Monday Poster Session
Category: Biliary/Pancreas
P2373 - Cholecystitis Complicated by Pyogenic Liver Abscess and Hepatic Vein Thrombosis: A Rare Lactobacillus Infection
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ahmad Zain, MBBS (he/him/his)
Parkview Medical Center
Pueblo, CO
Presenting Author(s)
Ahmad Zain, MBBS1, Amil Shah, DO1, Hammad Qadri, DO2, Fatima Ashfaq, MBBS3, Shan Tandon, MD1, Syed Rafay H zaidi, MBBS1, Muhammad Sohaib, MBBS1, Bryant Javier, DO1, Mustafa Nayeem, MD1, Malik Ahsan Safdar, MBBS4
1Parkview Medical Center, Pueblo, CO; 2United Health Services, Wilson Medical Center, Vestal, NY; 3Nishtar Medical University, Multan, Punjab, Pakistan; 4Services Institute of Medical Sciences, Lahore, Punjab, Pakistan
Introduction: Although the incidence of pyogenic liver abscesses PLA is very low in the western countries but carries a significant mortality risk ranging 5.6-10% which can rise to 22% in cases of multiple hepatic abscesses. Cholecystitis, with or without cholelithiasis, is often associated with synchronous liver abscesses which can further be complicated by a hepatic and portal venous thrombosis due to underlying severe inflammatory response to infection. Early diagnosis and treatment of underlying conditions are crucial to improving patient outcomes.
Case Description/
Methods: A 66-year-old female presented with two weeks of upper abdominal pain, nausea, vomiting, and loss of appetite. Initial evaluation showed thrombocytopenia, leukocytosis, elevated lactate, and hyperglycemia with right upper quadrant and epigastric tenderness. Liver function tests showed mild hyperbilirubinemia and transaminitis. HIDA scan confirmed cholecystitis, and CT revealed gallbladder wall thickening, pneumobilia, middle hepatic vein thrombosis, and multiple hepatic hypodensities up to 3.4 cm. She was started on IV Zosyn pending culture results. Interventional radiology drained the gallbladder, and gram stains revealed gram-positive rods, gram-positive cocci, and gram-negative rods. Blood cultures identified Streptococcus anginosus as the likely pathogen. A follow-up CT showed increased hepatic abscess size, prompting placement of a new drain, which also grew Streptococcus anginosus. With resolution of leukocytosis, improved liver function, and hemodynamic stability, the patient was discharged on oral amoxicillin 1 g every eight hours for four weeks with outpatient follow-up for elective cholecystectomy. Thrombocytopenia (platelet count 20) improved to 135, attributed to infection. Anticoagulation with apixaban was initiated per vascular recommendations, with outpatient re-evaluation planned.
Discussion: PLA with underlying infected biliary system is unusual but has been reported in literature. Mortality significantly increases with multiple abscesses complicated by venous thrombosis, such as hepatic or portal vein thrombosis, which occurs in up to 42% of cases. Advances in the imaging have increased detection of venous thrombosis,however, hepatic or portal vein thrombosis with concurrent APL can mimic hepatic malignancy and should be considered keenly. Prompt multidisciplinary approach for urgent intervention including surgery, drainage and broad antibiotics should be immediately considered to prevent high risk complications.
