Monday Poster Session
Category: Biliary/Pancreas
P2264 - When IgG4-Related Disease Mimics Metastatic Cancer: A Case of Recurrent Pancreatitis with Mass-Forming Lesions
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- OA
Omar Alwan, MD
Hamilton Medical Center
Dalton, GA
Presenting Author(s)
Omar Alwan, MD1, Mohamed Alharami, MD2, Frhaan Zahrawi, MBBCh3, Hadi Hemaidan, MS4, Ziad Suleiman, MD5
1Hamilton Medical Center, Dalton, GA; 2Henry Ford Warren, Warren, MI; 3Franciscan Health Olympia Fields, Olympia Fields, IL; 4Florida International University, Daytona Beach, FL; 5Southwest healthcare medical education consortium, Murrieta, CA
Introduction: Immunoglobulin G4-related disease (IgG4-RD) is a systemic, immune-mediated fibroinflammatory disorder characterized by tumefactive lesions, storiform fibrosis, and lymphoplasmacytic infiltrates with an abundance of IgG4-positive plasma cells. The wide range of clinical presentations, multi-organ involvement, and tendency to mimic malignancies increase the complexity of diagnosis. Autoimmune pancreatitis (AIP), particularly type 1, is a prototypical manifestation of IgG4-RD, which can present as a pancreatic mass mimicking pancreatic cancer. To date, histopathology remains the only definitive method for differentiating IgG4-RD lesions from malignancy, and the fact that patients can continually develop and present with newly formed masses leads to a vicious cycle of diagnostic dilemmas and unnecessary invasive procedures.
Case Description/
Methods: A 59-year-old woman presented with abdominal pain. She had a history of multiple emergency department visits for similar episodes, previously diagnosed as idiopathic pancreatitis. CT imaging revealed multiple ill-defined pancreatic and hepatic lesions, as well as enlarged axillary and paraaortic lymph nodes, raising concern for metastatic disease (Figure 1). Liver and pancreatic biopsies were non-diagnostic but showed atypical lymphocytic infiltrates and fibrosclerotic tissue. Flow cytometry ruled out lymphoproliferative disease. Given the clinical context, she was empirically started on corticosteroids for a presumed diagnosis of IgG4-RD. However, shortly thereafter, new bilateral renal lesions, a pleural nodule, a thyroid nodule, and retroperitoneal stranding were detected, once again raising concern for metastatic disease and prompting renewed diagnostic investigation (Figure 1). A repeat liver biopsy demonstrated a lymphoplasmacytic infiltrate with polytypic plasma cells, consistent with IgG4-RD. Clonality was excluded by a repeat flow cytometry and BIOMED-2 PCR. The patient was discharged on corticosteroids, with plans to start a steroid-sparing immunosuppressant therapy.
Discussion: IgG4-RD shares clinical and radiological features with metastatic cancer. Clinicians face significant challenges in weighing the benefits versus the risks of ordering invasive, yet potentially diagnostic, procedures. IgG4-RD responds well to corticosteroid therapy; thus, early recognition and treatment are key to preventing irreversible organ damage and avoiding unwarranted invasive interventions.
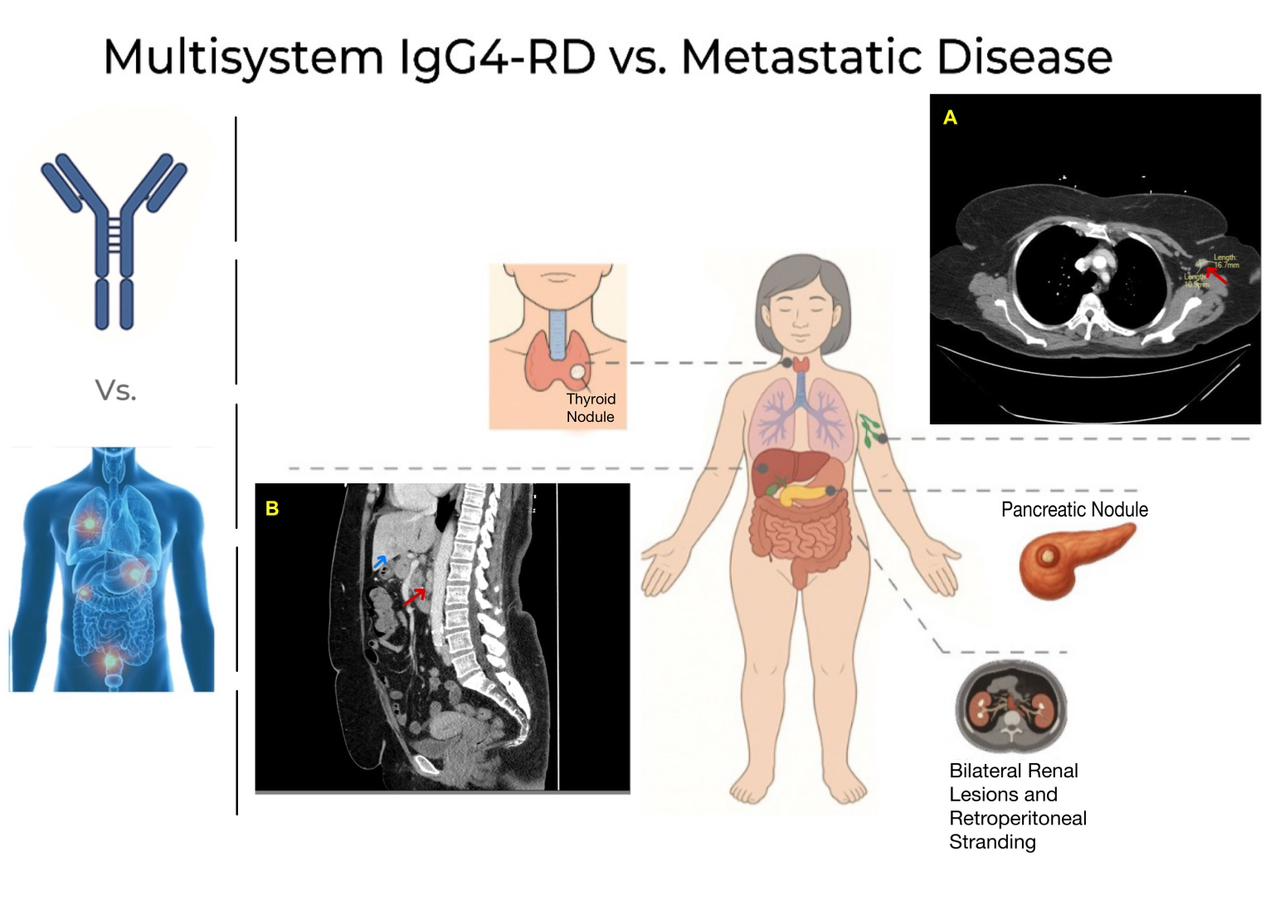
Figure: (A) Axial chest CT image showing a right axillary lymphadenopathy (red arrow).
