Tuesday Poster Session
Category: Colon
P4618 - Heterotopia in Hindsight: A Stomach Where It Shouldn’t Be
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Alexa Plato, MD
Yale New Haven Health, Bridgeport Hospital
Bridgeport, CT
Presenting Author(s)
Alexa Plato, MD1, Cheng-Hung Tai, MD1, Raquel Rozner, MD2, Paul Cohen, MD1
1Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 2Yale School of Medicine, Gastroenterology Associates, PC, Northeast Medical Group/Yale New Haven Health, Stratford, CT
Introduction: Gastric heterotopia (GH) refers to the presence of gastric mucosa outside its normal anatomic
location. While GH is most commonly observed in the esophagus and duodenum, its occurrence
in the rectum is exceedingly rare, with limited case reports and unclear clinical implications.
Though often asymptomatic, GH has been associated with rectal bleeding, abdominal pain, and
potential malignant transformation.
Case Description/
Methods: A 45-year-old woman with a history of asthma, Graves’ disease, and migraines underwent
a routine screening colonoscopy. She reported intermittent constipation managed with docusate
but denied hematochezia, abdominal pain, weight loss, or family history of colorectal cancer.
Physical exam and labs were unremarkable. Colonoscopy revealed, a 5 mm sessile serrated
polyp in the cecum, 2 mm tubular adenoma in the ascending colon, and a 4 cm patch of
erythematous, friable, and nodular area with polypoid features in the rectum (Image 1).
Histopathology of the rectal lesion showed gastric oxyntic mucosa within benign rectal mucosa,
consistent with gastric heterotopia (Image 2). The patient was asymptomatic and was advised to
