Monday Poster Session
Category: Biliary/Pancreas
P2257 - IgG4-Related Cholangitis and Autoimmune Pancreatitis Presenting With Weight Loss
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Venkat Arutla, MD
Rochester General Hospital
Rochester, NY
Presenting Author(s)
Venkat Arutla, MD1, Ese Uwagbale, MD2, Mark S. McFarland, MD, MSc3, Jason Gutman, MD4, Karin Dunnigan, MD1
1Rochester General Hospital, Rochester, NY; 2Rochester General Hospital, Webster, NY; 3Rochester General Hospital, Pittsford, NY; 4rochester general hospital, Rochester, NY
Introduction: IgG4-related disease is an immune-mediated disease that can involve the pancreas and biliary tract. It is characterized by non-specific symptoms, including abdominal pain and weight loss. We present a case of IgG 4-related cholangitis and autoimmune pancreatitis presenting with weight loss.
Case Description/
Methods: A 72-year-old man with a past medical history of Systemic Lupus Erythematosus (SLE) well controlled with hydroxychloroquine presented with 30 pounds of unintentional weight loss over 4 months and new onset dysphagia to solids. Labs showed newly elevated liver function tests (LFTs) with peak values of total bilirubin 1.4, aspartate aminotransferase of 133 U/L (0-34 U/L), alanine aminotransferase of 160 U/L (10-49 U/L) and alkaline phosphatase of 639 U/L (46-116 U/L). Computed tomography (CT) of the abdomen and pelvis revealed mild to moderate intrahepatic biliary dilation with a minimal 8 mm dilation of the common bile duct (CBD). However, the CBD was noted to have an age-indeterminate thick enhancing wall concerning cholangitis. The patient subsequently underwent magnetic resonance cholangiopancreatography (MRCP), which showed diffusely low T1 signal with delayed enhancement of the pancreas with a slightly enlarged tail compared to the head, obscured pancreatic duct, and loss of normal lobular architecture (Figure 1). These findings suggest IgG-4 disease-related pancreatitis.
Esophagogastroduodenoscopy (EGD) showed Los Angeles (LA) grade A esophagitis. Endoscopic ultrasound showed enlarged sausage-shaped parenchyma of the body and tail of the pancreas, suggestive of autoimmune pancreatitis and abnormal appearing common hepatic and CBD with thickened wall (Figure 2), measuring 3.6 mm. The lumen of the bile duct measured 3.1 mm. Further serum analysis revealed elevated Total IgG of 2043 mg/dL (767-1590 mg/dL) and elevated IgG subclass 4 of 529 mg/dL (2.4-121 mg/dL). The patient was started on prednisone 40 mg daily for 6 weeks with improved IgG4 from 529.9 to 206.7, LFTs normalized, and follow-up MRCP showed improvement in previous findings. He was then tapered off prednisone with the initiation of rituximab infusion by Rheumatology due to persistent elevation of IgG4 with weight gain and improvement in his symptoms.
Discussion: IgG 4-related disease is an important differential diagnosis for weight loss, especially in a patient with underlying autoimmune disease. An accurate diagnosis can be made using a combination of imaging, radiologic, and sometimes histological findings.
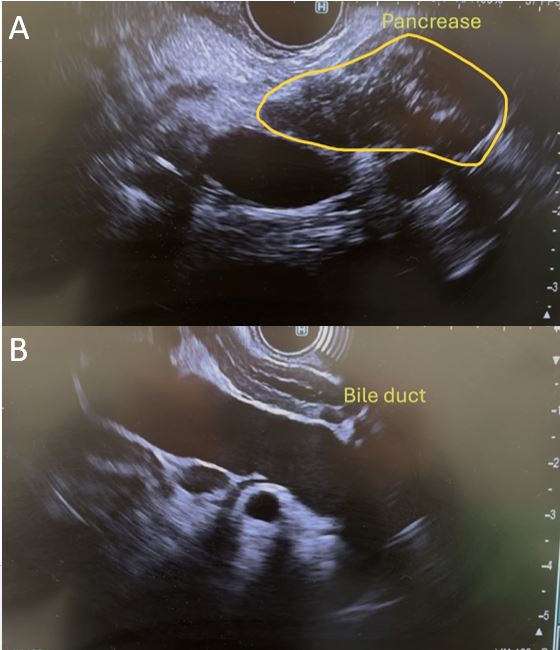
Figure: Figure 1: MRCP of intrahepatic ducts (A) and pancreas (B) pre-steroids and intrahepatic ducts (C) and pancreas (D) post-steroids.
