Monday Poster Session
Category: Biliary/Pancreas
P2319 - A Rare Case of a Symptomatic Choledochocolonic Fistula With Concomitant Gallbladder Agenesis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Christina Joya, DO
Valley Hospital Medical Center
Las Vegas, NV
Presenting Author(s)
Christina Joya, DO1, Renuka Verma, MD2, Sara Alleyasin, DO3, Scott Silver, DO1, Vishvinder Sharma, MD1
1Valley Hospital Medical Center, Las Vegas, NV; 2Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, Las Vegas, NV; 3Valley Health System, Las Vegas, NV
Introduction: Bilioenteric fistulas (BEFs) are an uncommon complication of chronic gallstone disease, occurring in approximately 1% of patients with biliary disease. Choledochocolonic fistulas (CDCFs) are an exceedingly rare subtype with few documented cases. Gallbladder agenesis (GA) is a separate rare anomaly with an estimated incidence of 0.01-0.05%. We present a case of a patient with a CDCF and concomitant GA presenting with choledocholithiasis.
Case Description/
Methods: A 72-year-old female presented with jaundice, epigastric abdominal pain, nausea, and nonbilious, nonbloody vomiting. Labs on arrival were significant for total bilirubin 11.5 mg/dl, alkaline phosphatase 1337 IU/L, AST 306 U/L, and ALT 331 U/L. A CT abdomen pelvis without contrast showed severe biliary dilation with the common bile duct (CBD) measuring 11 mm, extensive pneumobilia, choledocholithiasis, and an absent gallbladder. The patient reported no history of cholecystectomy. The patient underwent endoscopic retrograde cholangiopancreatography ( ERCP) with sphincterotomy and endoscopic ultrasound (EUS). The cholangiogram showed CBD dilation with multiple stones and pus. The stones were removed with a 15 mm extraction balloon. A diagnostic laparoscopy was performed, but the gallbladder was not visualized, and no biliary structures were illuminated during the intraoperative cholangiography.
