Monday Poster Session
Category: Biliary/Pancreas
P2329 - Gastric Outlet Obstruction due to Pancreatic Serous Cystadenoma Relieved by Endoscopic Cystgastrostomy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Edward Cay, DO
Mclaren Greater Lansing / Michigan State University
Lansing, MI
Presenting Author(s)
Edward Cay, DO1, Austin Tiesenga, DO2, Stephen Simmer, MD3
1Mclaren Greater Lansing / Michigan State University, Lansing, MI; 2Corewell Health Lakeland, St. Joseph, MI; 3Corewell Health Grand Rapids, Grand Rapids, MI
Introduction: Pancreatic serous cystadenomas (SCAs) are typically benign asymptomatic lesions, incidentally found on cross-sectional imaging. We present a patient who underwent endoscopic ultrasound (EUS) guided cystgastrostomy for large SCA compressing the stomach causing gastric outlet obstruction.
Case Description/
Methods: A 56 year-old man with a past medical history of membranous glomerulonephritis on hemodialysis and chronic hepatitis C cirrhosis, presented with worsening painful abdominal distension for two weeks and weight loss due to early satiety. Contrast enhanced computed tomography showed a 23 cm pancreatic cystic structure with mass effect on the greater curvature of the stomach.
Endosonography demonstrated a large abdominal cyst with multiple septations, and fine needle aspiration showed CEA 1.5 ng/mL, amylase 37 U/L and paucicellular cytology suggestive of serous cystadenoma. Patient was deemed too high risk for surgery given multiple comorbidities, and underwent 2.6 L palliative drainage by interventional radiology (IR) with improvement of symptoms.
Given several recurrences over the past several months despite drainages by IR, the patient was readmitted. EUS-guided cystgastrostomy was performed on the dominant cystic lesion, with 1.5 L serous fluid drained and a lumen apposing metal stent (LAMS) placed with double pigtail stents. Repeat endoscopy two months later showed the cyst cavity with a small amount of debris, removal of LAMS and replacement of double pigtail stents to maintain drainage, which patient tolerated well.
