Monday Poster Session
Category: Biliary/Pancreas
P2218 - Healthcare Resource Utilization and Expenditures in US Adults at Risk for Pancreatic Exocrine Insufficiency: A Population-Based Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- HL
Haeseon Lee, PharmD, MSc (she/her/hers)
University of Utah
Salt Lake City, UT
Presenting Author(s)
Haeseon Lee, PharmD, MSc1, Jeong-Yeon Cho, PharmD, PhD1, Daryl Ramai, MD, MPH, MSc2, Kyoo Kim, MSc3, Dafni Fragkogianni, MD3, Gamar Akhundova-Unadkat, MD3, Miroslav Vujasinovic, MD, PhD4, J.-Matthias Löhr, MD5, Nathorn Chaiyakunapruk, PharmD, PhD1
1University of Utah, Salt Lake City, UT; 2Brigham and Women's Hospital, Boston, MA; 3Abbott Products Operations AG, Allschwil, Basel-Landschaft, Switzerland; 4Karolinska University Hospital, Karolinska Institutet, Stockholm, Stockholms Lan, Sweden; 5Karolinska University Hospital, Karolinska Institutet, Huddinge, Stockholms Lan, Sweden
Introduction: Pancreatic exocrine insufficiency (PEI) imposes a substantial burden on patients due to chronic gastrointestinal symptoms and long-term nutritional complications. Despite the clinical importance, healthcare resource utilization and its economic impact in the U.S. remain underexplored. This study assessed management practices and medical expenditures among adults at risk for PEI.
Methods: We conducted a retrospective cohort study using electronic health records from the University of Utah Health. The study included patients diagnosed with PEI, chronic pancreatitis, cystic fibrosis, or pancreatic cancer, or who underwent pancreatic surgery between Jan 2016 and Apr 2022. Those with less than six months of follow-up or with cancer other than pancreatic cancer were excluded. Patients were classified as "confirmed PEI" if they had an ICD-10 code for PEI (K86.81) or received pancreatic enzyme replacement therapy (PERT). Inverse probability of treatment weighting (IPTW) was applied to adjust for baseline covariates. Primary outcomes included annualized healthcare costs and utilization. We also examined therapeutic regimens, diagnostic testing, and specialist involvement.
Results: Of 2,578 patients, 1,108 (43.0%) had confirmed PEI. After IPTW adjustment, patients with confirmed PEI had more annualized outpatient visits (7.7 vs 6.2, P < 0.001) and inpatient days (6.6 vs 5.1, p=0.01) compared to those without PEI. Total healthcare costs were also higher ($116,354 vs $78,983, P < 0.001). Among patients with confirmed PEI, outpatient and inpatient costs accounted for 58.5% and 39.6% of total costs, respectively. In this group, 75.4% received PERT, 19.4% had dietary counseling, while 20.9% received neither intervention. Patients receiving PERT or counseling were significantly more likely to have consulted specialists (odds ratio 3.8, 95% CI 2.6–5.7, P < 0.001). Fecal diagnostic testing was performed in 14.2% of confirmed PEI cases, with fecal fat estimation, a clinical standard, conducted in only 4.0%.
Discussion: This study highlights the significant clinical and economic burden associated with PEI in the U.S., due to increased use of both outpatient and inpatient services. PEI is frequently underdiagnosed and undertreated, contributing to avoidable resource utilization. Improving diagnostic practices, ensuring timely and appropriate initiation of PERT, and facilitating specialist involvement are critical steps toward closing existing care gaps and reducing overall healthcare expenditures.