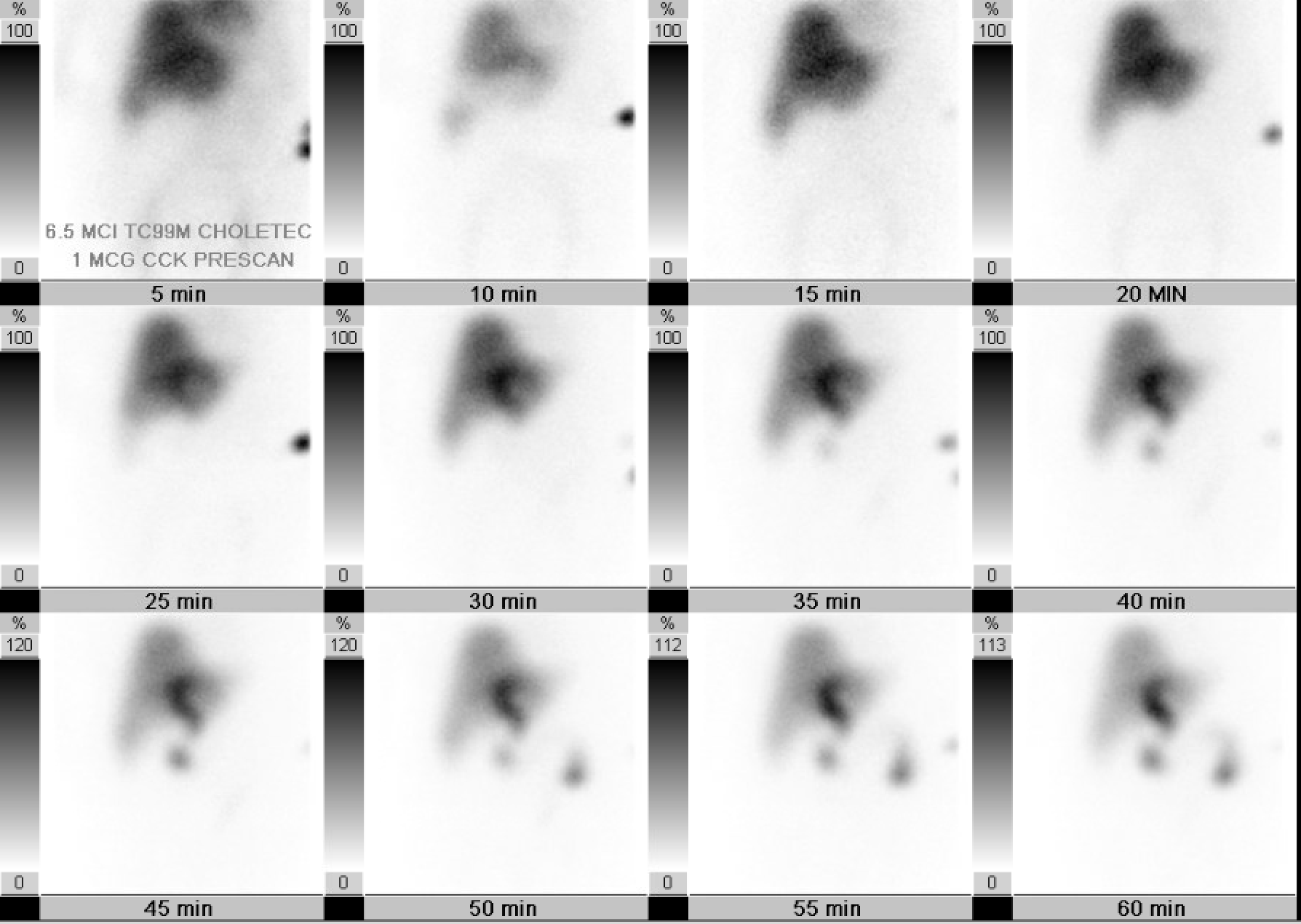
Figure: A= Liver abscess on initial encounter
B= Repeat interval CT with increased size of liver abscess
C= CT scan with IR drain in place for liver abscess
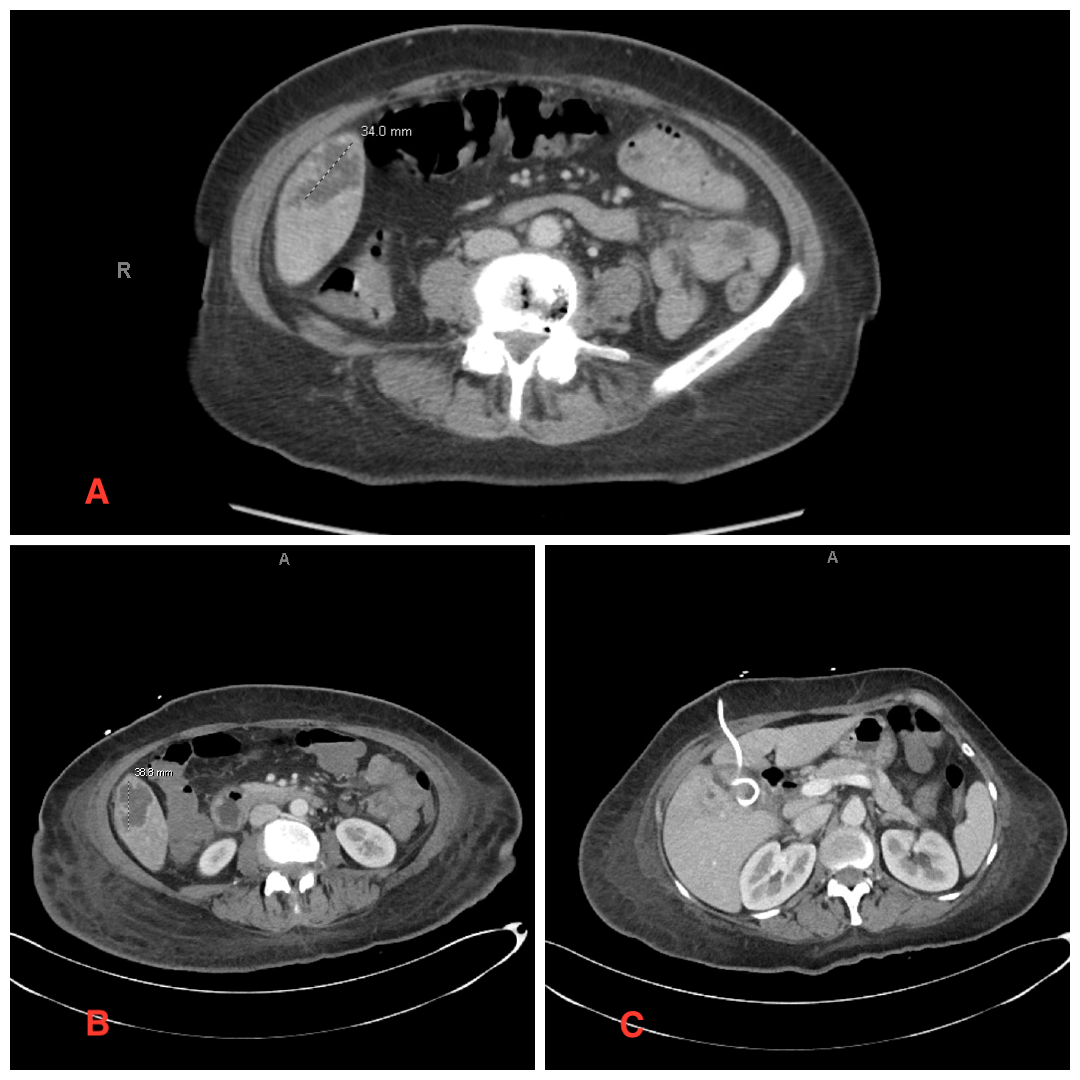
Figure: HIDA scan showing gallbladder filling defect
Disclosures:
Ahmad Zain indicated no relevant financial relationships.
Amil Shah indicated no relevant financial relationships.
Hammad Qadri indicated no relevant financial relationships.
Fatima Ashfaq indicated no relevant financial relationships.
Shan Tandon indicated no relevant financial relationships.
Syed Rafay H zaidi indicated no relevant financial relationships.
Muhammad Sohaib indicated no relevant financial relationships.
Bryant Javier indicated no relevant financial relationships.
Mustafa Nayeem indicated no relevant financial relationships.
Malik Ahsan Safdar indicated no relevant financial relationships.
