Tuesday Poster Session
Category: Colon
P4631 - Congenital Perirectal Lymphatico-Venous Malformation and Crohn's Disease: A Rare Coincidence
.jpg)
Bachviet AH Nguyen, MD (he/him/his)
University of British Columbia Department of Medicine
Surrey, BC, Canada
Presenting Author(s)
1University of British Columbia Department of Medicine, Surrey, BC, Canada; 2UBC Department of Medicine/IBD Centre of BC, Vancouver, BC, Canada
Introduction: Lymphatico-venous malformations (LVM) are a result of abnormalities during embryogenesis and are often present since birth. There is a frequent association with phleboliths due to their tendency to thrombose, and typically present on the face, limbs, or trunk. Rarely, LVMs affect the rectum and typically manifest as hematochezia in children and adolescents.
We present the rare case of a patient with Crohn's disease (CD) and an incidentally discovered perirectal LVM.
Case Description/
Methods:
A 36 year old male with a remote history of Crohn’s disease not on medication presented with 2 hours of central abdominal pain radiating to the right lower quadrant (RLQ). He complained of nausea, non-bloody diarrhea, and reported that the pain was different from his previous flares of Crohn’s disease. On examination, he had generalized abdominal tenderness with focal RLQ tenderness. His bloodwork including a CRP was normal.
A CT abdo-pelvis with IV contrast was equivocal for appendicitis, however there was rectal wall thickening and perirectal fat stranding with approximately 50 lymph nodes with eggshell calcifications in the adjacent perirectal fat. A colonoscopy and biopsy demonstrated prominent venous changes at 30cm and in the rectum ; there was also mildly active ileal disease. On MR enterography, there were no features of small bowel CD.
It was concluded that the prominent perirectal vasculature and calcifications were consistent with phleboliths in the setting of a perirectal lymphatico-venous malformation. The patient’s abdominal pain of unclear etiology self-resolved and he continued to remain asymptomatic.
Discussion:
To our knowledge, this is the first case describing a perirectal LVM in a patient with CD. The cause of the patient’s abdominal pain remains unclear given that his history of mildly active left sided Crohn’s colitis is considered inconsistent with his presentation, while intestinal vascular malformations typically involve painless hematochezia. However, there have been case reports describing abdominal pain in patients with a vascular malformation that have led to misdiagnosis with IBD or neoplasm.
As our patient did not have hematochezia, no intervention was performed. For patients with symptomatic LVMs, percutaneous or endoscopy-guided hybrid sclerotherapy is a therapeutic option. It is therefore prudent to consider an LVM in the differential diagnosis of a patient with IBD presenting with rectal bleeding.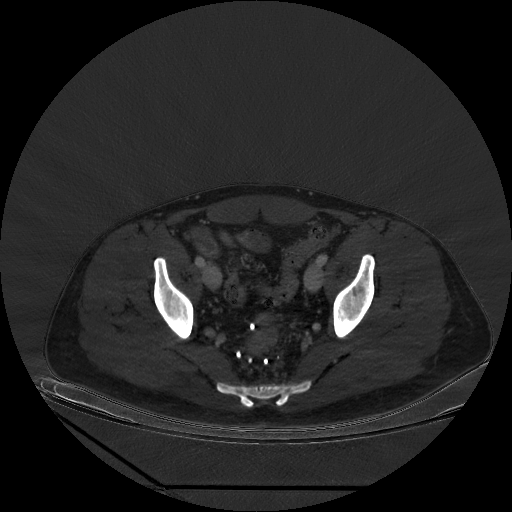
Figure: Figure 1: Axial view of CT abdo-pelvis with iodine contrast. There is moderate rectal wall thickening with perirectal stranding. Punctate calcifications are present within the rectal wall. Numerous (approximately 50) phleboliths in the perirectal fat extending from the distal sigmoid/to the anus.
Disclosures:
Bachviet Nguyen indicated no relevant financial relationships.
Astrid-Jane Williams indicated no relevant financial relationships.
Bachviet AH. Nguyen, MD1, Astrid-Jane Williams, MD2. P4631 - Congenital Perirectal Lymphatico-Venous Malformation and Crohn's Disease: A Rare Coincidence, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