(B) Sagittal abdominal CT image demonstrating para-aortic lymphadenopathy (red arrow) and an ill-defined hepatic lesion (blue arrow).
The central illustration maps associated findings including a thyroid nodule, pancreatic nodule, and bilateral renal lesions with retroperitoneal stranding.
Disclosures:
Omar Alwan indicated no relevant financial relationships.
Mohamed Alharami indicated no relevant financial relationships.
Frhaan Zahrawi indicated no relevant financial relationships.
Hadi Hemaidan indicated no relevant financial relationships.
Ziad Suleiman indicated no relevant financial relationships.
Omar Alwan, MD1, Mohamed Alharami, MD2, Frhaan Zahrawi, MBBCh3, Hadi Hemaidan, MS4, Ziad Suleiman, MD5. P2264 - When IgG4-Related Disease Mimics Metastatic Cancer: A Case of Recurrent Pancreatitis with Mass-Forming Lesions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Hamilton Medical Center, Dalton, GA; 2Henry Ford Warren, Warren, MI; 3Franciscan Health Olympia Fields, Olympia Fields, IL; 4Florida International University, Daytona Beach, FL; 5Southwest healthcare medical education consortium, Murrieta, CA
Introduction: Immunoglobulin G4-related disease (IgG4-RD) is a systemic, immune-mediated fibroinflammatory disorder characterized by tumefactive lesions, storiform fibrosis, and lymphoplasmacytic infiltrates with an abundance of IgG4-positive plasma cells. The wide range of clinical presentations, multi-organ involvement, and tendency to mimic malignancies increase the complexity of diagnosis. Autoimmune pancreatitis (AIP), particularly type 1, is a prototypical manifestation of IgG4-RD, which can present as a pancreatic mass mimicking pancreatic cancer. To date, histopathology remains the only definitive method for differentiating IgG4-RD lesions from malignancy, and the fact that patients can continually develop and present with newly formed masses leads to a vicious cycle of diagnostic dilemmas and unnecessary invasive procedures.
Case Description/
Methods: A 59-year-old woman presented with abdominal pain. She had a history of multiple emergency department visits for similar episodes, previously diagnosed as idiopathic pancreatitis. CT imaging revealed multiple ill-defined pancreatic and hepatic lesions, as well as enlarged axillary and paraaortic lymph nodes, raising concern for metastatic disease (Figure 1). Liver and pancreatic biopsies were non-diagnostic but showed atypical lymphocytic infiltrates and fibrosclerotic tissue. Flow cytometry ruled out lymphoproliferative disease. Given the clinical context, she was empirically started on corticosteroids for a presumed diagnosis of IgG4-RD. However, shortly thereafter, new bilateral renal lesions, a pleural nodule, a thyroid nodule, and retroperitoneal stranding were detected, once again raising concern for metastatic disease and prompting renewed diagnostic investigation (Figure 1). A repeat liver biopsy demonstrated a lymphoplasmacytic infiltrate with polytypic plasma cells, consistent with IgG4-RD. Clonality was excluded by a repeat flow cytometry and BIOMED-2 PCR. The patient was discharged on corticosteroids, with plans to start a steroid-sparing immunosuppressant therapy.