Ahmad Zain, MBBS1, Amil Shah, DO1, Hammad Qadri, DO2, Fatima Ashfaq, MBBS3, Shan Tandon, MD1, Syed Rafay H zaidi, MBBS1, Muhammad Sohaib, MBBS1, Bryant Javier, DO1, Mustafa Nayeem, MD1, Malik Ahsan Safdar, MBBS4. P2373 - Cholecystitis Complicated by Pyogenic Liver Abscess and Hepatic Vein Thrombosis: A Rare Lactobacillus Infection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Parkview Medical Center, Pueblo, CO; 2United Health Services, Wilson Medical Center, Vestal, NY; 3Nishtar Medical University, Multan, Punjab, Pakistan; 4Services Institute of Medical Sciences, Lahore, Punjab, Pakistan
Introduction: Although the incidence of pyogenic liver abscesses PLA is very low in the western countries but carries a significant mortality risk ranging 5.6-10% which can rise to 22% in cases of multiple hepatic abscesses. Cholecystitis, with or without cholelithiasis, is often associated with synchronous liver abscesses which can further be complicated by a hepatic and portal venous thrombosis due to underlying severe inflammatory response to infection. Early diagnosis and treatment of underlying conditions are crucial to improving patient outcomes.
Case Description/
Methods: A 66-year-old female presented with two weeks of upper abdominal pain, nausea, vomiting, and loss of appetite. Initial evaluation showed thrombocytopenia, leukocytosis, elevated lactate, and hyperglycemia with right upper quadrant and epigastric tenderness. Liver function tests showed mild hyperbilirubinemia and transaminitis. HIDA scan confirmed cholecystitis, and CT revealed gallbladder wall thickening, pneumobilia, middle hepatic vein thrombosis, and multiple hepatic hypodensities up to 3.4 cm. She was started on IV Zosyn pending culture results. Interventional radiology drained the gallbladder, and gram stains revealed gram-positive rods, gram-positive cocci, and gram-negative rods. Blood cultures identified Streptococcus anginosus as the likely pathogen. A follow-up CT showed increased hepatic abscess size, prompting placement of a new drain, which also grew Streptococcus anginosus. With resolution of leukocytosis, improved liver function, and hemodynamic stability, the patient was discharged on oral amoxicillin 1 g every eight hours for four weeks with outpatient follow-up for elective cholecystectomy. Thrombocytopenia (platelet count 20) improved to 135, attributed to infection. Anticoagulation with apixaban was initiated per vascular recommendations, with outpatient re-evaluation planned.
Discussion: PLA with underlying infected biliary system is unusual but has been reported in literature. Mortality significantly increases with multiple abscesses complicated by venous thrombosis, such as hepatic or portal vein thrombosis, which occurs in up to 42% of cases. Advances in the imaging have increased detection of venous thrombosis,however, hepatic or portal vein thrombosis with concurrent APL can mimic hepatic malignancy and should be considered keenly. Prompt multidisciplinary approach for urgent intervention including surgery, drainage and broad antibiotics should be immediately considered to prevent high risk complications.
