Monday Poster Session
Category: Biliary/Pancreas
P2326 - Necrotizing Pancreatitis: A Large Pseudocyst With Deadly Mass Effect
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Joanna Yuen, DO, MA (she/her/hers)
Ochsner Health Clinic Foundation
Presenting Author(s)
Joanna Yuen, DO, MA, James Gore, DO, Kelley Hill, MD
Ochsner Health Clinic Foundation, New Orleans, LA
Introduction: Pancreatic pseudocysts are encapsulated collections of homogeneous fluid in or around the pancreas. Most resolve spontaneously or are treated supportively. Necrotizing pseudocysts are rare, yet severe complications of acute pancreatitis typically treated with minimally invasive endoscopic drainage. This case highlights the critical course of an adult male who succumbed to the development of a large necrotizing pseudocyst despite an aggressive but unconventional approach to management.
Case Description/
Methods: A 28-year-old man with a history of alcoholic pancreatitis presented with four days of worsening epigastric pain and ascites. He was tachycardic, hypotensive, and jaundiced. His lipase was 75, aspartate transaminase 207, alanine transaminase 59, alkaline phosphatase 536, total bilirubin 13 (direct 8), ammonia 87, albumin 1.6, lactate dehydrogenase 705, lactic acid 5, and leukocyte count 13. Abdominal computed tomography (CT) demonstrated acute pancreatitis, questionable peripancreatic infiltration, and a large adjacent cystic mass with significant mass effect.
Fluids, antibiotics, and pressors were started. Course was complicated by pulseless electrical activity, requiring intubation. Advanced Endoscopy (AES) was unavailable for emergent transgastric drainage at the time. In an attempt to achieve source control and alleviate mass effect, percutaneous bedside pseudocyst drainage was performed, removing 3 L of cola-colored ascitic fluid. Blood cultures and fluid cultures were negative for organismal growth.
Subsequent AES intervention revealed peritoneal ascites and a pseudocyst larger than 120 mm. A cystogastrostomy was performed with initial improvement. Clinical status, however, declined due to fluid reaccumulation and worsening shock. A second bedside paracentesis removed an additional 2.5 L. Despite aggressive management, the patient developed severe acidosis with multi-organ failure. Family opted for comfort care and the patient passed away.
Discussion: Alcohol-induced pancreatitis is associated with an increased risk of pseudocyst development and necrosis. Given his multi-organ failure and untimely death, the patient’s clinical picture strongly suggests necrotizing pancreatitis. Large pseudocysts can cause detrimental mass effects on adjacent organs, and less common approaches like percutaneous drainage may be performed as a temporizing measure to improve clinical status. As seen in this case, early identification of these complications can be critical to management.
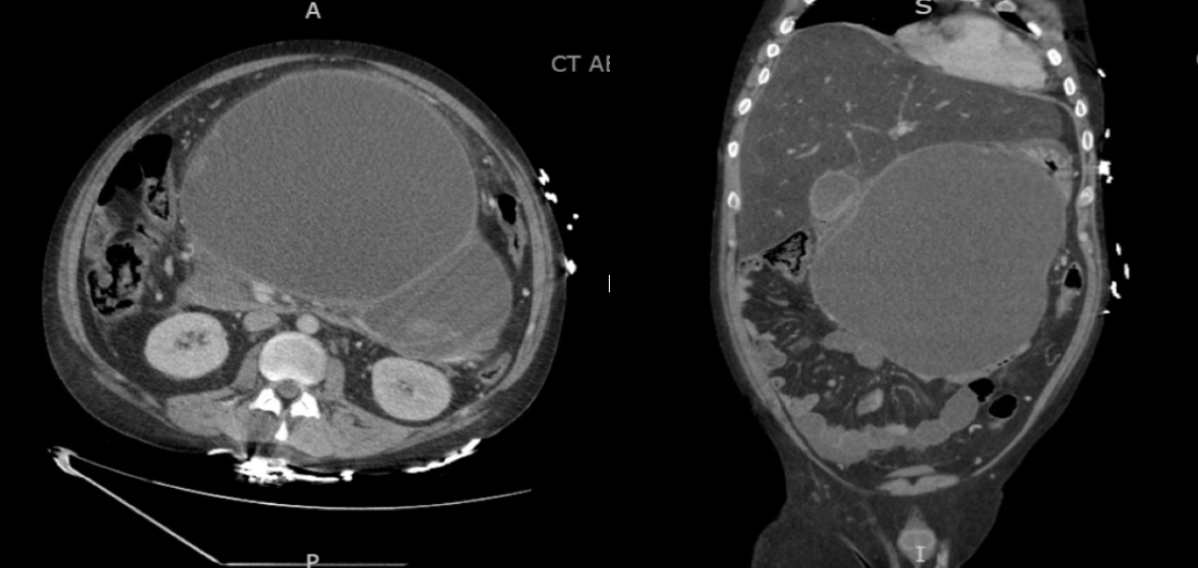
Figure: Figure 1. CT scan of the abdomen and pelvis demonstrating a large cystic abdominal mass adjacent to the pancreas, measuring 16 x 24 x 24 cm with significant mass effect on the stomach.
Disclosures:
Joanna Yuen indicated no relevant financial relationships.
James Gore indicated no relevant financial relationships.
Kelley Hill indicated no relevant financial relationships.