The surgery was aborted due to significant adhesions between the liver and transverse colon. Subsequent MRI abdomen with and without contrast showed a fistula between the biliary tree and hepatic flexure with no identifiable gallbladder. Colonoscopy confirmed a fistulous opening 50 cm from the anal verge.
Discussion: In current literature, very few cases of BEFs occurring in patients with GA have been documented. BEFs can develop secondary to long-standing inflammation and pressure on surrounding tissue from gallstones, causing erosion. GA is associated with the development of choledocholithiasis, likely due to increased basal pressure in the sphincter of Oddi. In this patient, chronic gallstone disease in the setting of GA ultimately resulted in the formation of the CDCF. Failure to diagnose BEFs may lead to increased complications, including septic shock from cholangitis and colonic perforations. While surgery is the mainstay of diagnosis and treatment, colonoscopy may be helpful for evaluation in cases where diagnosis is unclear. Recognizing the potential for developing BEFs in patients with GA is essential.
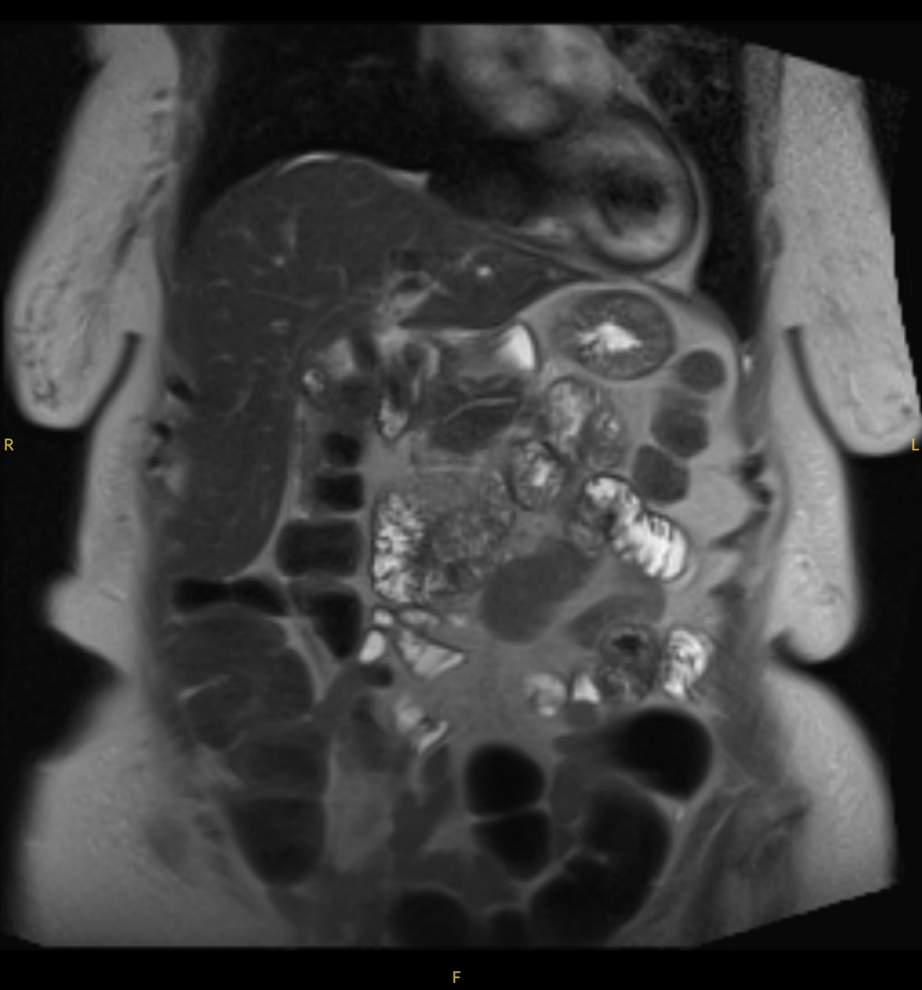
Figure: MRI abdomen with and without contrast showing a fistula between the biliary tree and hepatic flexure.
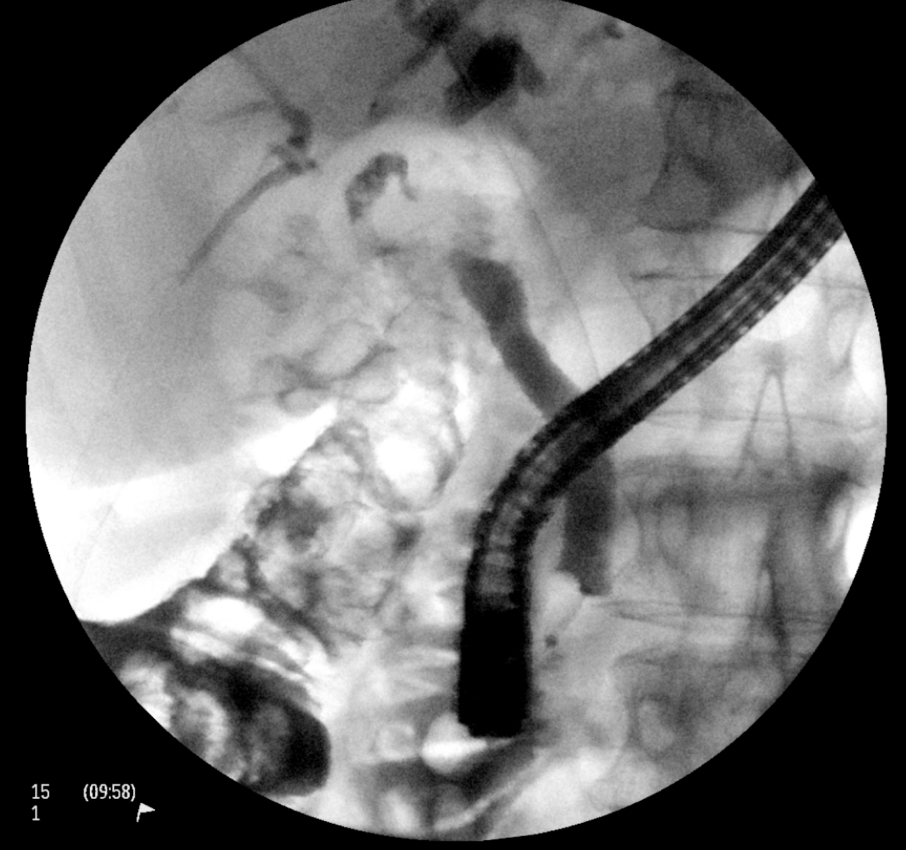
Figure: Cholangiogram showing a fistula tract between the biliary tract and adjacent colon.
Disclosures:
Christina Joya indicated no relevant financial relationships.
Renuka Verma indicated no relevant financial relationships.
Sara Alleyasin indicated no relevant financial relationships.
Scott Silver indicated no relevant financial relationships.
Vishvinder Sharma indicated no relevant financial relationships.
