Monday Poster Session
Category: Biliary/Pancreas
Outcomes of Acute Pancreatitis in Patients With and Without <i>C. difficile</i> Infection: A Nationwide Study
P2201 - Outcomes of Acute Pancreatitis in Patients With and Without C. difficile Infection: A Nationwide Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Raj H. Patel, MD
St. Mary Medical Center
Langhorne, PA
Presenting Author(s)
Raj H. Patel, MD1, Sneh Sonaiya, MD, MPH, MBA2, Charmy Parikh, MD3, Karan J.. Yagnik, MD4, Pranav Patel, MD5, Umang Patel, DO1, Bradley D. Confer, DO5, Harshit S. Khara, MD6
1St. Mary Medical Center, Langhorne, PA; 2University of Nevada, Las Vegas, Las Vegas, NV; 3Mercy Catholic Medical Center, Darby, PA; 4Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University, Long Branch, NJ; 5Geisinger Health System, Danville, PA; 6Geisinger Health System, Danville, NJ
Introduction:
A significant increase has been noted in hospital admissions for patients with Acute Pancreatitis (AP) in the past decade. This also increases the risk of exposure to C. difficile infection (CDI. Although CDI primarily affects the colon, rising data reveal it has a significant impact on the hepatobiliary system. In this study, we aim to analyze potential clinical outcomes of CDI in patients with AP with a focus on overall resource utilization.
Methods: The National Inpatient Sample (NIS) database from 2016 to 2020 was utilized to identify adult hospitalizations (age >18 years) with a primary diagnosis of AP. Patients were stratified into 2 groups based on the presence or absence of CDI. Propensity score matching was conducted to adjust for baseline characteristics. SAS 9.4 was used to analyze the inpatient outcomes, including inpatient mortality, length of stay (LOS), total hospital charges (THC; inflation-adjusted to 2020 USD), and utilization of critical care interventions (e.g., intubation, ICU admission).
Results: 46,900 patients with AP were stratified into 2 propensity-matched groups: patients with CDI (n=23450, mean age 55.2 years) and without CDI (n=23450, mean age 53.2 years). Patients in the CDI group had significantly higher inpatient mortality (6.2% vs. 2.4%, p< 0.001), longer LOS (median 13.2 vs. 5.3 days, p< 0.001), and higher THC (mean $38,789 vs. $14,455, p< 0.001). CDI in AP patients was associated with a significantly higher rate of non-infectious necrosis (7.8% vs 3.76%, p< 0.001) and infectious necrosis (3.49% vs 1.08%, p< 0.001) compared to non-CDI group. Rates of pseudocyst formation (9.7% vs. 6.1%, p< 0.001) and abdominal compartment syndrome (0.7% vs. 0.1%, p< 0.001) were also higher in patients with CDI. Furthermore, CDI group demonstrated a higher rate of complications, including septic shock, peritonitis, septicemia, AKI, and pulmonary embolism (p< 0.001).
The need for critical care interventions was relatively higher in CDI cohort, with increased rates of intubation, CVC placement, pressor support, and ICU admission (p< 0.001).
Discussion: Our findings reveal significantly poor outcomes and increased healthcare resource utilization in AP patients with CDI, underscoring the need for clinical vigilance, judicious use of antibiotics, and tailored management strategies for the vulnerable population.
