Monday Poster Session
Category: Biliary/Pancreas
P2219 - Pancreatic Head Fullness: A Retrospective Study of Diagnostic Pathways and Clinical Outcomes
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ahmad Alkurd, MD
LSU Health Shreveport
Houston, TX
Presenting Author(s)
Omar Khan, MD1, Ahmad Alkurd, MD1, Cole Bourgeois, BS1, Katelyn Foreman, BS1, Erika Lytle, DO2, Brittany Pass, BS1, Connor Plaisance, MD1, Dylan Thompson, BS1, Daniyal Raza, MD1, Qiang Cai, MD, PhD, MACG3
1LSU Health Shreveport, Shreveport, LA; 2Edward Via College of Osteopathic Medicine, Shreveport, LA; 3LSU Health Sciences Center - SHREVEPORT, LA, Shreveport, LA
Introduction: Pancreatic head fullness is an incidental imaging finding often seen on computed tomography (CT) or magnetic resonance imaging (MRI). The lack of standardized guidelines for evaluating this finding creates uncertainty in its management and outcomes. While limited studies, primarily focusing on CT scans, suggest that most cases are benign, the potential for malignancy underscores the need for a systematic approach. This study evaluates the diagnostic workup, outcomes, and management of patients with pancreatic head fullness at a single academic center.
Methods: This retrospective study identified patients through radiology keyword searches for pancreatic head fullness on CT or MRI from January 2020 to March 2024. Data collected included demographics (Table 2), clinical history, EUS with or without fine-needle aspiration (FNA) or biopsy (FNB), tumor markers, final diagnoses (Table 1), and treatments. Patients without definitive diagnoses or those lost to follow-up were excluded from the final analysis. Descriptive statistics summarized the findings.
Results: Among 407 identified patients, 183 (45%) were excluded due to loss to follow-up or absence of further workup. The final analysis comprised 224 patients, with an average age of 59 years; 58% were male and 42% female. The racial distribution was 56% Black, 42% White, and 1% Hispanic. A history of pancreatitis was documented in 39% of patients. 94% of patients reported tobacco or alcohol use. EUS was performed in 48% (n=107), with 78 undergoing FNA/FNB. An elevated CEA level, either from the serum or cystic fluid, or an elevated CA 19-9 were seen in 62 patients.
Diagnoses included both pancreatic and metastatic cancer (28%), pancreatitis (31%), pseudocysts (11%), and intraductal papillary mucinous neoplasms (IPMN) or serous/mucinous cystadenomas (6%). Treatments varied, with 42 patients (19%) undergoing surgery, 39 (17%) receiving chemotherapy, and 14 (6%) electing hospice. The remaining patients had benign findings that were managed with lifestyle modifications and surveillance.
Discussion: While many cases of pancreatic head fullness were benign, malignancy was identified in 28% of patients. The significant proportion of patients lost to follow-up or without further evaluation may have underestimated malignancy rates. These findings emphasize the importance of standardized diagnostic and management protocols to optimize patient outcomes and improve surveillance practices in patients with pancreatic head fullness detected on imaging.
