Monday Poster Session
Category: Biliary/Pancreas
P2209 - Outcomes of Necrotizing Pancreatitis in Patients with Obesity: Insights from National Inpatient Sample
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Peter Kim, MD
University of Minnesota Medical Center
Minneapolis, MN
Presenting Author(s)
Peter Kim, MD1, Hima Varsha Voruganti, MD2, Rahul Karna, MD1, Mohammad Bilal, MD, FACG3
1University of Minnesota Medical Center, Minneapolis, MN; 2North Alabama Medical Center, Florence, AL; 3University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Obesity is associated with higher risk of complications in patients with acute pancreatitis. Increased cytokine release, adipokine levels, and unsaturated fatty acid-mediated lipotoxicity have been hypothesized as mediators of inflammation in obese patients. Necrotizing pancreatitis (NP) accounts for 5–10% of pancreatitis cases and is associated with increased morbidity and mortality compared to interstitial pancreatitis. However, the impact of body mass index (BMI) on NP has not been well-characterized.
Methods: We conducted a retrospective cohort study of patients with NP using the 2020 National Inpatient Sample database. Patients were categorized into two cohorts: NP with obesity and NP without obesity. We assessed outcomes including respiratory failure, portal vein thrombosis, and use of interventions such as mechanical ventilation, hemodialysis, open necrosectomy, endoscopic drainage, percutaneous drainage, laparoscopic drainage, length of stay, and in-hospital mortality. Multivariate regression analyses were used to compare outcomes after controlling for confounders such as sex, age, Charlson Comorbidity Index, household income, and insurance status.
Results: Among 4,555 hospitalized NP patients, 3,390 (74.8%) comprised the obese cohort and 1,165 (25.2%) comprised the non-obese cohort. Demographic characteristics of both cohorts are demonstrated in Table 1. The obese cohort had significantly higher rates of acute hypoxic respiratory failure (20.05% vs 10.73%, adjusted odds ratio [aOR] 2.75, CI 1.65-4.60, p< 0.001), intubation (13.4% vs 7.29%, aOR 2.25, CI 1.26-4.01, p=0.006), and hemodialysis (4.42% vs 1.29%, aOR 4.31, CI 1.28-14.67, p=0.019). The non-obese cohort had significantly higher rates of portal vein thrombosis (10.73% vs 6.04%, aOR 0.52, CI 0.29-0.93, p=0.027), open necrosectomy (6.14% vs 2.50%, aOR 0.47, CI 0.22-0.98, p=0.045), and endoscopic drainage (6.08% vs 2.21%, aOR 0.29, CI 0.12-0.70, p=0.006). Overall, length of stay (11.42 vs 10.68 days, p=0.739) and in-hospital mortality (aOR 1.38, 95% CI 0.53-3.58, p=0.502) did not differ significantly between cohorts. Table 2 demonstrates outcomes of patients with NP between obese and non-obese cohorts.
Discussion: Our large database study suggests that obesity in NP patients is associated with severe extra-pancreatic manifestations while non-obese patients have higher odds of drainage procedures. Future studies should assess the reasons for increased need for drainage procedures in non-obese patients.