Joanna Yuen, DO, MA, James Gore, DO, Kelley Hill, MD. P2326 - Necrotizing Pancreatitis: A Large Pseudocyst With Deadly Mass Effect, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Ochsner Health Clinic Foundation, New Orleans, LA
Introduction: Pancreatic pseudocysts are encapsulated collections of homogeneous fluid in or around the pancreas. Most resolve spontaneously or are treated supportively. Necrotizing pseudocysts are rare, yet severe complications of acute pancreatitis typically treated with minimally invasive endoscopic drainage. This case highlights the critical course of an adult male who succumbed to the development of a large necrotizing pseudocyst despite an aggressive but unconventional approach to management.
Case Description/
Methods: A 28-year-old man with a history of alcoholic pancreatitis presented with four days of worsening epigastric pain and ascites. He was tachycardic, hypotensive, and jaundiced. His lipase was 75, aspartate transaminase 207, alanine transaminase 59, alkaline phosphatase 536, total bilirubin 13 (direct 8), ammonia 87, albumin 1.6, lactate dehydrogenase 705, lactic acid 5, and leukocyte count 13. Abdominal computed tomography (CT) demonstrated acute pancreatitis, questionable peripancreatic infiltration, and a large adjacent cystic mass with significant mass effect.
Fluids, antibiotics, and pressors were started. Course was complicated by pulseless electrical activity, requiring intubation. Advanced Endoscopy (AES) was unavailable for emergent transgastric drainage at the time. In an attempt to achieve source control and alleviate mass effect, percutaneous bedside pseudocyst drainage was performed, removing 3 L of cola-colored ascitic fluid. Blood cultures and fluid cultures were negative for organismal growth.
Subsequent AES intervention revealed peritoneal ascites and a pseudocyst larger than 120 mm. A cystogastrostomy was performed with initial improvement. Clinical status, however, declined due to fluid reaccumulation and worsening shock. A second bedside paracentesis removed an additional 2.5 L. Despite aggressive management, the patient developed severe acidosis with multi-organ failure. Family opted for comfort care and the patient passed away.
Discussion: Alcohol-induced pancreatitis is associated with an increased risk of pseudocyst development and necrosis. Given his multi-organ failure and untimely death, the patient’s clinical picture strongly suggests necrotizing pancreatitis. Large pseudocysts can cause detrimental mass effects on adjacent organs, and less common approaches like percutaneous drainage may be performed as a temporizing measure to improve clinical status. As seen in this case, early identification of these complications can be critical to management.
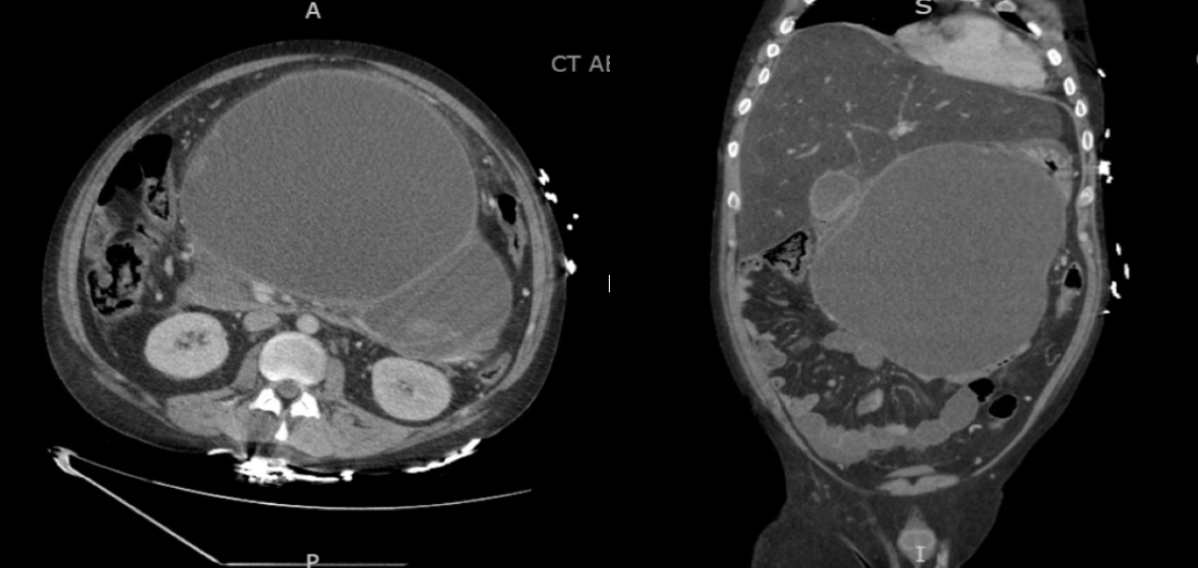
Figure: Figure 1. CT scan of the abdomen and pelvis demonstrating a large cystic abdominal mass adjacent to the pancreas, measuring 16 x 24 x 24 cm with significant mass effect on the stomach.
Disclosures:
Joanna Yuen indicated no relevant financial relationships.
James Gore indicated no relevant financial relationships.
Kelley Hill indicated no relevant financial relationships.
Joanna Yuen, DO, MA, James Gore, DO, Kelley Hill, MD. P2326 - Necrotizing Pancreatitis: A Large Pseudocyst With Deadly Mass Effect, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