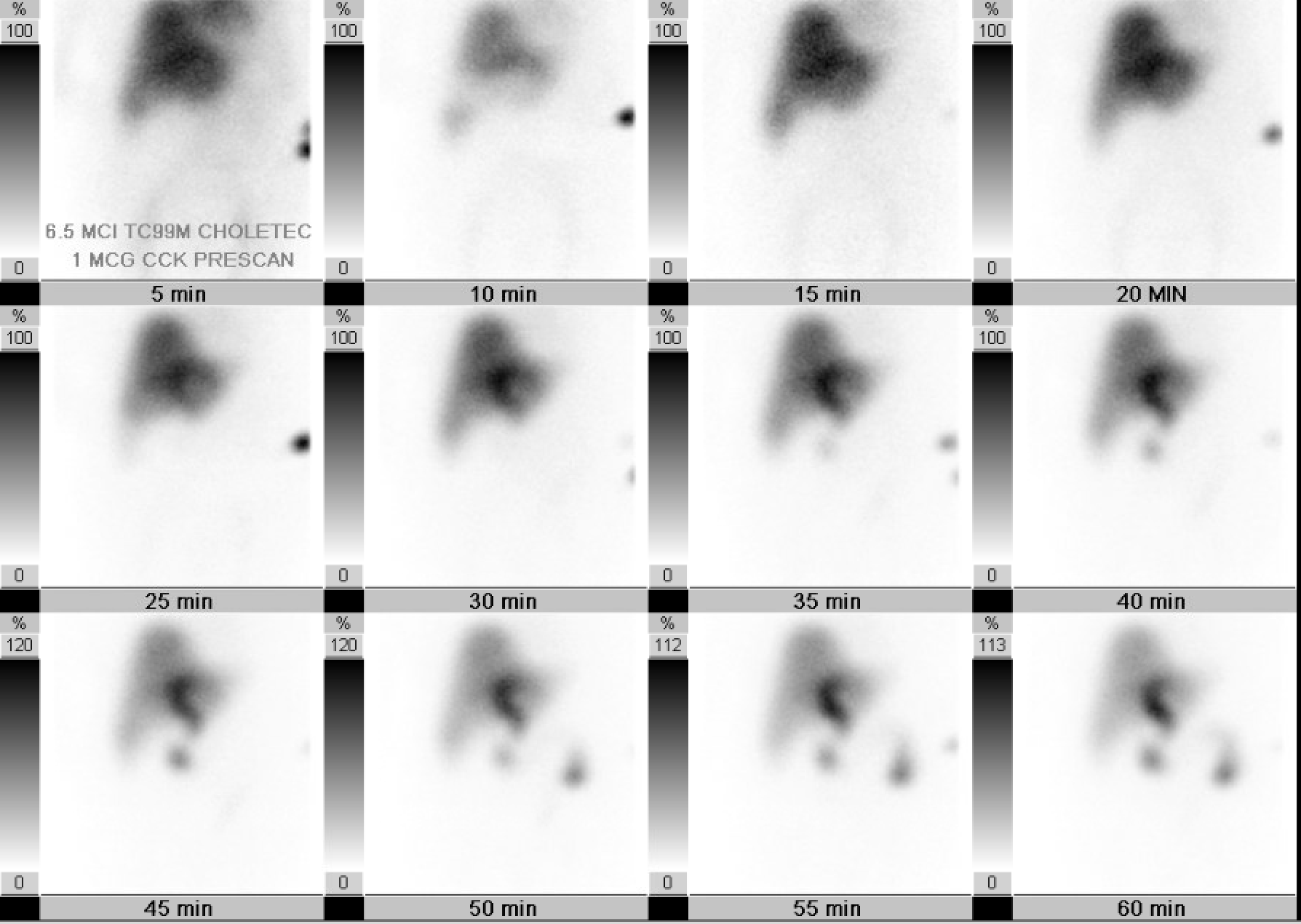
Figure: A= Liver abscess on initial encounter
B= Repeat interval CT with increased size of liver abscess
C= CT scan with IR drain in place for liver abscess
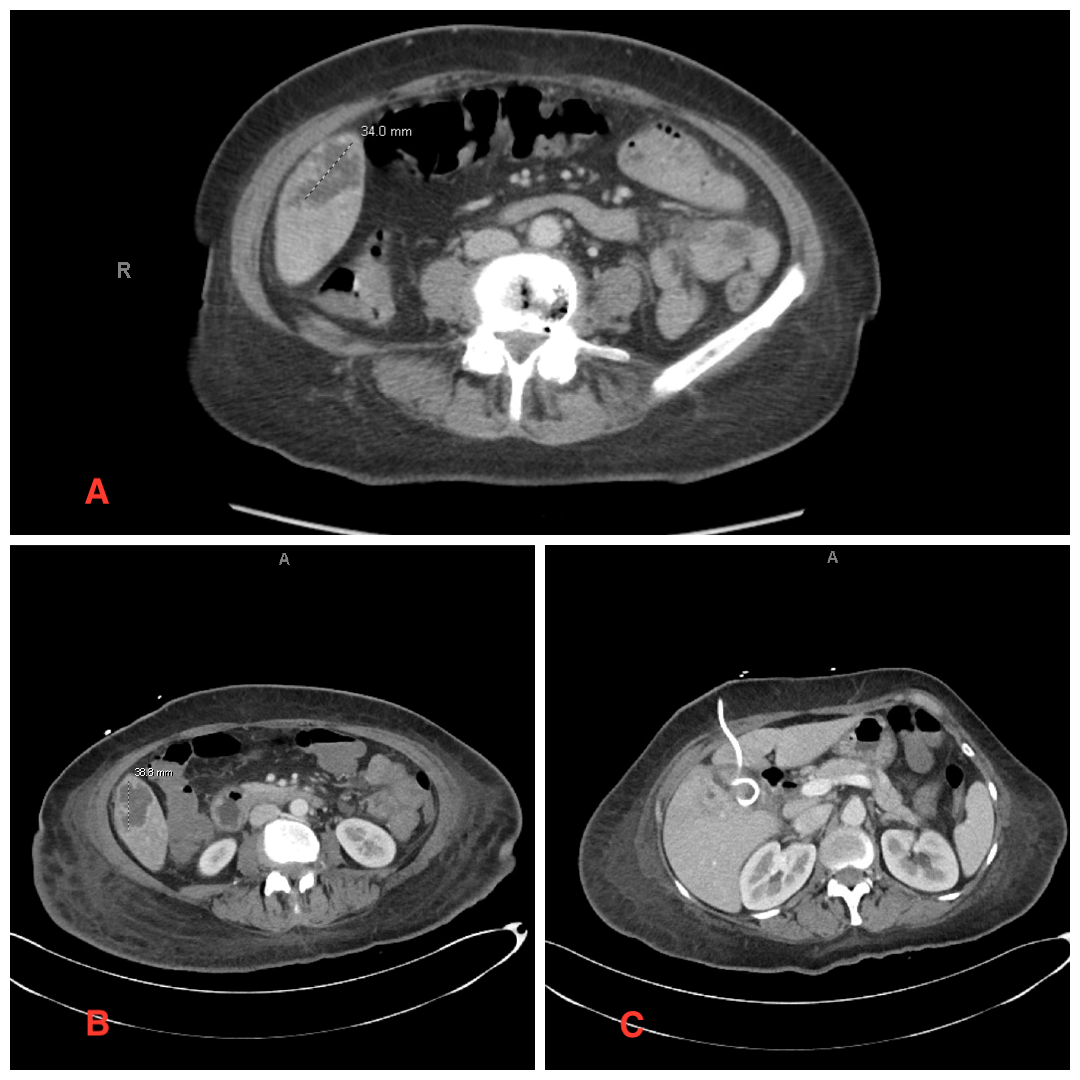
Figure: HIDA scan showing gallbladder filling defect
Disclosures:
Ahmad Zain indicated no relevant financial relationships.
Amil Shah indicated no relevant financial relationships.
Hammad Qadri indicated no relevant financial relationships.
Fatima Ashfaq indicated no relevant financial relationships.
Shan Tandon indicated no relevant financial relationships.
Syed Rafay H zaidi indicated no relevant financial relationships.
Muhammad Sohaib indicated no relevant financial relationships.
Bryant Javier indicated no relevant financial relationships.
Mustafa Nayeem indicated no relevant financial relationships.
Malik Ahsan Safdar indicated no relevant financial relationships.
Ahmad Zain, MBBS1, Amil Shah, DO1, Hammad Qadri, DO2, Fatima Ashfaq, MBBS3, Shan Tandon, MD1, Syed Rafay H zaidi, MBBS1, Muhammad Sohaib, MBBS1, Bryant Javier, DO1, Mustafa Nayeem, MD1, Malik Ahsan Safdar, MBBS4. P2373 - Cholecystitis Complicated by Pyogenic Liver Abscess and Hepatic Vein Thrombosis: A Rare Lactobacillus Infection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
