Monday Poster Session
Category: Biliary/Pancreas
P2335 - Immune Checkpoint Inhibitor-Associated Eosinophilic Pancreatitis Presenting as a Pancreatic Mass
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Abdullah Javed, MBBS (he/him/his)
Allama Iqbal Medical College
Lahore, Punjab, Pakistan
Presenting Author(s)
Abdullah Javed, MBBS1, Nihal I. Khan, MD2, Muhammad Abdullah, MBBS3, Muhammad Aftab, MD4, Charanjeet Singh, MD2
1Allama Iqbal Medical College, Lahore, Punjab, Pakistan; 2AdventHealth Orlando, Orlando, FL; 3Lahore Medical and Dental College, Lahore, Punjab, Pakistan; 4Ross University School of Medicine, Miramar, FL
Introduction: Eosinophilic pancreatitis (EP) is a rare inflammatory condition characterized by diffuse pancreatic infiltration with eosinophils, elevated serum immunoglobulin E levels, and systemic eosinophilia. Herein, we report a case of EP presenting as an enlarging pancreatic mass in a patient receiving immune checkpoint inhibitor (ICI) therapy.
Case Description/
Methods: A 57-year-old man with a history of alcoholic chronic pancreatitis and metastatic squamous cell carcinoma of the lung on pembrolizumab presented with a one-month history of generalized abdominal and back pain. Initial CT of the abdomen & pelvis revealed a 3.5 cm hypo-enhancing mass in the pancreatic neck, with adjacent pancreatic ductal dilation and calcifications. An EUS-guided fine-needle aspiration (FNA) was performed that showed atypical cells on Rapid Onsite Evaluation, though final cytology revealed eosinophil-rich inflammatory infiltrates without neoplasia. Due to inconclusive MRI findings and concern for neoplasm in the setting of metastatic lung cancer, we repeated EUS-FNA, which confirmed persistent eosinophilic infiltration, reactive acinar tissue, and IgG4-positive plasma cells lacking features of autoimmune pancreatitis (AIP) or pancreatic neoplasm. Given his ongoing pembrolizumab therapy and associated systemic eosinophilia, we suspected ICI-related EP. We held the drug indefinitely and started him on pancreatic enzyme replacement therapy. Upon periodic follow-ups, his symptoms resolved, and serial CT imaging showed a reduction in the size of the pancreatic mass. In light of these findings, immunotherapy may be cautiously reintroduced with steroids, pending oncological review and CT in three months.
Discussion: EP has an estimated incidence of less than 1%, with fewer than 20 reported cases, and lacks clear diagnostic criteria, making it a challenging entity to establish. It often presents with clinical and radiological findings resembling a pancreatic neoplasm. However, unlike malignancy, EP is a benign, steroid-responsive condition that may occur secondary to AIP, eosinophilic syndromes, or drug-induced adverse events. In our case, serial EUS-guided biopsies revealed dense eosinophilic infiltrates without features of malignancy or AIP. Given the history of ICI therapy and systemic eosinophilia, we suspected an ICI-related etiology, as these drugs are known to trigger eosinophilic infiltration. This case underscores the need to consider EP in ICI-treated patients with a pancreatic mass to avoid surgical interventions.
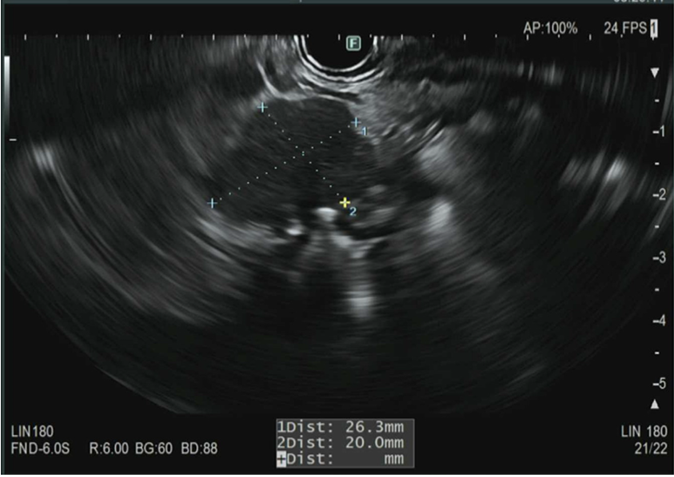
Figure: Figure 1. Endoscopic ultrasound (EUS) showing a 26 x 20 mm mass-like hypoechoic area in the neck of the pancreas and upstream pancreatic duct dilation.