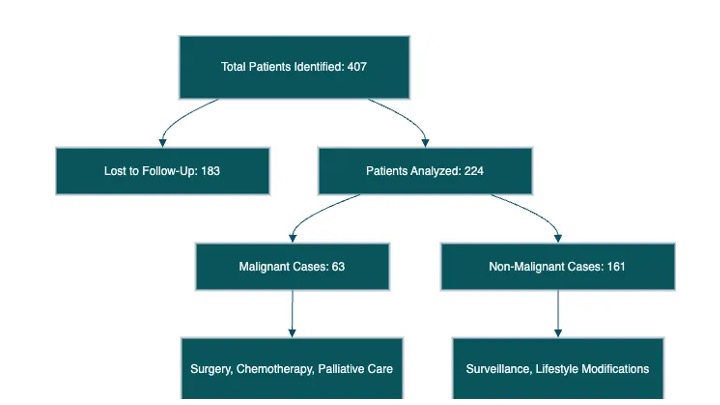
Figure: Table 1 and Table 2
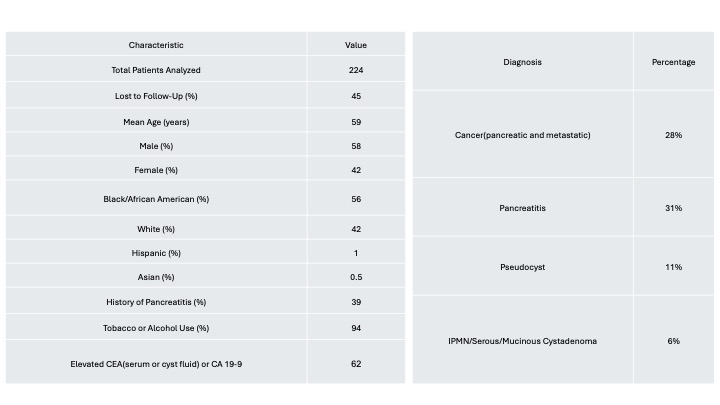
Figure: Figure 1
Disclosures:
Omar Khan indicated no relevant financial relationships.
Ahmad Alkurd indicated no relevant financial relationships.
Cole Bourgeois indicated no relevant financial relationships.
Katelyn Foreman indicated no relevant financial relationships.
Erika Lytle indicated no relevant financial relationships.
Brittany Pass indicated no relevant financial relationships.
Connor Plaisance indicated no relevant financial relationships.
Dylan Thompson indicated no relevant financial relationships.
Daniyal Raza indicated no relevant financial relationships.
Qiang Cai indicated no relevant financial relationships.
Omar Khan, MD1, Ahmad Alkurd, MD1, Cole Bourgeois, BS1, Katelyn Foreman, BS1, Erika Lytle, DO2, Brittany Pass, BS1, Connor Plaisance, MD1, Dylan Thompson, BS1, Daniyal Raza, MD1, Qiang Cai, MD, PhD, MACG3. P2219 - Pancreatic Head Fullness: A Retrospective Study of Diagnostic Pathways and Clinical Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1LSU Health Shreveport, Shreveport, LA; 2Edward Via College of Osteopathic Medicine, Shreveport, LA; 3LSU Health Sciences Center - SHREVEPORT, LA, Shreveport, LA
Introduction: Pancreatic head fullness is an incidental imaging finding often seen on computed tomography (CT) or magnetic resonance imaging (MRI). The lack of standardized guidelines for evaluating this finding creates uncertainty in its management and outcomes. While limited studies, primarily focusing on CT scans, suggest that most cases are benign, the potential for malignancy underscores the need for a systematic approach. This study evaluates the diagnostic workup, outcomes, and management of patients with pancreatic head fullness at a single academic center.
Methods: This retrospective study identified patients through radiology keyword searches for pancreatic head fullness on CT or MRI from January 2020 to March 2024. Data collected included demographics (Table 2), clinical history, EUS with or without fine-needle aspiration (FNA) or biopsy (FNB), tumor markers, final diagnoses (Table 1), and treatments. Patients without definitive diagnoses or those lost to follow-up were excluded from the final analysis. Descriptive statistics summarized the findings.
Results: Among 407 identified patients, 183 (45%) were excluded due to loss to follow-up or absence of further workup. The final analysis comprised 224 patients, with an average age of 59 years; 58% were male and 42% female. The racial distribution was 56% Black, 42% White, and 1% Hispanic. A history of pancreatitis was documented in 39% of patients. 94% of patients reported tobacco or alcohol use. EUS was performed in 48% (n=107), with 78 undergoing FNA/FNB. An elevated CEA level, either from the serum or cystic fluid, or an elevated CA 19-9 were seen in 62 patients.