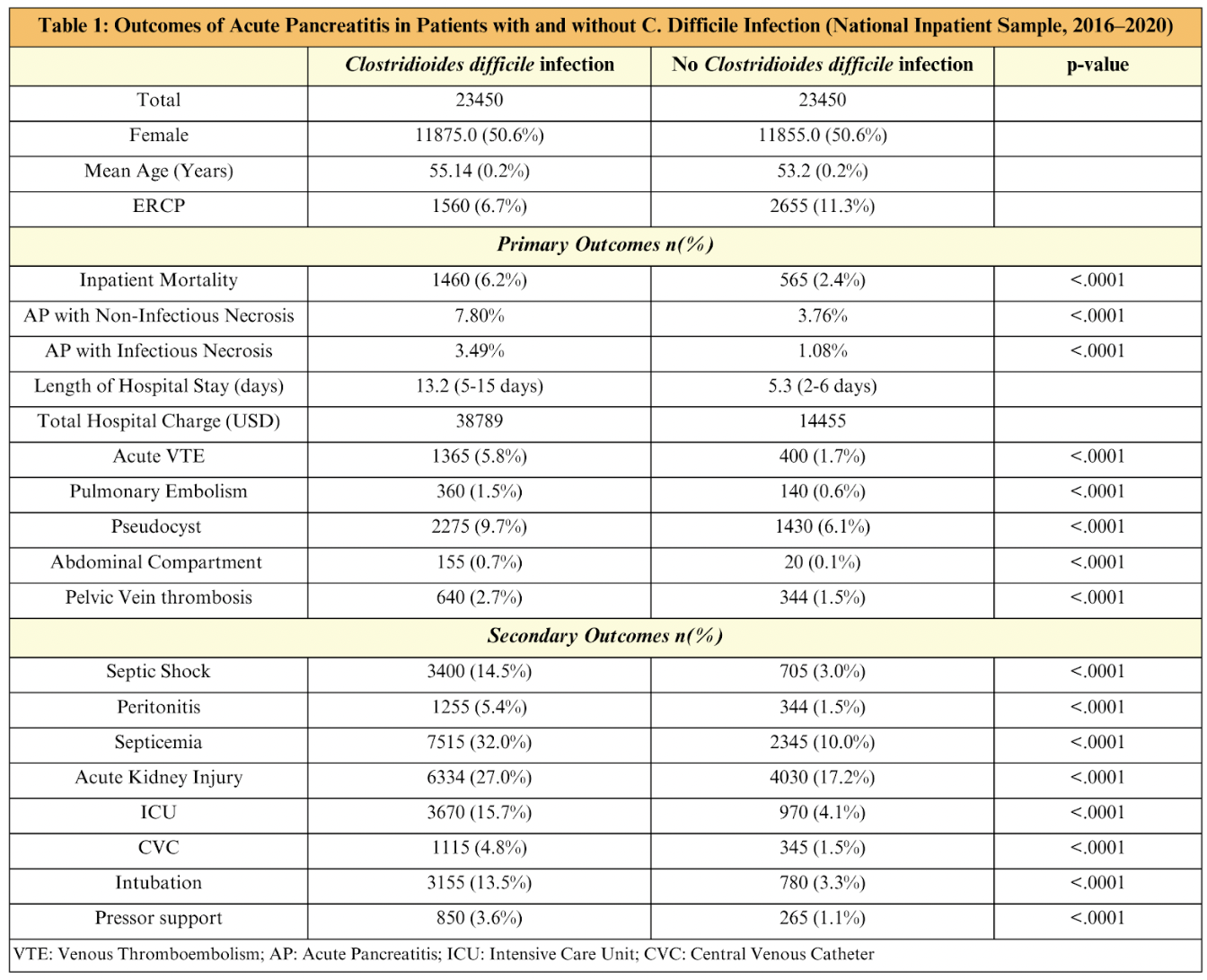
Figure: Outcomes of Acute Pancreatitis in Patients with and without C. difficile Infection
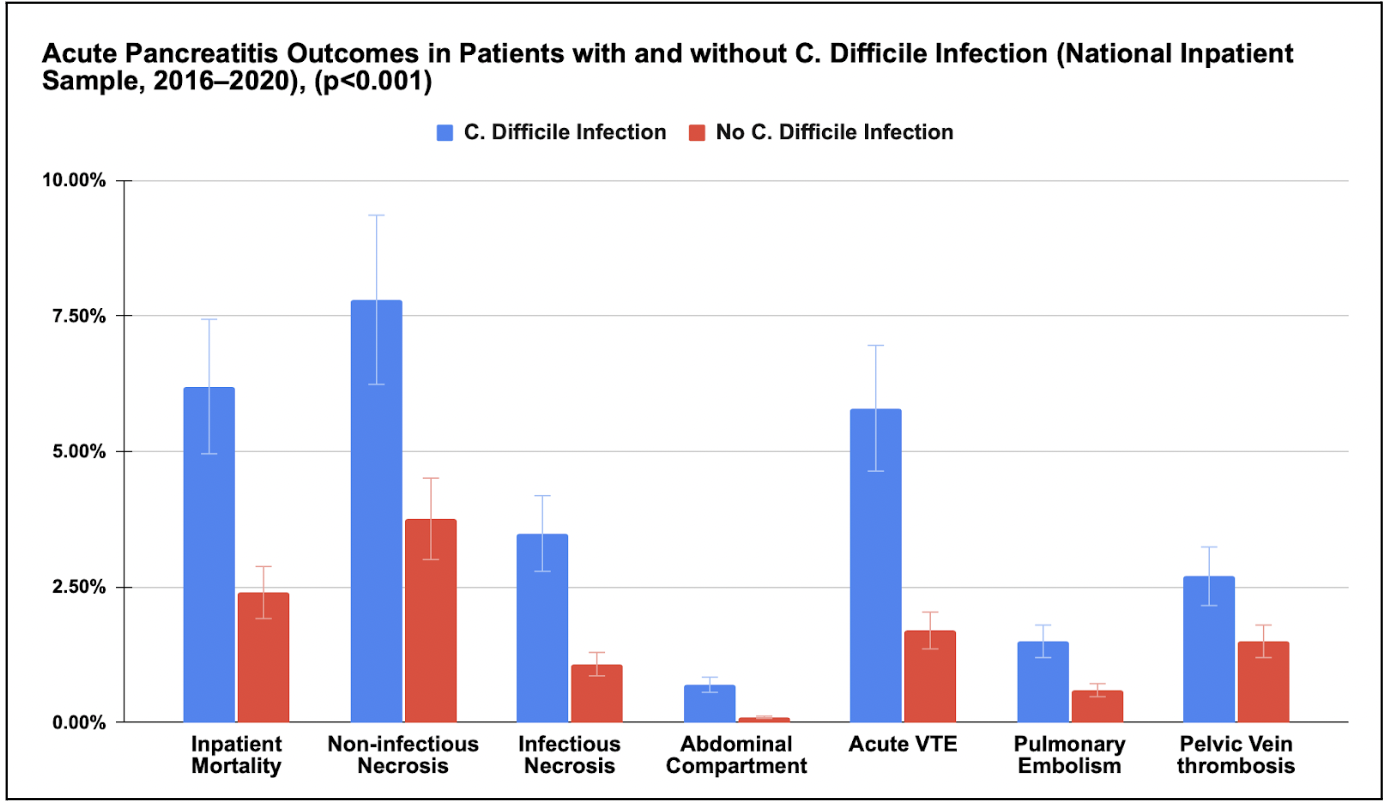
Figure: Acute Pancreatitis Outcomes in Patients with and without C. difficile Infection (p value < 0.001) [Graphical representation]
Disclosures:
Raj Patel indicated no relevant financial relationships.
Sneh Sonaiya indicated no relevant financial relationships.
Charmy Parikh indicated no relevant financial relationships.
Karan Yagnik indicated no relevant financial relationships.
Pranav Patel indicated no relevant financial relationships.
Umang Patel indicated no relevant financial relationships.
Bradley Confer indicated no relevant financial relationships.
Harshit Khara indicated no relevant financial relationships.
Raj H. Patel, MD1, Sneh Sonaiya, MD, MPH, MBA2, Charmy Parikh, MD3, Karan J.. Yagnik, MD4, Pranav Patel, MD5, Umang Patel, DO1, Bradley D. Confer, DO5, Harshit S. Khara, MD6. P2201 - Outcomes of Acute Pancreatitis in Patients With and Without <i>C. difficile</i> Infection: A Nationwide Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Mary Medical Center, Langhorne, PA; 2University of Nevada, Las Vegas, Las Vegas, NV; 3Mercy Catholic Medical Center, Darby, PA; 4Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University, Long Branch, NJ; 5Geisinger Health System, Danville, PA; 6Geisinger Health System, Danville, NJ
Introduction:
A significant increase has been noted in hospital admissions for patients with Acute Pancreatitis (AP) in the past decade. This also increases the risk of exposure to C. difficile infection (CDI. Although CDI primarily affects the colon, rising data reveal it has a significant impact on the hepatobiliary system. In this study, we aim to analyze potential clinical outcomes of CDI in patients with AP with a focus on overall resource utilization.