Discussion: Pancreatic serous cystadenomas classically have a honeycomb appearance on imaging, and a pathognomonic “sunburst” central scar calcification. Fluid is usually bloody with low viscosity, low CEA and low amylase levels.
Typically less than 4 cm in size, if these lesions growth larger it may become symptomatic from mass effect, including abdominal distension and gastric outlet obstruction, as seen with our patient. Surgical management for symptomatic patients typically results in no recurrence.
While our patient had rapid reaccumulation of an extremely large SCA causing gastric outlet obstruction, his surgical candidacy was limited. This case highlights EUS guided cystgastrostomy as an alternative to surgical management to symptomatic pancreatic cystadenomas.
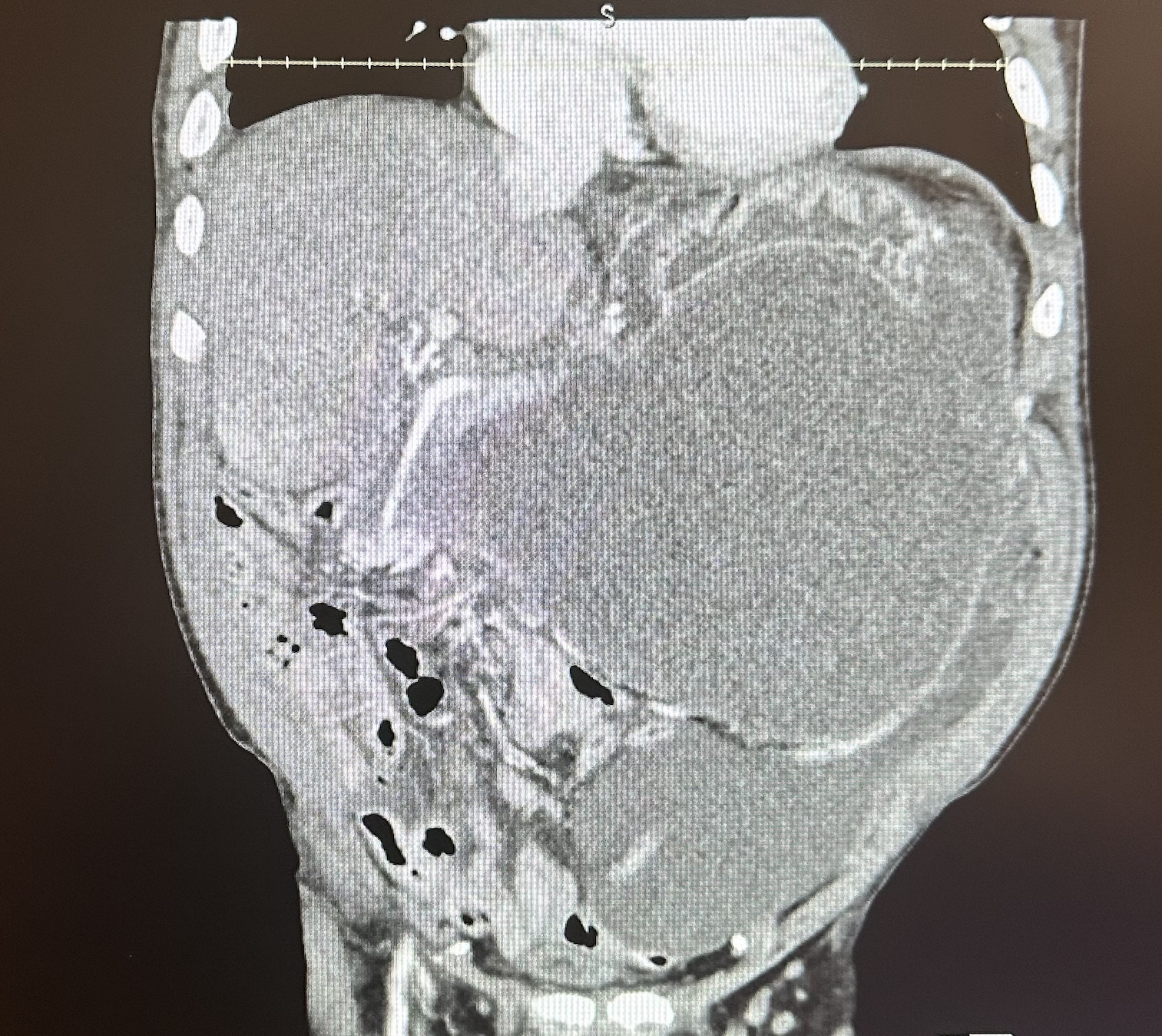
Figure: Contrast enhanced computed tomography showing 8.5 x 23.5 x 18.4 cm large cystic pancreatic mass with mild mural enhancement and septation, compressing stomach.
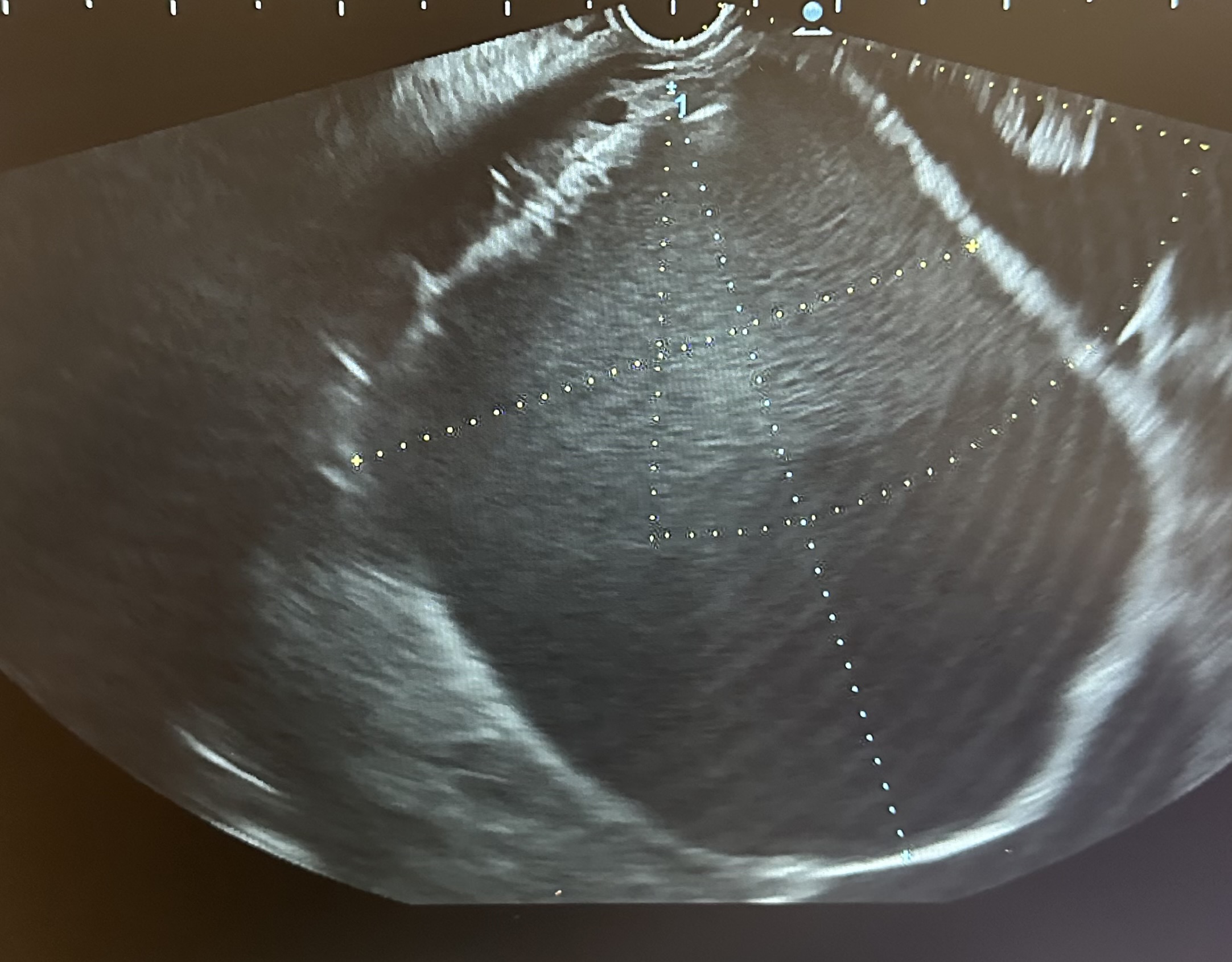
Figure: Endosonography showing large dominant pancreatic cyst measuring 89 mm x 80 mm.
Disclosures:
Edward Cay indicated no relevant financial relationships.
Austin Tiesenga indicated no relevant financial relationships.
Stephen Simmer indicated no relevant financial relationships.
Edward Cay, DO1, Austin Tiesenga, DO2, Stephen Simmer, MD3. P2329 - Gastric Outlet Obstruction due to Pancreatic Serous Cystadenoma Relieved by Endoscopic Cystgastrostomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mclaren Greater Lansing / Michigan State University, Lansing, MI; 2Corewell Health Lakeland, St. Joseph, MI; 3Corewell Health Grand Rapids, Grand Rapids, MI
