Tuesday Poster Session
Category: Colon
P4627 - Immune Checkpoint Inhibitor Colitis: A Case Report on How Steroid Use Obscured Diagnosis Until Taper-Induced Flare

Ziad Suleiman, MD (he/him/his)
Southwest healthcare medical education consortium
Murrieta, CA
Presenting Author(s)
1Southwest healthcare medical education consortium, Murrieta, CA; 2Henry Ford Warren, Warren, MI; 3Hamilton Medical Center, Dalton, GA; 4University of South Florida, Port Orange, FL; 5University of Florida, Port Orange, FL
Introduction:
Although they have revolutionized the treatment of various malignancies, immune checkpoint inhibitors (ICIs) are associated with immune-related adverse events (irAEs), with colitis being particularly significant given its potential severity. Corticosteroids are the mainstay treatment of irAEs, including ICI colitis; however, they should be used with caution, as they may affect both irAE control and ICI efficacy. Prior or concurrent steroid use may obscure evolving complications.
Case Description/
Methods:
A 61-year-old male with metastatic melanoma underwent treatment with pembrolizumab. During therapy, he developed persistent flu-like symptoms unresponsive to NSAIDs and was given multiple steroid courses to manage and prevent recurrence of his symptoms. A few weeks after completion of ICI therapy, and while rapidly tapering a steroid course, he presented to the emergency department with severe dehydration, confusion, and abdominal pain. Initial workup showed signs consistent with diabetic ketoacidosis (DKA), as well as abnormal thyroid and adrenal function tests, raising concerns for multiple endocrine irAEs. He was stabilized and discharged on high-dose steroids with instructions for a gradual taper. A few weeks later, he presented with 15–20 episodes of non-bloody diarrhea. Despite the severity of symptoms, colonic mucosa looked normal, with no gross evidence of inflammation. However, biopsies revealed severe active colitis, increased intraepithelial lymphocytes, cryptitis, and crypt abscesses, findings consistent with ICI colitis. High-dose corticosteroids were restarted again, resulting in improvement of symptoms, with instructions for a slow, careful taper to minimize risk of relapse.
Discussion:
Despite being effective in managing irAEs, corticosteroids should be used with caution in patients receiving ICIs. They are typically introduced in response to uncontrolled irAEs; however, they can attenuate ICI efficacy and may obscure the development of more serious complications. In this case, steroids were initially given to manage simple flu-like symptoms. This may have masked the emergence of more serious irAEs, including new-onset diabetes, thyroiditis, adrenalitis, and ultimately colitis (Figure 1). Corticosteroid use in patients receiving ICIs should be reserved for severe or life-threatening irAEs, or when safer therapeutic options have been exhausted. Careful dosing and a gradual tapering regimen are essential to avoid rebound exacerbation of irAEs, which can be potentially fatal.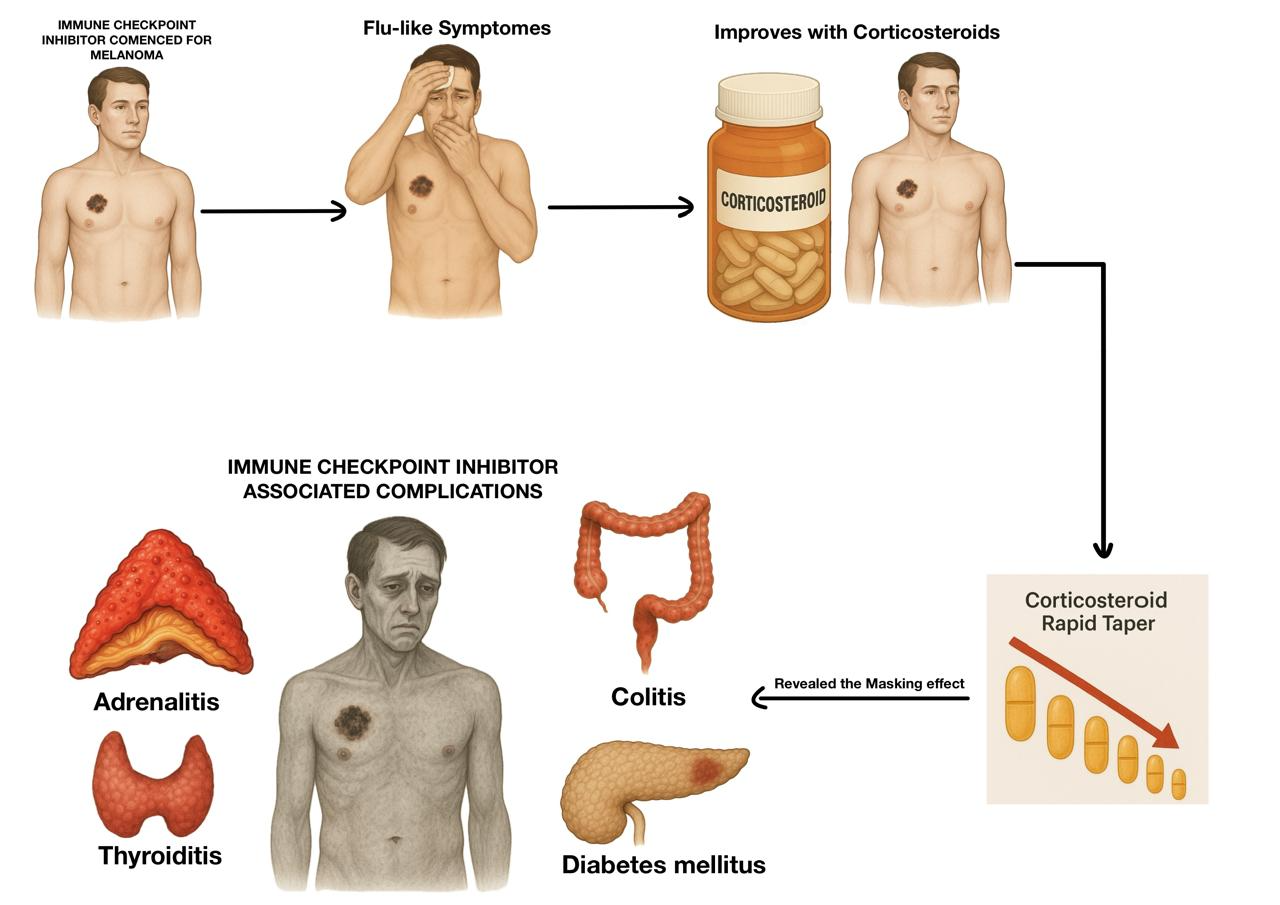
Figure: Figure 1. Summary of the patient clinical course treated with immune checkpoint inhibitor, highlighting how corticosteroid use masked evolving immune-related adverse events. A rapid taper unmasked severe complications including colitis, adrenalitis, thyroiditis, and diabetes mellitus.
Disclosures:
Ziad Suleiman indicated no relevant financial relationships.
Mohamed Alharami indicated no relevant financial relationships.
Omar Alwan indicated no relevant financial relationships.
Kareem Suleiman indicated no relevant financial relationships.
Salem Hemaidan indicated no relevant financial relationships.
Ziad Suleiman, MD1, Mohamed Alharami, MD2, Omar Alwan, MD3, Kareem Suleiman, BS4, Salem Hemaidan, BS5. P4627 - Immune Checkpoint Inhibitor Colitis: A Case Report on How Steroid Use Obscured Diagnosis Until Taper-Induced Flare, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