Discussion: IgG4-RD shares clinical and radiological features with metastatic cancer. Clinicians face significant challenges in weighing the benefits versus the risks of ordering invasive, yet potentially diagnostic, procedures. IgG4-RD responds well to corticosteroid therapy; thus, early recognition and treatment are key to preventing irreversible organ damage and avoiding unwarranted invasive interventions.
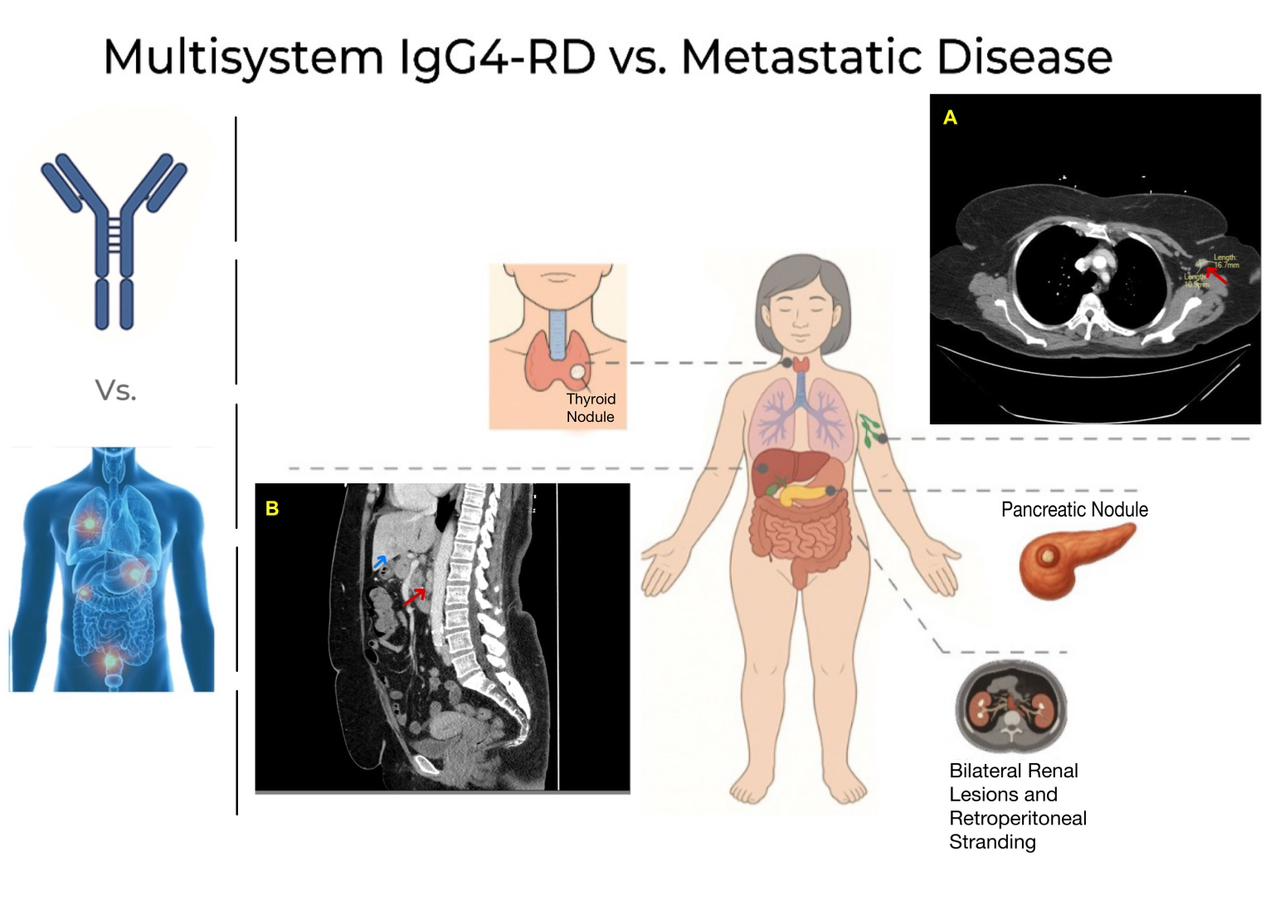
Figure: (A) Axial chest CT image showing a right axillary lymphadenopathy (red arrow).
(B) Sagittal abdominal CT image demonstrating para-aortic lymphadenopathy (red arrow) and an ill-defined hepatic lesion (blue arrow).
The central illustration maps associated findings including a thyroid nodule, pancreatic nodule, and bilateral renal lesions with retroperitoneal stranding.
Disclosures:
Omar Alwan indicated no relevant financial relationships.
Mohamed Alharami indicated no relevant financial relationships.
Frhaan Zahrawi indicated no relevant financial relationships.
Hadi Hemaidan indicated no relevant financial relationships.
Ziad Suleiman indicated no relevant financial relationships.
Omar Alwan, MD1, Mohamed Alharami, MD2, Frhaan Zahrawi, MBBCh3, Hadi Hemaidan, MS4, Ziad Suleiman, MD5. P2264 - When IgG4-Related Disease Mimics Metastatic Cancer: A Case of Recurrent Pancreatitis with Mass-Forming Lesions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