Introduction: Pancreatic serous cystadenomas (SCAs) are typically benign asymptomatic lesions, incidentally found on cross-sectional imaging. We present a patient who underwent endoscopic ultrasound (EUS) guided cystgastrostomy for large SCA compressing the stomach causing gastric outlet obstruction.
Case Description/
Methods: A 56 year-old man with a past medical history of membranous glomerulonephritis on hemodialysis and chronic hepatitis C cirrhosis, presented with worsening painful abdominal distension for two weeks and weight loss due to early satiety. Contrast enhanced computed tomography showed a 23 cm pancreatic cystic structure with mass effect on the greater curvature of the stomach.
Endosonography demonstrated a large abdominal cyst with multiple septations, and fine needle aspiration showed CEA 1.5 ng/mL, amylase 37 U/L and paucicellular cytology suggestive of serous cystadenoma. Patient was deemed too high risk for surgery given multiple comorbidities, and underwent 2.6 L palliative drainage by interventional radiology (IR) with improvement of symptoms.
Given several recurrences over the past several months despite drainages by IR, the patient was readmitted. EUS-guided cystgastrostomy was performed on the dominant cystic lesion, with 1.5 L serous fluid drained and a lumen apposing metal stent (LAMS) placed with double pigtail stents. Repeat endoscopy two months later showed the cyst cavity with a small amount of debris, removal of LAMS and replacement of double pigtail stents to maintain drainage, which patient tolerated well.
Discussion: Pancreatic serous cystadenomas classically have a honeycomb appearance on imaging, and a pathognomonic “sunburst” central scar calcification. Fluid is usually bloody with low viscosity, low CEA and low amylase levels.
Typically less than 4 cm in size, if these lesions growth larger it may become symptomatic from mass effect, including abdominal distension and gastric outlet obstruction, as seen with our patient. Surgical management for symptomatic patients typically results in no recurrence.