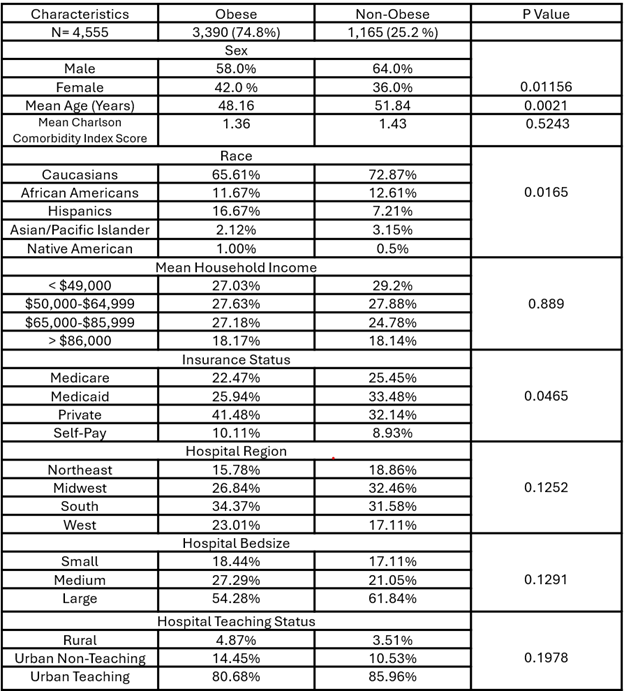
Figure: Table 1. Demographics of Obese vs Non-Obese Patients Admitted With Necrotizing Pancreatitis
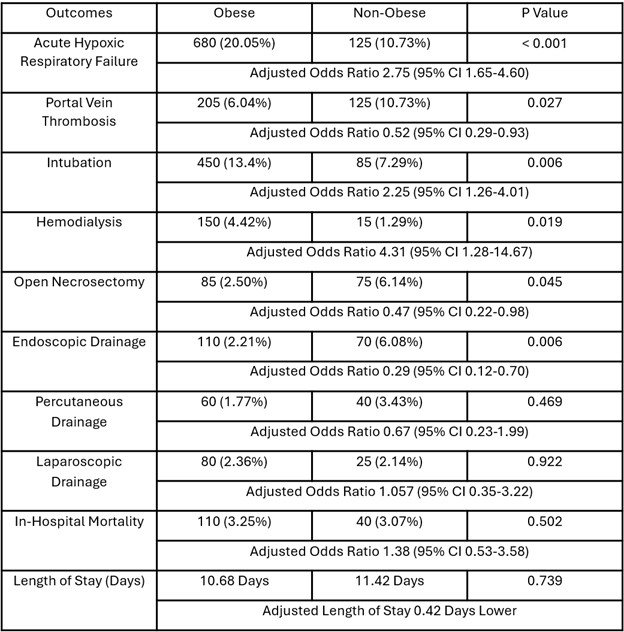
Figure: Table 2. In-Hospital Outcomes in Obese vs Non-Obese Patients With Necrotizing Pancreatitis
Disclosures:
Peter Kim indicated no relevant financial relationships.
Hima Varsha Voruganti indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Peter Kim, MD1, Hima Varsha Voruganti, MD2, Rahul Karna, MD1, Mohammad Bilal, MD, FACG3. P2209 - Outcomes of Necrotizing Pancreatitis in Patients with Obesity: Insights from National Inpatient Sample, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Minnesota Medical Center, Minneapolis, MN; 2North Alabama Medical Center, Florence, AL; 3University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Obesity is associated with higher risk of complications in patients with acute pancreatitis. Increased cytokine release, adipokine levels, and unsaturated fatty acid-mediated lipotoxicity have been hypothesized as mediators of inflammation in obese patients. Necrotizing pancreatitis (NP) accounts for 5–10% of pancreatitis cases and is associated with increased morbidity and mortality compared to interstitial pancreatitis. However, the impact of body mass index (BMI) on NP has not been well-characterized.
Methods: We conducted a retrospective cohort study of patients with NP using the 2020 National Inpatient Sample database. Patients were categorized into two cohorts: NP with obesity and NP without obesity. We assessed outcomes including respiratory failure, portal vein thrombosis, and use of interventions such as mechanical ventilation, hemodialysis, open necrosectomy, endoscopic drainage, percutaneous drainage, laparoscopic drainage, length of stay, and in-hospital mortality. Multivariate regression analyses were used to compare outcomes after controlling for confounders such as sex, age, Charlson Comorbidity Index, household income, and insurance status.
Results: Among 4,555 hospitalized NP patients, 3,390 (74.8%) comprised the obese cohort and 1,165 (25.2%) comprised the non-obese cohort. Demographic characteristics of both cohorts are demonstrated in Table 1. The obese cohort had significantly higher rates of acute hypoxic respiratory failure (20.05% vs 10.73%, adjusted odds ratio [aOR] 2.75, CI 1.65-4.60, p< 0.001), intubation (13.4% vs 7.29%, aOR 2.25, CI 1.26-4.01, p=0.006), and hemodialysis (4.42% vs 1.29%, aOR 4.31, CI 1.28-14.67, p=0.019). The non-obese cohort had significantly higher rates of portal vein thrombosis (10.73% vs 6.04%, aOR 0.52, CI 0.29-0.93, p=0.027), open necrosectomy (6.14% vs 2.50%, aOR 0.47, CI 0.22-0.98, p=0.045), and endoscopic drainage (6.08% vs 2.21%, aOR 0.29, CI 0.12-0.70, p=0.006). Overall, length of stay (11.42 vs 10.68 days, p=0.739) and in-hospital mortality (aOR 1.38, 95% CI 0.53-3.58, p=0.502) did not differ significantly between cohorts. Table 2 demonstrates outcomes of patients with NP between obese and non-obese cohorts.