repeat colonoscopy in 5 years.
Discussion: Rectal GH is an exceptionally rare finding, believed to arise from aberrant embryologic
differentiation or post-inflammatory metaplasia. It is most frequently identified incidentally, but
symptoms—when present—can mimic colorectal neoplasia. Importantly, while GH is generally
benign, cases of dysplasia and even adenocarcinoma arising within ectopic gastric mucosa have
been reported, warranting long-term surveillance in some patients.
Interestingly, gastric heterotopia expresses functional parietal cells, capable of acid secretion. In
the rectum, this may cause local irritation, inflammation, and ulceration, possibly explaining
bleeding or tenesmus in symptomatic patients. Moreover, GH has been associated with
overexpression of mucin genes (MUC5AC and MUC6), which may play a role in mucosal
protection but could also contribute to neoplastic potential.
With fewer than 30 reported rectal GH cases in the literature, this case adds to the growing body
of knowledge suggesting that these lesions, though rare, should not be overlooked. Greater
awareness and histologic recognition are essential to differentiate them from malignancy and to
guide appropriate management.
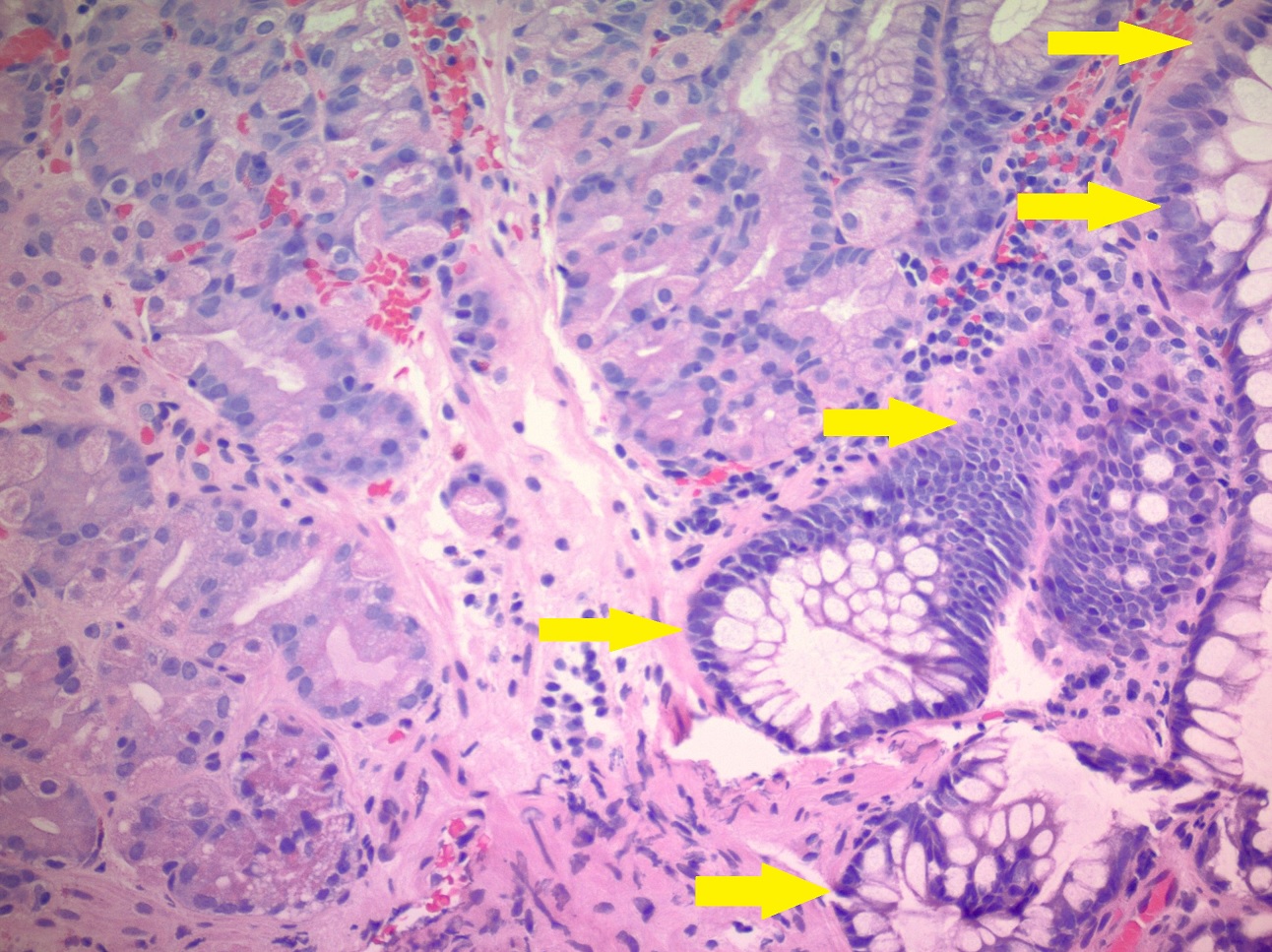
Figure: Image 1. Gastric Heterotopia seen on initial colonoscopy
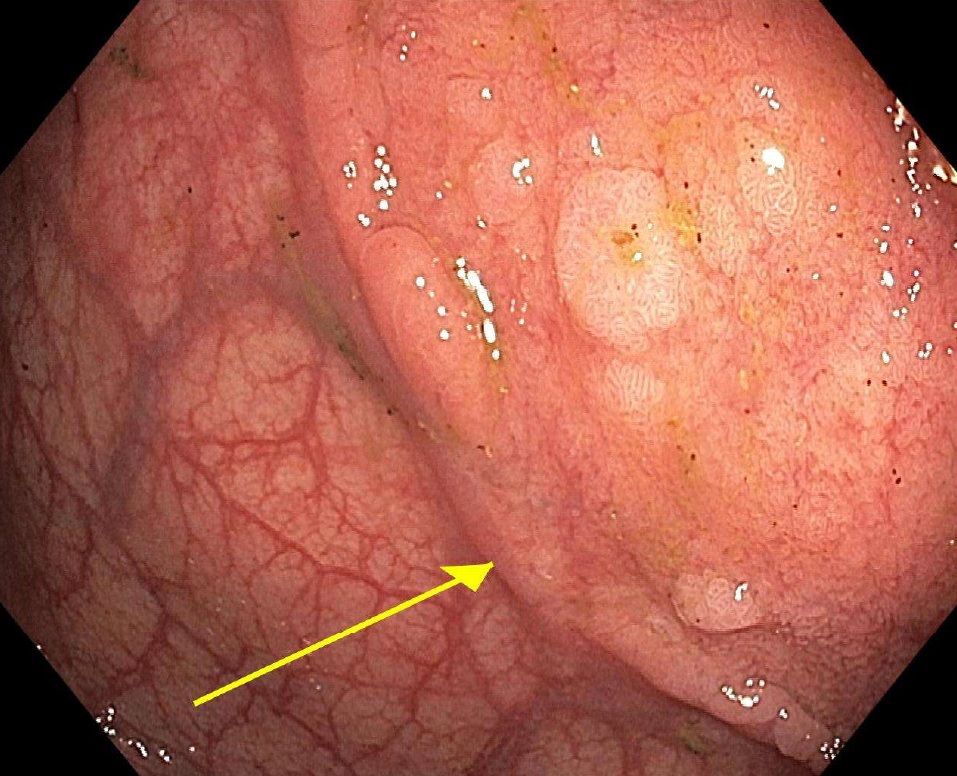
Figure: Image 2. H&E Stain, Rectal Biopsy
Disclosures:
Alexa Plato indicated no relevant financial relationships.
Cheng-Hung Tai indicated no relevant financial relationships.
Raquel Rozner indicated no relevant financial relationships.
Paul Cohen indicated no relevant financial relationships.
