper abdomen to the skin surface. Esophagogastroduodenoscopy (EGD) revealed friable mucosa along the lesser curvature of the stomach, without a visible fistula opening. Paracentesis was not consistent with spontaneous bacterial peritonitis. After the abdominal wall structure ruptured spontaneously, he was discharged with wound care and instructions to follow up with surgical and gastroenterology teams. Repeat CT performed 1 month later for persistent drainage showed a larger fluid collection in the gastrohepatic space. We diagnosed a gastrohepatic cutaneous fistula based on CT and EGD findings, given that no tract was visible on EGD. The patient continues to experience complications from ongoing fistula drainage, requiring regular outpatient monitoring and multiple readmissions.
Discussion: This case highlights a rare presentation of a fistula extending from the gastrohepatic space to the external abdominal wall in a patient with chronic pancreatitis. Chronic left upper quadrant inflammation and enzymatic tissue damage from recurrent alcohol-induced pancreatic flares likely contributed to the fistula’s formation. In the absence of a discrete tract amenable to closure, we prioritized supportive care, including drainage, antibiotics, and nutritional support, as the mainstay of treatment. We reserve surgical intervention for patients with persistent or complicated fistulas that do not respond to conservative measures.

Figure: Gastric body with a focal area of erythema and friability on the lesser curvature
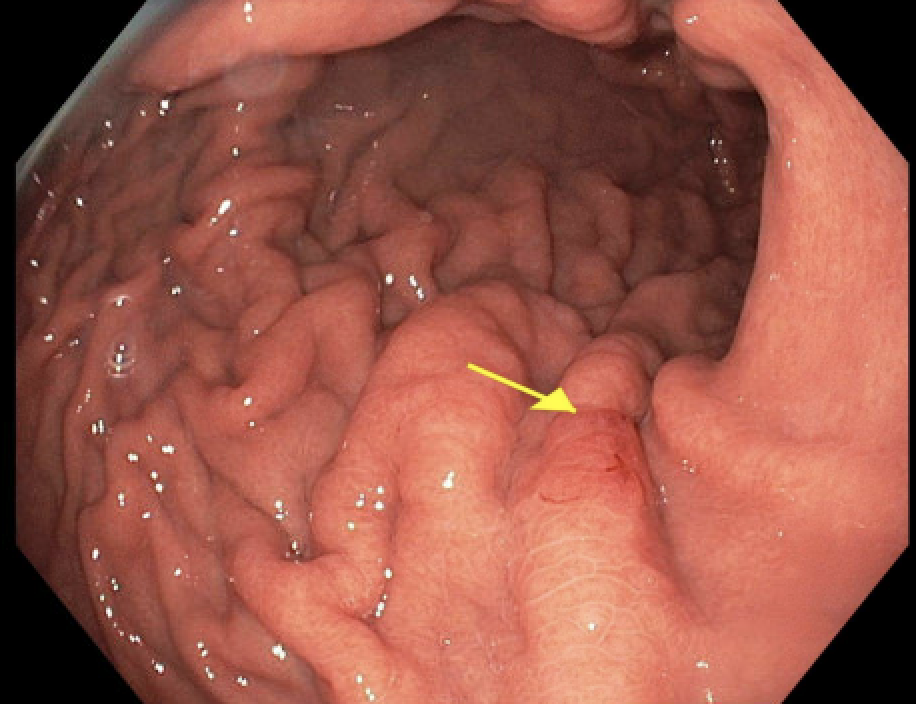
Figure: Abdominal Computed Tomography showing fistula from the gastrohepatic space to the abdominal wall
Disclosures:
Migara Jayasekera indicated no relevant financial relationships.
Valerie Quach indicated no relevant financial relationships.
Christo Mathew indicated no relevant financial relationships.
Migara Jayasekera, MD1, Valerie Quach, BS2, Christo Mathew, MD3. P2381 - An Uncommon Tract: Gastrohepatic Cutaneous Fistula Due to Chronic Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