Disclosures:
Abdullah Javed indicated no relevant financial relationships.
Nihal Khan indicated no relevant financial relationships.
Muhammad Abdullah indicated no relevant financial relationships.
Muhammad Aftab indicated no relevant financial relationships.
Charanjeet Singh indicated no relevant financial relationships.
Abdullah Javed, MBBS1, Nihal I. Khan, MD2, Muhammad Abdullah, MBBS3, Muhammad Aftab, MD4, Charanjeet Singh, MD2. P2335 - Immune Checkpoint Inhibitor-Associated Eosinophilic Pancreatitis Presenting as a Pancreatic Mass, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Allama Iqbal Medical College, Lahore, Punjab, Pakistan; 2AdventHealth Orlando, Orlando, FL; 3Lahore Medical and Dental College, Lahore, Punjab, Pakistan; 4Ross University School of Medicine, Miramar, FL
Introduction: Eosinophilic pancreatitis (EP) is a rare inflammatory condition characterized by diffuse pancreatic infiltration with eosinophils, elevated serum immunoglobulin E levels, and systemic eosinophilia. Herein, we report a case of EP presenting as an enlarging pancreatic mass in a patient receiving immune checkpoint inhibitor (ICI) therapy.
Case Description/
Methods: A 57-year-old man with a history of alcoholic chronic pancreatitis and metastatic squamous cell carcinoma of the lung on pembrolizumab presented with a one-month history of generalized abdominal and back pain. Initial CT of the abdomen & pelvis revealed a 3.5 cm hypo-enhancing mass in the pancreatic neck, with adjacent pancreatic ductal dilation and calcifications. An EUS-guided fine-needle aspiration (FNA) was performed that showed atypical cells on Rapid Onsite Evaluation, though final cytology revealed eosinophil-rich inflammatory infiltrates without neoplasia. Due to inconclusive MRI findings and concern for neoplasm in the setting of metastatic lung cancer, we repeated EUS-FNA, which confirmed persistent eosinophilic infiltration, reactive acinar tissue, and IgG4-positive plasma cells lacking features of autoimmune pancreatitis (AIP) or pancreatic neoplasm. Given his ongoing pembrolizumab therapy and associated systemic eosinophilia, we suspected ICI-related EP. We held the drug indefinitely and started him on pancreatic enzyme replacement therapy. Upon periodic follow-ups, his symptoms resolved, and serial CT imaging showed a reduction in the size of the pancreatic mass. In light of these findings, immunotherapy may be cautiously reintroduced with steroids, pending oncological review and CT in three months.
Discussion: EP has an estimated incidence of less than 1%, with fewer than 20 reported cases, and lacks clear diagnostic criteria, making it a challenging entity to establish. It often presents with clinical and radiological findings resembling a pancreatic neoplasm. However, unlike malignancy, EP is a benign, steroid-responsive condition that may occur secondary to AIP, eosinophilic syndromes, or drug-induced adverse events. In our case, serial EUS-guided biopsies revealed dense eosinophilic infiltrates without features of malignancy or AIP. Given the history of ICI therapy and systemic eosinophilia, we suspected an ICI-related etiology, as these drugs are known to trigger eosinophilic infiltration. This case underscores the need to consider EP in ICI-treated patients with a pancreatic mass to avoid surgical interventions.
Figure: Figure 1. Endoscopic ultrasound (EUS) showing a 26 x 20 mm mass-like hypoechoic area in the neck of the pancreas and upstream pancreatic duct dilation.
Disclosures:
Abdullah Javed indicated no relevant financial relationships.
Nihal Khan indicated no relevant financial relationships.
Muhammad Abdullah indicated no relevant financial relationships.
Muhammad Aftab indicated no relevant financial relationships.
Charanjeet Singh indicated no relevant financial relationships.
Abdullah Javed, MBBS1, Nihal I. Khan, MD2, Muhammad Abdullah, MBBS3, Muhammad Aftab, MD4, Charanjeet Singh, MD2. P2335 - Immune Checkpoint Inhibitor-Associated Eosinophilic Pancreatitis Presenting as a Pancreatic Mass, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