Discussion: Our large database study suggests that obesity in NP patients is associated with severe extra-pancreatic manifestations while non-obese patients have higher odds of drainage procedures. Future studies should assess the reasons for increased need for drainage procedures in non-obese patients.
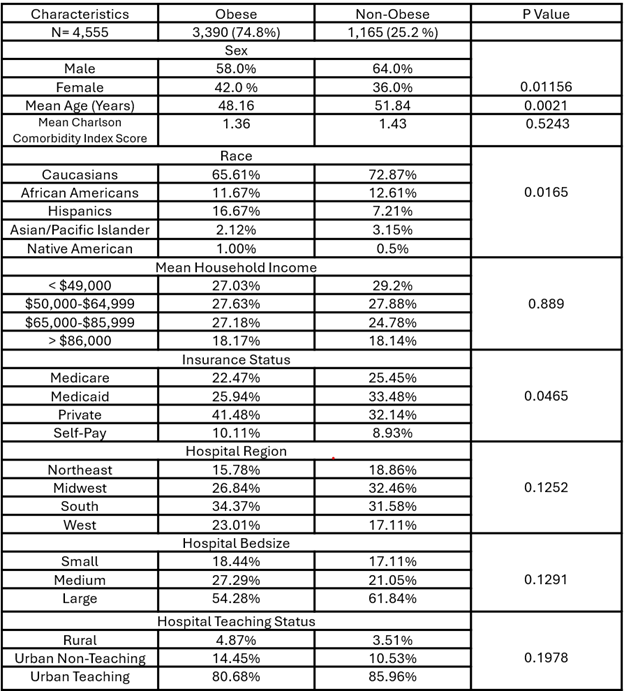
Figure: Table 1. Demographics of Obese vs Non-Obese Patients Admitted With Necrotizing Pancreatitis
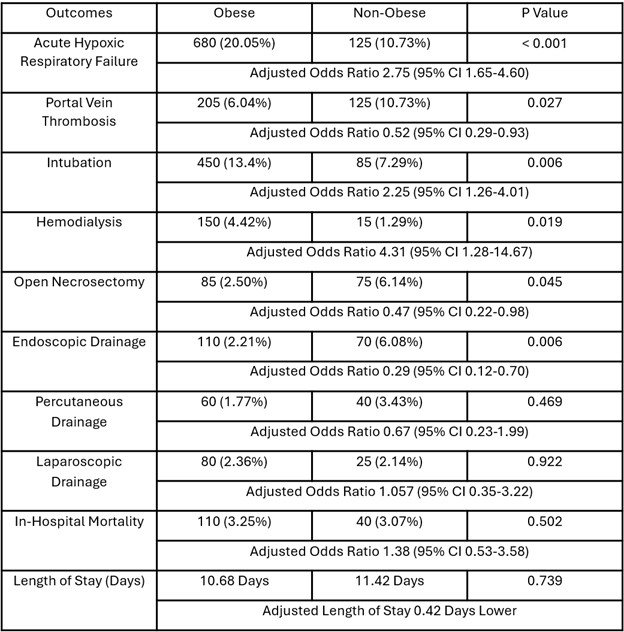
Figure: Table 2. In-Hospital Outcomes in Obese vs Non-Obese Patients With Necrotizing Pancreatitis
Disclosures:
Peter Kim indicated no relevant financial relationships.
Hima Varsha Voruganti indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Peter Kim, MD1, Hima Varsha Voruganti, MD2, Rahul Karna, MD1, Mohammad Bilal, MD, FACG3. P2209 - Outcomes of Necrotizing Pancreatitis in Patients with Obesity: Insights from National Inpatient Sample, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