Alexa Plato, MD1, Cheng-Hung Tai, MD1, Raquel Rozner, MD2, Paul Cohen, MD1. P4618 - Heterotopia in Hindsight: A Stomach Where It Shouldn’t Be, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 2Yale School of Medicine, Gastroenterology Associates, PC, Northeast Medical Group/Yale New Haven Health, Stratford, CT
Introduction: Gastric heterotopia (GH) refers to the presence of gastric mucosa outside its normal anatomic
location. While GH is most commonly observed in the esophagus and duodenum, its occurrence
in the rectum is exceedingly rare, with limited case reports and unclear clinical implications.
Though often asymptomatic, GH has been associated with rectal bleeding, abdominal pain, and
potential malignant transformation.
Case Description/
Methods: A 45-year-old woman with a history of asthma, Graves’ disease, and migraines underwent
a routine screening colonoscopy. She reported intermittent constipation managed with docusate
but denied hematochezia, abdominal pain, weight loss, or family history of colorectal cancer.
Physical exam and labs were unremarkable. Colonoscopy revealed, a 5 mm sessile serrated
polyp in the cecum, 2 mm tubular adenoma in the ascending colon, and a 4 cm patch of
erythematous, friable, and nodular area with polypoid features in the rectum (Image 1).
Histopathology of the rectal lesion showed gastric oxyntic mucosa within benign rectal mucosa,
consistent with gastric heterotopia (Image 2). The patient was asymptomatic and was advised to
repeat colonoscopy in 5 years.
Discussion: Rectal GH is an exceptionally rare finding, believed to arise from aberrant embryologic
differentiation or post-inflammatory metaplasia. It is most frequently identified incidentally, but