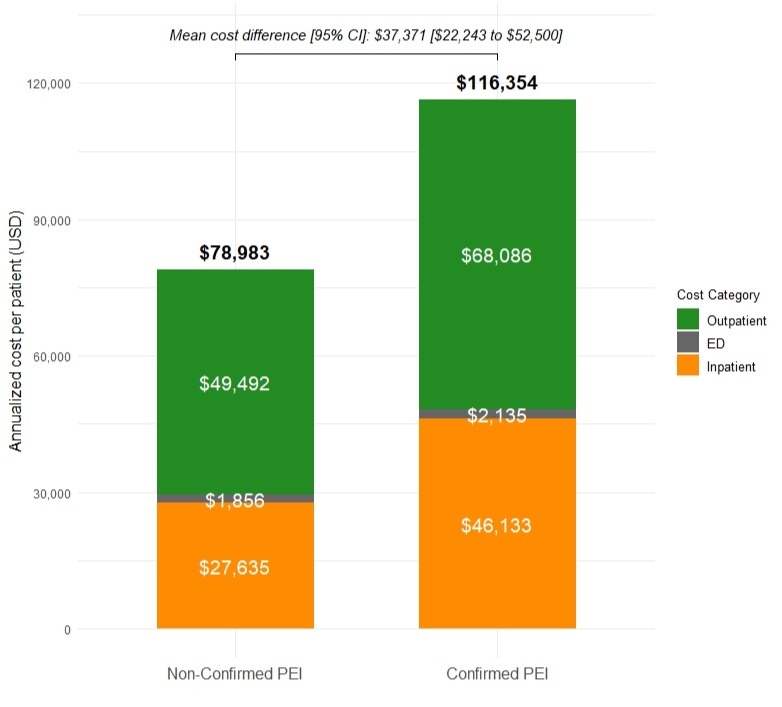
Figure: Total Healthcare Costs among Patients at Risk for Pancreatic Exocrine Insufficiency
Disclosures:
Haeseon Lee: Abbott Products Operations AG – Grant/Research Support.
Jeong-Yeon Cho: Abbott Products Operations AG – Grant/Research Support.
Daryl Ramai indicated no relevant financial relationships.
Kyoo Kim: Abbott Products Operations AG – Employee.
Dafni Fragkogianni: Abbott Products Operations AG – Employee.
Gamar Akhundova-Unadkat: Abbott Products Operations AG – Employee.
Miroslav Vujasinovic: Abbott Products Operations AG – Advisory Committee/Board Member, Speakers Bureau. Amgen Inc – Advisory Committee/Board Member, Speakers Bureau. Nordmark Pharma – Speakers Bureau. Viatris – Speakers Bureau.
J.-Matthias Löhr: Abbott Products Operations AG – Advisory Committee/Board Member, Speakers Bureau. Amgen Inc – Advisory Committee/Board Member. FrostPharma – Speakers Bureau. Nordmark Pharma – Speakers Bureau. Viatris – Speakers Bureau.
Nathorn Chaiyakunapruk: Abbott Products Operations AG – Grant/Research Support.
Haeseon Lee, PharmD, MSc1, Jeong-Yeon Cho, PharmD, PhD1, Daryl Ramai, MD, MPH, MSc2, Kyoo Kim, MSc3, Dafni Fragkogianni, MD3, Gamar Akhundova-Unadkat, MD3, Miroslav Vujasinovic, MD, PhD4, J.-Matthias Löhr, MD5, Nathorn Chaiyakunapruk, PharmD, PhD1. P2218 - Healthcare Resource Utilization and Expenditures in US Adults at Risk for Pancreatic Exocrine Insufficiency: A Population-Based Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Utah, Salt Lake City, UT; 2Brigham and Women's Hospital, Boston, MA; 3Abbott Products Operations AG, Allschwil, Basel-Landschaft, Switzerland; 4Karolinska University Hospital, Karolinska Institutet, Stockholm, Stockholms Lan, Sweden; 5Karolinska University Hospital, Karolinska Institutet, Huddinge, Stockholms Lan, Sweden
Introduction: Pancreatic exocrine insufficiency (PEI) imposes a substantial burden on patients due to chronic gastrointestinal symptoms and long-term nutritional complications. Despite the clinical importance, healthcare resource utilization and its economic impact in the U.S. remain underexplored. This study assessed management practices and medical expenditures among adults at risk for PEI.
Methods: We conducted a retrospective cohort study using electronic health records from the University of Utah Health. The study included patients diagnosed with PEI, chronic pancreatitis, cystic fibrosis, or pancreatic cancer, or who underwent pancreatic surgery between Jan 2016 and Apr 2022. Those with less than six months of follow-up or with cancer other than pancreatic cancer were excluded. Patients were classified as "confirmed PEI" if they had an ICD-10 code for PEI (K86.81) or received pancreatic enzyme replacement therapy (PERT). Inverse probability of treatment weighting (IPTW) was applied to adjust for baseline covariates. Primary outcomes included annualized healthcare costs and utilization. We also examined therapeutic regimens, diagnostic testing, and specialist involvement.