Christina Joya, DO1, Renuka Verma, MD2, Sara Alleyasin, DO3, Scott Silver, DO1, Vishvinder Sharma, MD1. P2319 - A Rare Case of a Symptomatic Choledochocolonic Fistula With Concomitant Gallbladder Agenesis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Valley Hospital Medical Center, Las Vegas, NV; 2Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, Las Vegas, NV; 3Valley Health System, Las Vegas, NV
Introduction: Bilioenteric fistulas (BEFs) are an uncommon complication of chronic gallstone disease, occurring in approximately 1% of patients with biliary disease. Choledochocolonic fistulas (CDCFs) are an exceedingly rare subtype with few documented cases. Gallbladder agenesis (GA) is a separate rare anomaly with an estimated incidence of 0.01-0.05%. We present a case of a patient with a CDCF and concomitant GA presenting with choledocholithiasis.
Case Description/
Methods: A 72-year-old female presented with jaundice, epigastric abdominal pain, nausea, and nonbilious, nonbloody vomiting. Labs on arrival were significant for total bilirubin 11.5 mg/dl, alkaline phosphatase 1337 IU/L, AST 306 U/L, and ALT 331 U/L. A CT abdomen pelvis without contrast showed severe biliary dilation with the common bile duct (CBD) measuring 11 mm, extensive pneumobilia, choledocholithiasis, and an absent gallbladder. The patient reported no history of cholecystectomy. The patient underwent endoscopic retrograde cholangiopancreatography ( ERCP) with sphincterotomy and endoscopic ultrasound (EUS). The cholangiogram showed CBD dilation with multiple stones and pus. The stones were removed with a 15 mm extraction balloon. A diagnostic laparoscopy was performed, but the gallbladder was not visualized, and no biliary structures were illuminated during the intraoperative cholangiography.
The surgery was aborted due to significant adhesions between the liver and transverse colon. Subsequent MRI abdomen with and without contrast showed a fistula between the biliary tree and hepatic flexure with no identifiable gallbladder. Colonoscopy confirmed a fistulous opening 50 cm from the anal verge.
Discussion: In current literature, very few cases of BEFs occurring in patients with GA have been documented. BEFs can develop secondary to long-standing inflammation and pressure on surrounding tissue from gallstones, causing erosion. GA is associated with the development of choledocholithiasis, likely due to increased basal pressure in the sphincter of Oddi. In this patient, chronic gallstone disease in the setting of GA ultimately resulted in the formation of the CDCF. Failure to diagnose BEFs may lead to increased complications, including septic shock from cholangitis and colonic perforations. While surgery is the mainstay of diagnosis and treatment, colonoscopy may be helpful for evaluation in cases where diagnosis is unclear. Recognizing the potential for developing BEFs in patients with GA is essential.
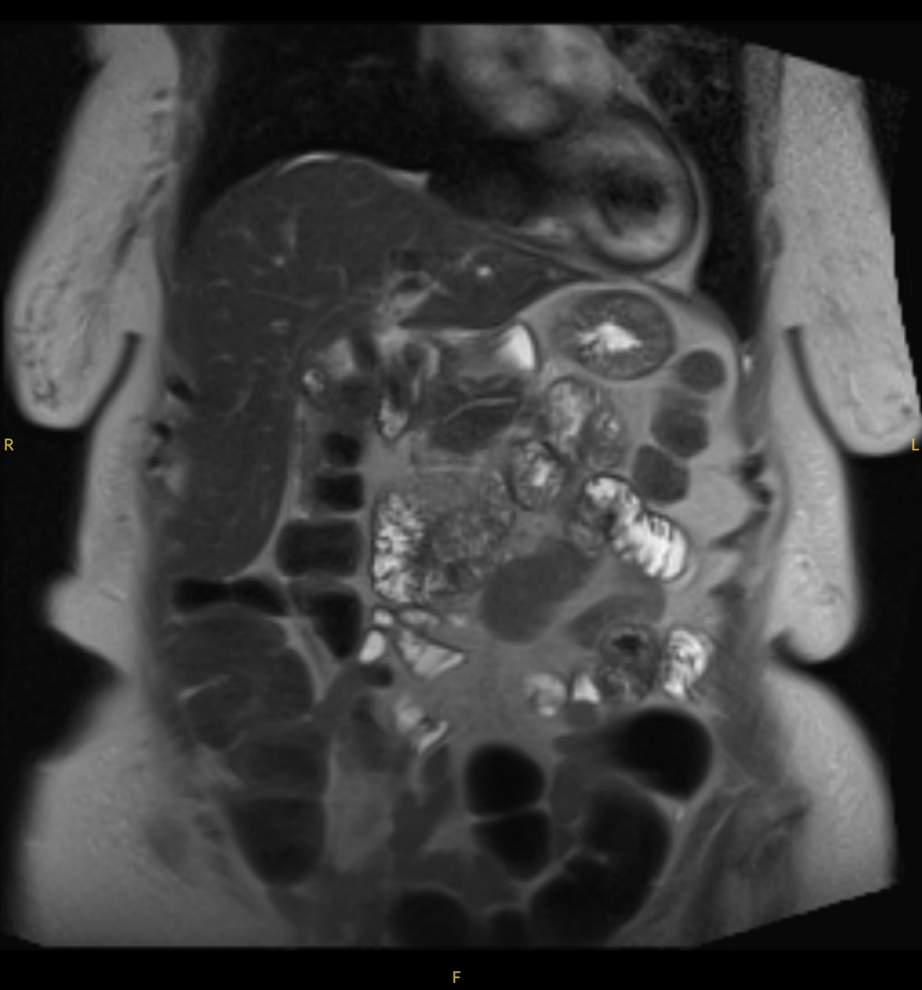
Figure: MRI abdomen with and without contrast showing a fistula between the biliary tree and hepatic flexure.