Methods: The National Inpatient Sample (NIS) database from 2016 to 2020 was utilized to identify adult hospitalizations (age >18 years) with a primary diagnosis of AP. Patients were stratified into 2 groups based on the presence or absence of CDI. Propensity score matching was conducted to adjust for baseline characteristics. SAS 9.4 was used to analyze the inpatient outcomes, including inpatient mortality, length of stay (LOS), total hospital charges (THC; inflation-adjusted to 2020 USD), and utilization of critical care interventions (e.g., intubation, ICU admission).
Results: 46,900 patients with AP were stratified into 2 propensity-matched groups: patients with CDI (n=23450, mean age 55.2 years) and without CDI (n=23450, mean age 53.2 years). Patients in the CDI group had significantly higher inpatient mortality (6.2% vs. 2.4%, p< 0.001), longer LOS (median 13.2 vs. 5.3 days, p< 0.001), and higher THC (mean $38,789 vs. $14,455, p< 0.001). CDI in AP patients was associated with a significantly higher rate of non-infectious necrosis (7.8% vs 3.76%, p< 0.001) and infectious necrosis (3.49% vs 1.08%, p< 0.001) compared to non-CDI group. Rates of pseudocyst formation (9.7% vs. 6.1%, p< 0.001) and abdominal compartment syndrome (0.7% vs. 0.1%, p< 0.001) were also higher in patients with CDI. Furthermore, CDI group demonstrated a higher rate of complications, including septic shock, peritonitis, septicemia, AKI, and pulmonary embolism (p< 0.001).