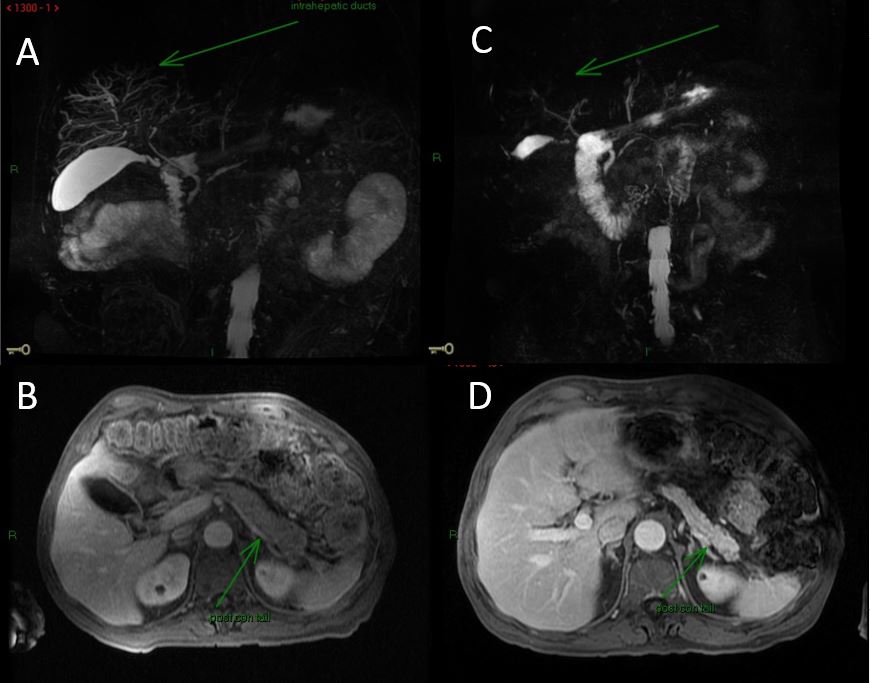
Figure: Figure 2: Endoscopic ultrasound showing enlarged sausage-shaped pancreas (A) and CBD with thickened wall (B).
Disclosures:
Venkat Arutla indicated no relevant financial relationships.
Ese Uwagbale indicated no relevant financial relationships.
Mark McFarland indicated no relevant financial relationships.
Jason Gutman indicated no relevant financial relationships.
Karin Dunnigan indicated no relevant financial relationships.
Venkat Arutla, MD1, Ese Uwagbale, MD2, Mark S. McFarland, MD, MSc3, Jason Gutman, MD4, Karin Dunnigan, MD1. P2257 - IgG4-Related Cholangitis and Autoimmune Pancreatitis Presenting With Weight Loss, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rochester General Hospital, Rochester, NY; 2Rochester General Hospital, Webster, NY; 3Rochester General Hospital, Pittsford, NY; 4rochester general hospital, Rochester, NY
Introduction: IgG4-related disease is an immune-mediated disease that can involve the pancreas and biliary tract. It is characterized by non-specific symptoms, including abdominal pain and weight loss. We present a case of IgG 4-related cholangitis and autoimmune pancreatitis presenting with weight loss.
Case Description/
Methods: A 72-year-old man with a past medical history of Systemic Lupus Erythematosus (SLE) well controlled with hydroxychloroquine presented with 30 pounds of unintentional weight loss over 4 months and new onset dysphagia to solids. Labs showed newly elevated liver function tests (LFTs) with peak values of total bilirubin 1.4, aspartate aminotransferase of 133 U/L (0-34 U/L), alanine aminotransferase of 160 U/L (10-49 U/L) and alkaline phosphatase of 639 U/L (46-116 U/L). Computed tomography (CT) of the abdomen and pelvis revealed mild to moderate intrahepatic biliary dilation with a minimal 8 mm dilation of the common bile duct (CBD). However, the CBD was noted to have an age-indeterminate thick enhancing wall concerning cholangitis. The patient subsequently underwent magnetic resonance cholangiopancreatography (MRCP), which showed diffusely low T1 signal with delayed enhancement of the pancreas with a slightly enlarged tail compared to the head, obscured pancreatic duct, and loss of normal lobular architecture (Figure 1). These findings suggest IgG-4 disease-related pancreatitis.
Esophagogastroduodenoscopy (EGD) showed Los Angeles (LA) grade A esophagitis. Endoscopic ultrasound showed enlarged sausage-shaped parenchyma of the body and tail of the pancreas, suggestive of autoimmune pancreatitis and abnormal appearing common hepatic and CBD with thickened wall (Figure 2), measuring 3.6 mm. The lumen of the bile duct measured 3.1 mm. Further serum analysis revealed elevated Total IgG of 2043 mg/dL (767-1590 mg/dL) and elevated IgG subclass 4 of 529 mg/dL (2.4-121 mg/dL). The patient was started on prednisone 40 mg daily for 6 weeks with improved IgG4 from 529.9 to 206.7, LFTs normalized, and follow-up MRCP showed improvement in previous findings. He was then tapered off prednisone with the initiation of rituximab infusion by Rheumatology due to persistent elevation of IgG4 with weight gain and improvement in his symptoms.