While our patient had rapid reaccumulation of an extremely large SCA causing gastric outlet obstruction, his surgical candidacy was limited. This case highlights EUS guided cystgastrostomy as an alternative to surgical management to symptomatic pancreatic cystadenomas.
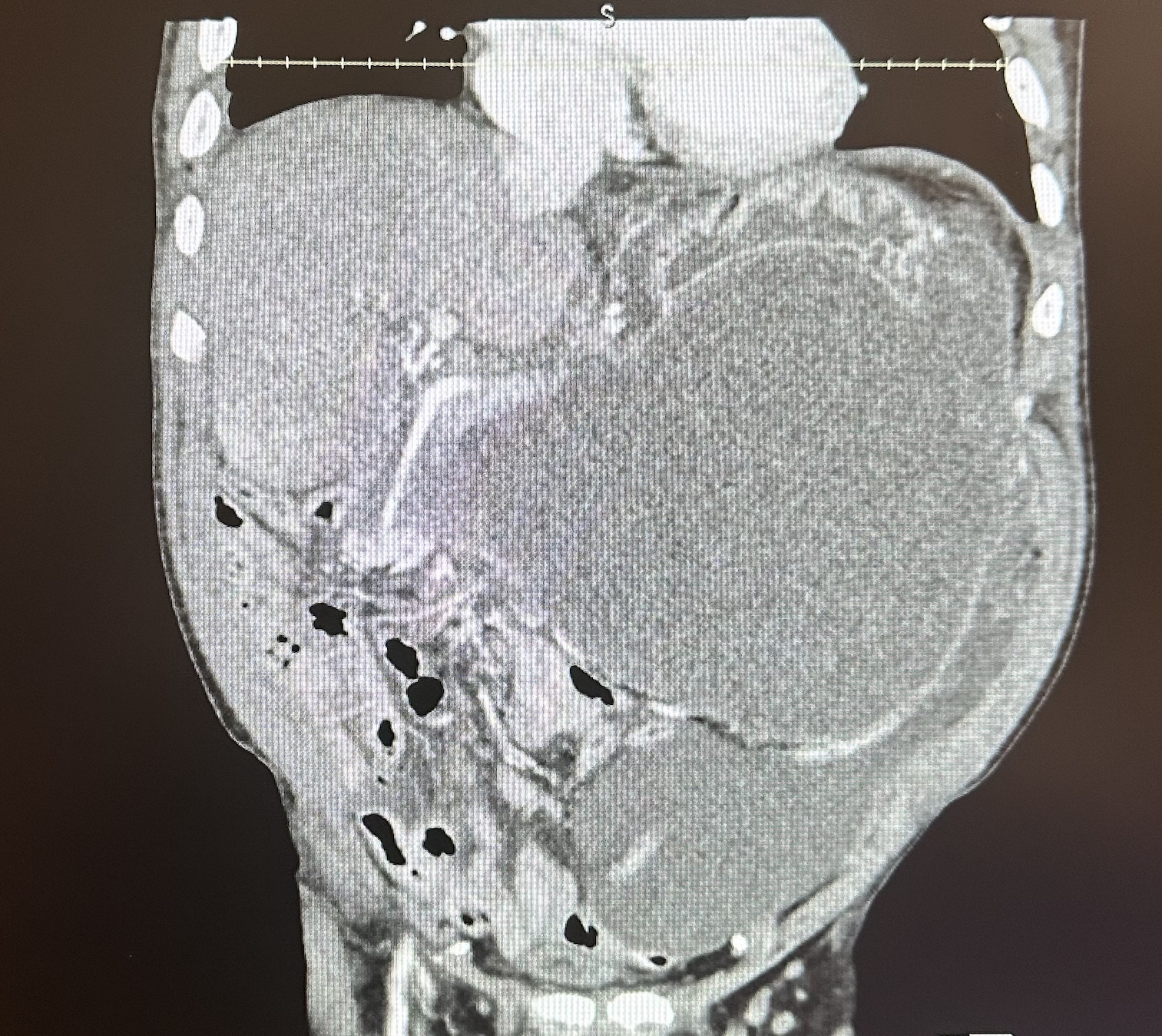
Figure: Contrast enhanced computed tomography showing 8.5 x 23.5 x 18.4 cm large cystic pancreatic mass with mild mural enhancement and septation, compressing stomach.