The need for critical care interventions was relatively higher in CDI cohort, with increased rates of intubation, CVC placement, pressor support, and ICU admission (p< 0.001).
Discussion: Our findings reveal significantly poor outcomes and increased healthcare resource utilization in AP patients with CDI, underscoring the need for clinical vigilance, judicious use of antibiotics, and tailored management strategies for the vulnerable population.
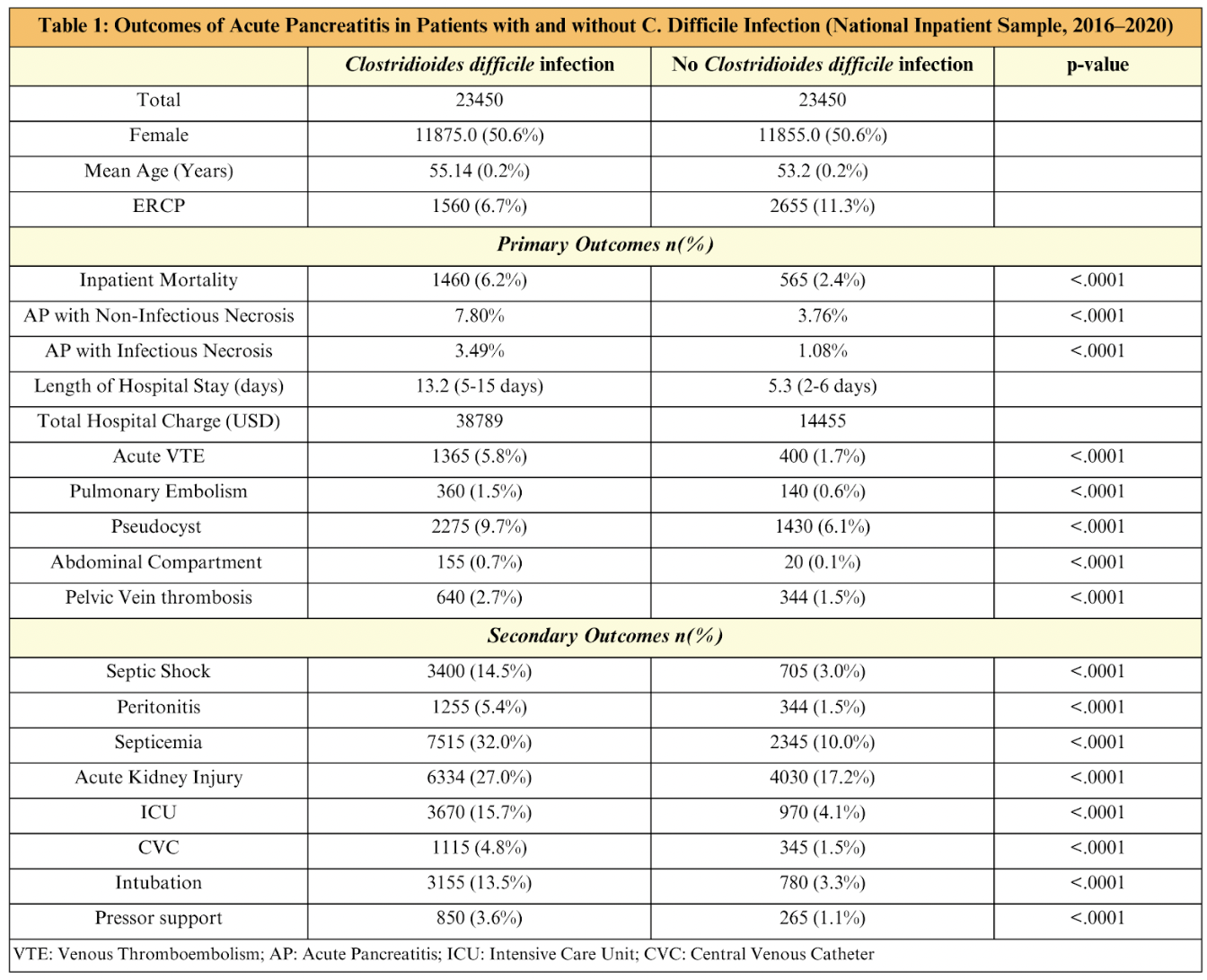
Figure: Outcomes of Acute Pancreatitis in Patients with and without C. difficile Infection
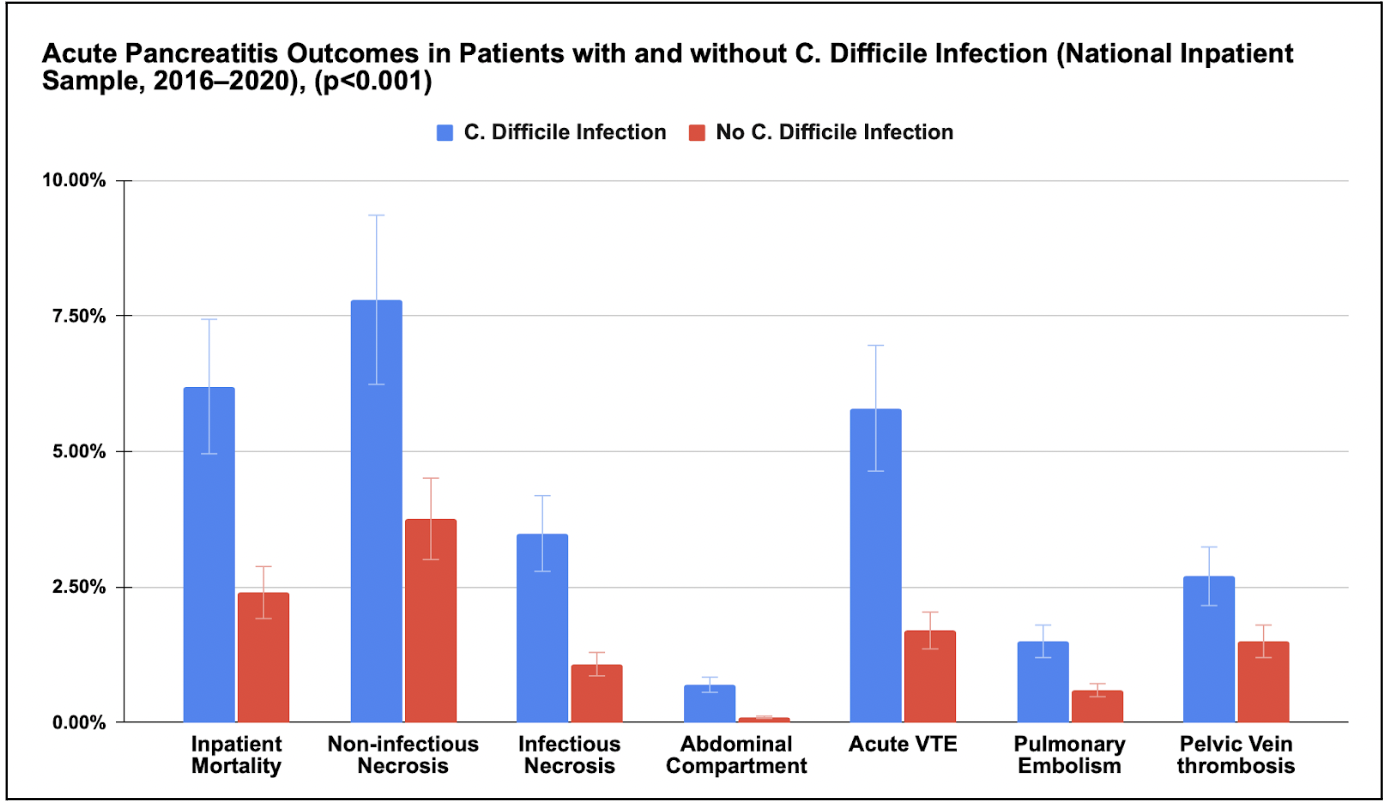
Figure: Acute Pancreatitis Outcomes in Patients with and without C. difficile Infection (p value < 0.001) [Graphical representation]
Disclosures:
Raj Patel indicated no relevant financial relationships.
Sneh Sonaiya indicated no relevant financial relationships.
Charmy Parikh indicated no relevant financial relationships.
Karan Yagnik indicated no relevant financial relationships.
Pranav Patel indicated no relevant financial relationships.
Umang Patel indicated no relevant financial relationships.
Bradley Confer indicated no relevant financial relationships.
Harshit Khara indicated no relevant financial relationships.
Raj H. Patel, MD1, Sneh Sonaiya, MD, MPH, MBA2, Charmy Parikh, MD3, Karan J.. Yagnik, MD4, Pranav Patel, MD5, Umang Patel, DO1, Bradley D. Confer, DO5, Harshit S. Khara, MD6. P2201 - Outcomes of Acute Pancreatitis in Patients With and Without <i>C. difficile</i> Infection: A Nationwide Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