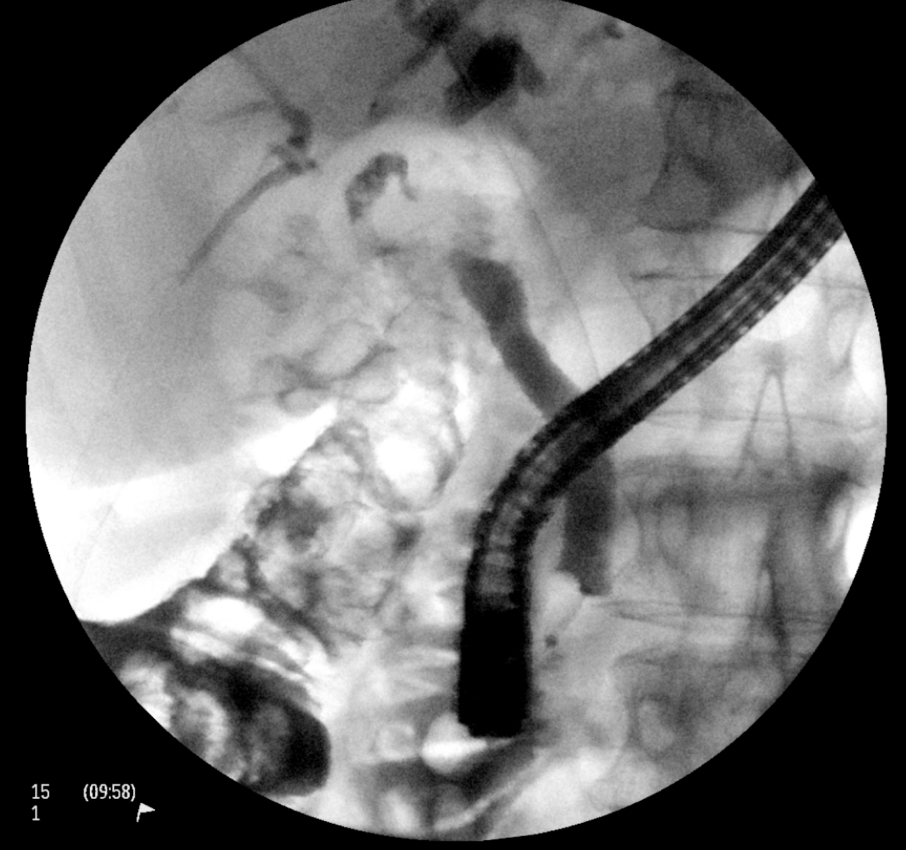
Figure: Cholangiogram showing a fistula tract between the biliary tract and adjacent colon.
Disclosures:
Christina Joya indicated no relevant financial relationships.
Renuka Verma indicated no relevant financial relationships.
Sara Alleyasin indicated no relevant financial relationships.
Scott Silver indicated no relevant financial relationships.
Vishvinder Sharma indicated no relevant financial relationships.
Christina Joya, DO1, Renuka Verma, MD2, Sara Alleyasin, DO3, Scott Silver, DO1, Vishvinder Sharma, MD1. P2319 - A Rare Case of a Symptomatic Choledochocolonic Fistula With Concomitant Gallbladder Agenesis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