Discussion: IgG 4-related disease is an important differential diagnosis for weight loss, especially in a patient with underlying autoimmune disease. An accurate diagnosis can be made using a combination of imaging, radiologic, and sometimes histological findings.
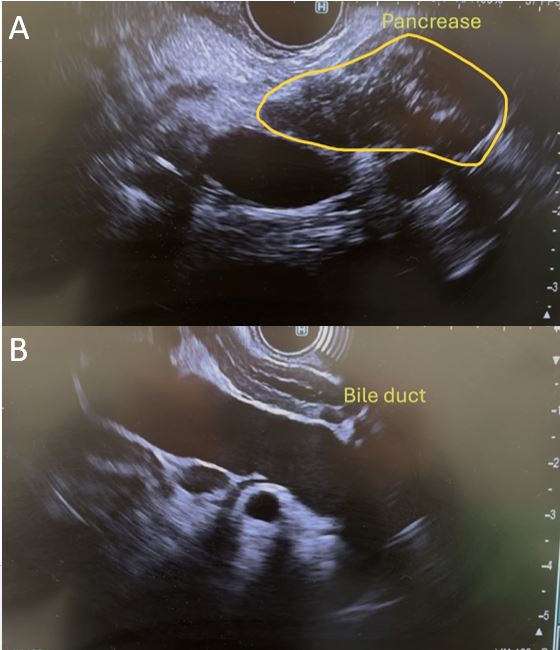
Figure: Figure 1: MRCP of intrahepatic ducts (A) and pancreas (B) pre-steroids and intrahepatic ducts (C) and pancreas (D) post-steroids.
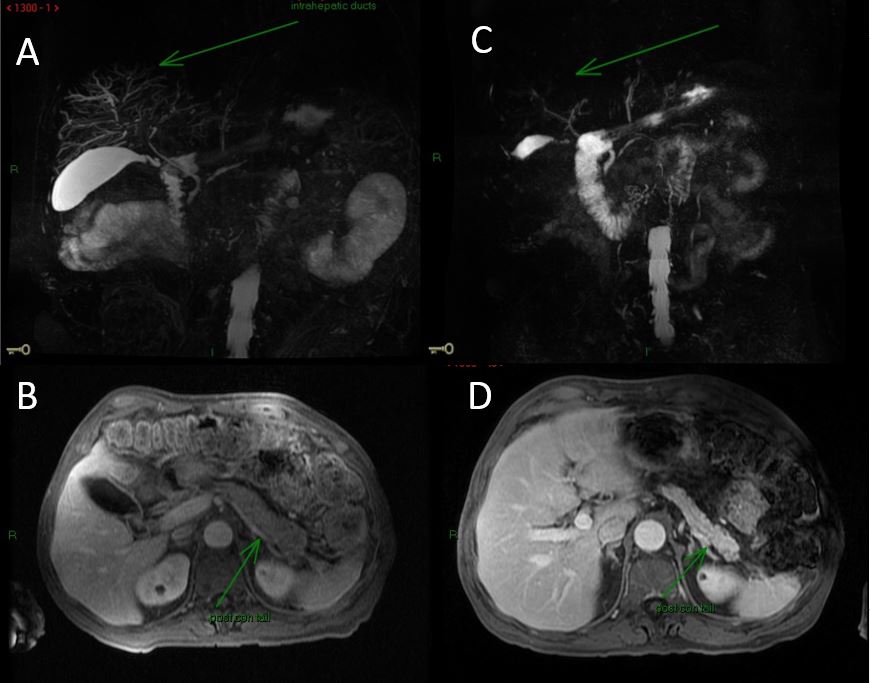
Figure: Figure 2: Endoscopic ultrasound showing enlarged sausage-shaped pancreas (A) and CBD with thickened wall (B).
Disclosures:
Venkat Arutla indicated no relevant financial relationships.
Ese Uwagbale indicated no relevant financial relationships.
Mark McFarland indicated no relevant financial relationships.
Jason Gutman indicated no relevant financial relationships.
Karin Dunnigan indicated no relevant financial relationships.
Venkat Arutla, MD1, Ese Uwagbale, MD2, Mark S. McFarland, MD, MSc3, Jason Gutman, MD4, Karin Dunnigan, MD1. P2257 - IgG4-Related Cholangitis and Autoimmune Pancreatitis Presenting With Weight Loss, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