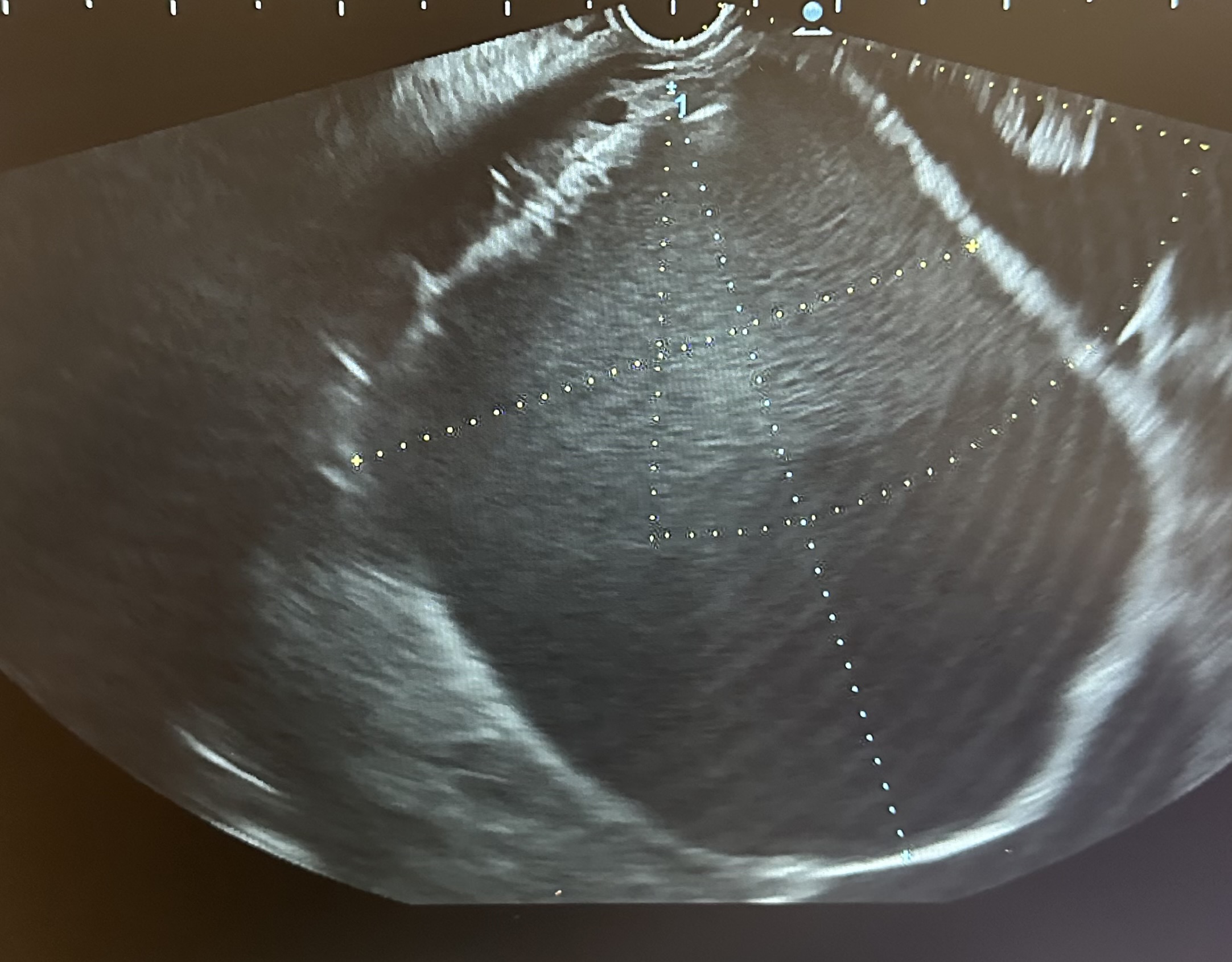
Figure: Endosonography showing large dominant pancreatic cyst measuring 89 mm x 80 mm.
Disclosures:
Edward Cay indicated no relevant financial relationships.
Austin Tiesenga indicated no relevant financial relationships.
Stephen Simmer indicated no relevant financial relationships.
Edward Cay, DO1, Austin Tiesenga, DO2, Stephen Simmer, MD3. P2329 - Gastric Outlet Obstruction due to Pancreatic Serous Cystadenoma Relieved by Endoscopic Cystgastrostomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