Results: Of 2,578 patients, 1,108 (43.0%) had confirmed PEI. After IPTW adjustment, patients with confirmed PEI had more annualized outpatient visits (7.7 vs 6.2, P < 0.001) and inpatient days (6.6 vs 5.1, p=0.01) compared to those without PEI. Total healthcare costs were also higher ($116,354 vs $78,983, P < 0.001). Among patients with confirmed PEI, outpatient and inpatient costs accounted for 58.5% and 39.6% of total costs, respectively. In this group, 75.4% received PERT, 19.4% had dietary counseling, while 20.9% received neither intervention. Patients receiving PERT or counseling were significantly more likely to have consulted specialists (odds ratio 3.8, 95% CI 2.6–5.7, P < 0.001). Fecal diagnostic testing was performed in 14.2% of confirmed PEI cases, with fecal fat estimation, a clinical standard, conducted in only 4.0%.
Discussion: This study highlights the significant clinical and economic burden associated with PEI in the U.S., due to increased use of both outpatient and inpatient services. PEI is frequently underdiagnosed and undertreated, contributing to avoidable resource utilization. Improving diagnostic practices, ensuring timely and appropriate initiation of PERT, and facilitating specialist involvement are critical steps toward closing existing care gaps and reducing overall healthcare expenditures.
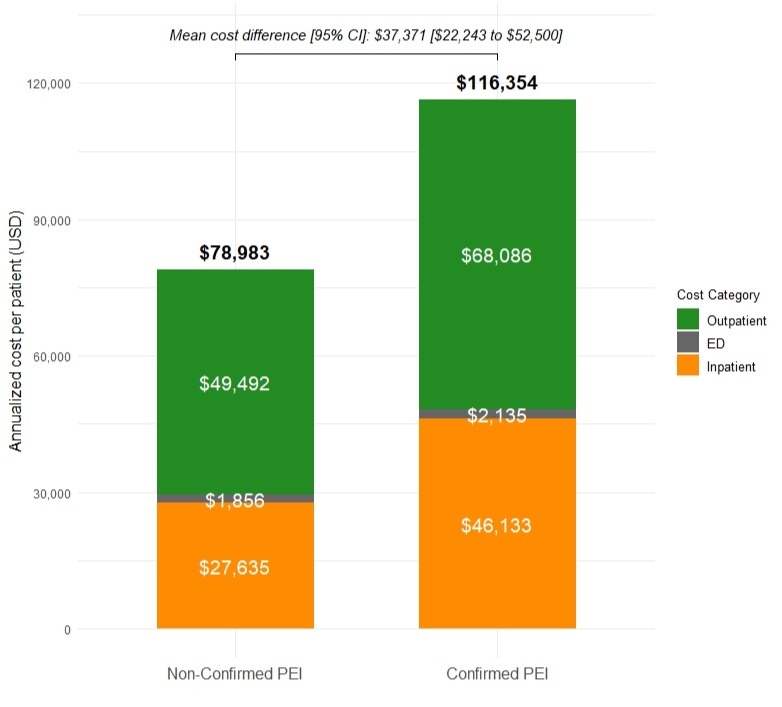
Figure: Total Healthcare Costs among Patients at Risk for Pancreatic Exocrine Insufficiency
Disclosures:
Haeseon Lee: Abbott Products Operations AG – Grant/Research Support.
Jeong-Yeon Cho: Abbott Products Operations AG – Grant/Research Support.
Daryl Ramai indicated no relevant financial relationships.
Kyoo Kim: Abbott Products Operations AG – Employee.
Dafni Fragkogianni: Abbott Products Operations AG – Employee.
Gamar Akhundova-Unadkat: Abbott Products Operations AG – Employee.
Miroslav Vujasinovic: Abbott Products Operations AG – Advisory Committee/Board Member, Speakers Bureau. Amgen Inc – Advisory Committee/Board Member, Speakers Bureau. Nordmark Pharma – Speakers Bureau. Viatris – Speakers Bureau.
J.-Matthias Löhr: Abbott Products Operations AG – Advisory Committee/Board Member, Speakers Bureau. Amgen Inc – Advisory Committee/Board Member. FrostPharma – Speakers Bureau. Nordmark Pharma – Speakers Bureau. Viatris – Speakers Bureau.
Nathorn Chaiyakunapruk: Abbott Products Operations AG – Grant/Research Support.
Haeseon Lee, PharmD, MSc1, Jeong-Yeon Cho, PharmD, PhD1, Daryl Ramai, MD, MPH, MSc2, Kyoo Kim, MSc3, Dafni Fragkogianni, MD3, Gamar Akhundova-Unadkat, MD3, Miroslav Vujasinovic, MD, PhD4, J.-Matthias Löhr, MD5, Nathorn Chaiyakunapruk, PharmD, PhD1. P2218 - Healthcare Resource Utilization and Expenditures in US Adults at Risk for Pancreatic Exocrine Insufficiency: A Population-Based Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