symptoms—when present—can mimic colorectal neoplasia. Importantly, while GH is generally
benign, cases of dysplasia and even adenocarcinoma arising within ectopic gastric mucosa have
been reported, warranting long-term surveillance in some patients.
Interestingly, gastric heterotopia expresses functional parietal cells, capable of acid secretion. In
the rectum, this may cause local irritation, inflammation, and ulceration, possibly explaining
bleeding or tenesmus in symptomatic patients. Moreover, GH has been associated with
overexpression of mucin genes (MUC5AC and MUC6), which may play a role in mucosal
protection but could also contribute to neoplastic potential.
With fewer than 30 reported rectal GH cases in the literature, this case adds to the growing body
of knowledge suggesting that these lesions, though rare, should not be overlooked. Greater
awareness and histologic recognition are essential to differentiate them from malignancy and to
guide appropriate management.
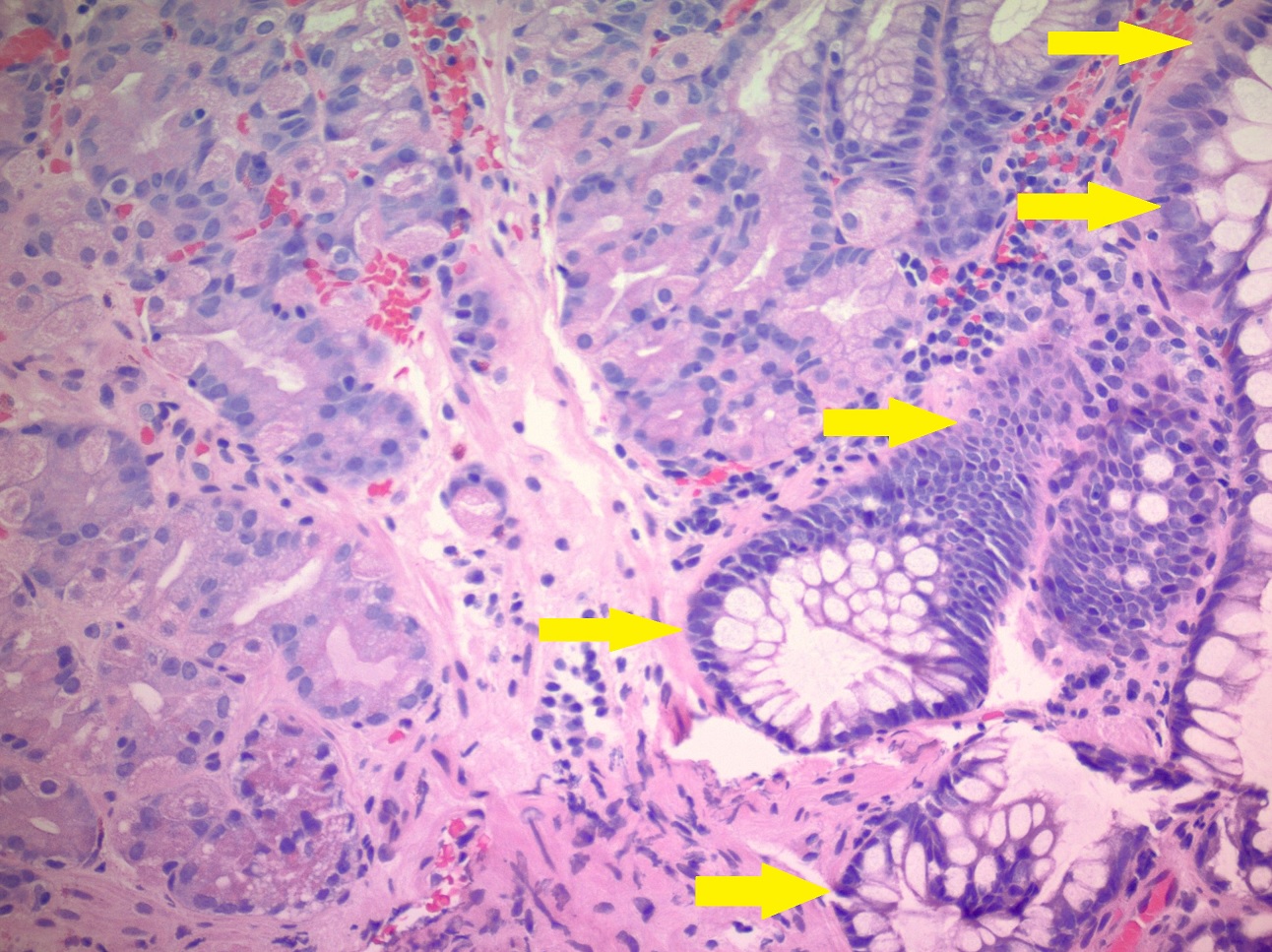
Figure: Image 1. Gastric Heterotopia seen on initial colonoscopy
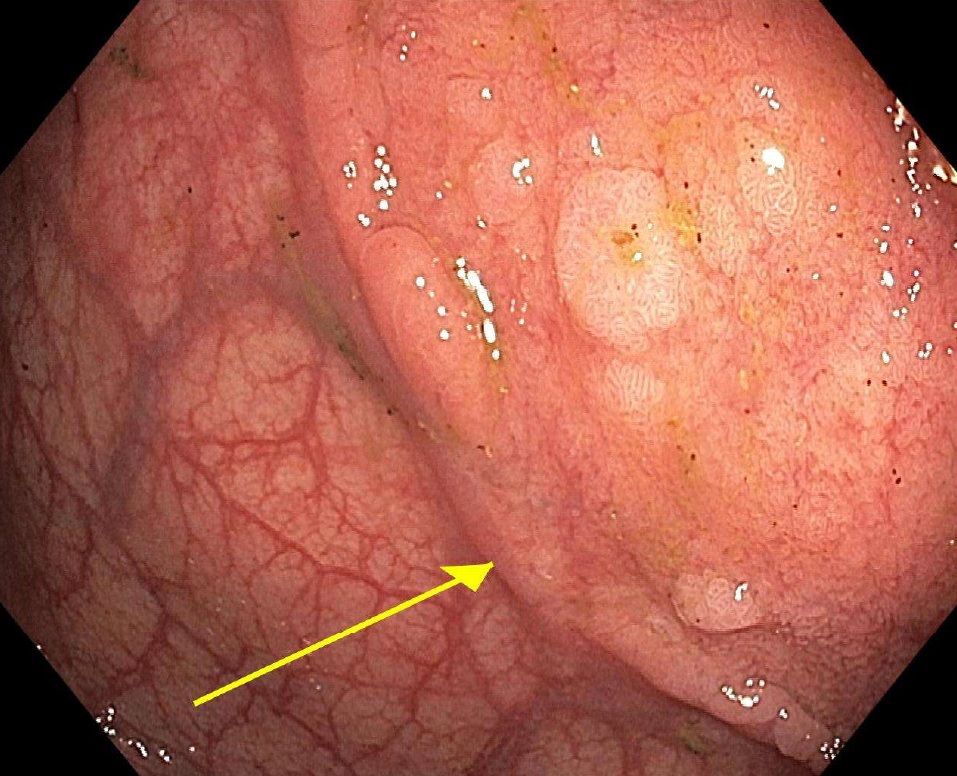
Figure: Image 2. H&E Stain, Rectal Biopsy
Disclosures:
Alexa Plato indicated no relevant financial relationships.
Cheng-Hung Tai indicated no relevant financial relationships.
Raquel Rozner indicated no relevant financial relationships.
Paul Cohen indicated no relevant financial relationships.
Alexa Plato, MD1, Cheng-Hung Tai, MD1, Raquel Rozner, MD2, Paul Cohen, MD1. P4618 - Heterotopia in Hindsight: A Stomach Where It Shouldn’t Be, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