Diagnoses included both pancreatic and metastatic cancer (28%), pancreatitis (31%), pseudocysts (11%), and intraductal papillary mucinous neoplasms (IPMN) or serous/mucinous cystadenomas (6%). Treatments varied, with 42 patients (19%) undergoing surgery, 39 (17%) receiving chemotherapy, and 14 (6%) electing hospice. The remaining patients had benign findings that were managed with lifestyle modifications and surveillance.
Discussion: While many cases of pancreatic head fullness were benign, malignancy was identified in 28% of patients. The significant proportion of patients lost to follow-up or without further evaluation may have underestimated malignancy rates. These findings emphasize the importance of standardized diagnostic and management protocols to optimize patient outcomes and improve surveillance practices in patients with pancreatic head fullness detected on imaging.
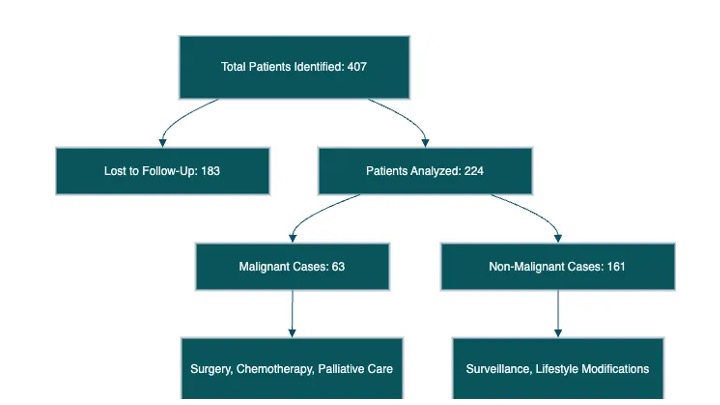
Figure: Table 1 and Table 2
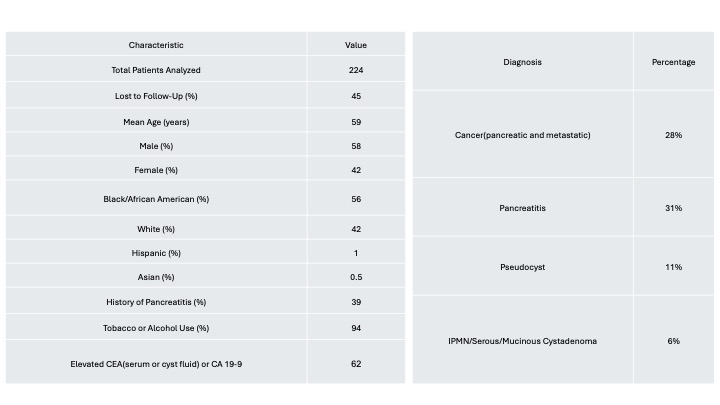
Figure: Figure 1
Disclosures:
Omar Khan indicated no relevant financial relationships.
Ahmad Alkurd indicated no relevant financial relationships.
Cole Bourgeois indicated no relevant financial relationships.
Katelyn Foreman indicated no relevant financial relationships.
Erika Lytle indicated no relevant financial relationships.
Brittany Pass indicated no relevant financial relationships.
Connor Plaisance indicated no relevant financial relationships.
Dylan Thompson indicated no relevant financial relationships.
Daniyal Raza indicated no relevant financial relationships.
Qiang Cai indicated no relevant financial relationships.
Omar Khan, MD1, Ahmad Alkurd, MD1, Cole Bourgeois, BS1, Katelyn Foreman, BS1, Erika Lytle, DO2, Brittany Pass, BS1, Connor Plaisance, MD1, Dylan Thompson, BS1, Daniyal Raza, MD1, Qiang Cai, MD, PhD, MACG3. P2219 - Pancreatic Head Fullness: A Retrospective Study of Diagnostic Pathways and Clinical Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
