Tuesday Poster Session
Category: Colon
P4587 - Obesity and Sociodemographic Patterns in Early vs Late-Onset Colorectal Cancer Hospitalizations
- MS
Manali Shah, MD
Rutgers New Jersey Medical School
Newark, NJ
Presenting Author(s)
1Rutgers New Jersey Medical School, Newark, NJ; 2Rutgers New Jersey Medical School, New York, NY; 3Rutgers Cancer Institute of New Jersey, Newark, NJ
Introduction: The incidence of early-onset colorectal cancer (EOCRC), defined as diagnosis before age 50, is rising despite a decline in overall colorectal cancer (CRC) rates. EOCRC presents unique clinical challenges and disparities, with emerging evidence linking obesity and sociodemographic factors to increased risk. The objective focus of this study was to compare hospitalization trends, length of stay, inpatient mortality, and sociodemographic disparities between EOCRC and late-onset CRC (LOCRC), with particular focus on the role of obesity.
Methods: We analyzed data from the National Inpatient Sample (2016–2020) for hospitalizations with a primary diagnosis of CRC. Patients were classified as EOCRC (< 50 years) or LOCRC (≥50 years). Multivariate logistic regression evaluated associations between BMI, demographics, and inpatient outcomes including mortality, length of stay (LOS), and inpatient chemotherapy use.
Results:
A total of 246,231 inpatient hospitalizations with a primary diagnosis of colorectal cancer (CRC) were identified. Of these, 33,662 (13.7%) were classified as EOCRC, while 212,569 (86.3%) were classified as LOCRC. EOCRC patients were more likely to be female (OR 1.09, p< 0.001), Black (OR 1.17), Hispanic (OR 1.56), or Asian (OR 1.29) compared to White patients (p< 0.001 for all). They were also more likely to have Medicaid, private insurance, or be uninsured, while LOCRC patients were predominantly Medicare-insured. Obesity was significantly associated with EOCRC in patients with BMI 30–39 (OR 1.08, p=0.008) and BMI ≥40 (OR 1.52, p< 0.001). Conversely, LOCRC showed that patients with a BMI 30-39 (OR 0.92, p=0.008) and BMI ≥40 (OR 0.656, p< 0.001). EOCRC patients had higher rates of tobacco use disorder (OR 1.25), depression (OR 1.14), and lower rates of diabetes, CAD, and alcohol use disorder. EOCRC patients had slightly shorter LOS (6.01 vs. 6.66 days) and lower inpatient mortality (OR 0.649, p< 0.001). Inpatient chemotherapy use was more likely in patients with EOCRC (OR 1.75, p< 0.001).
Discussion:
EOCRC patients demonstrate distinct demographic, clinical, and inpatient profiles compared to LOCRC patients, with obesity, race, and insurance status playing key roles. The increased burden among younger, racially diverse, and uninsured populations underscores the need for early screening, risk stratification, and targeted prevention strategies. These findings reinforce changes in CRC screening guidelines and call for further research into the biological and social drivers of EOCRC.
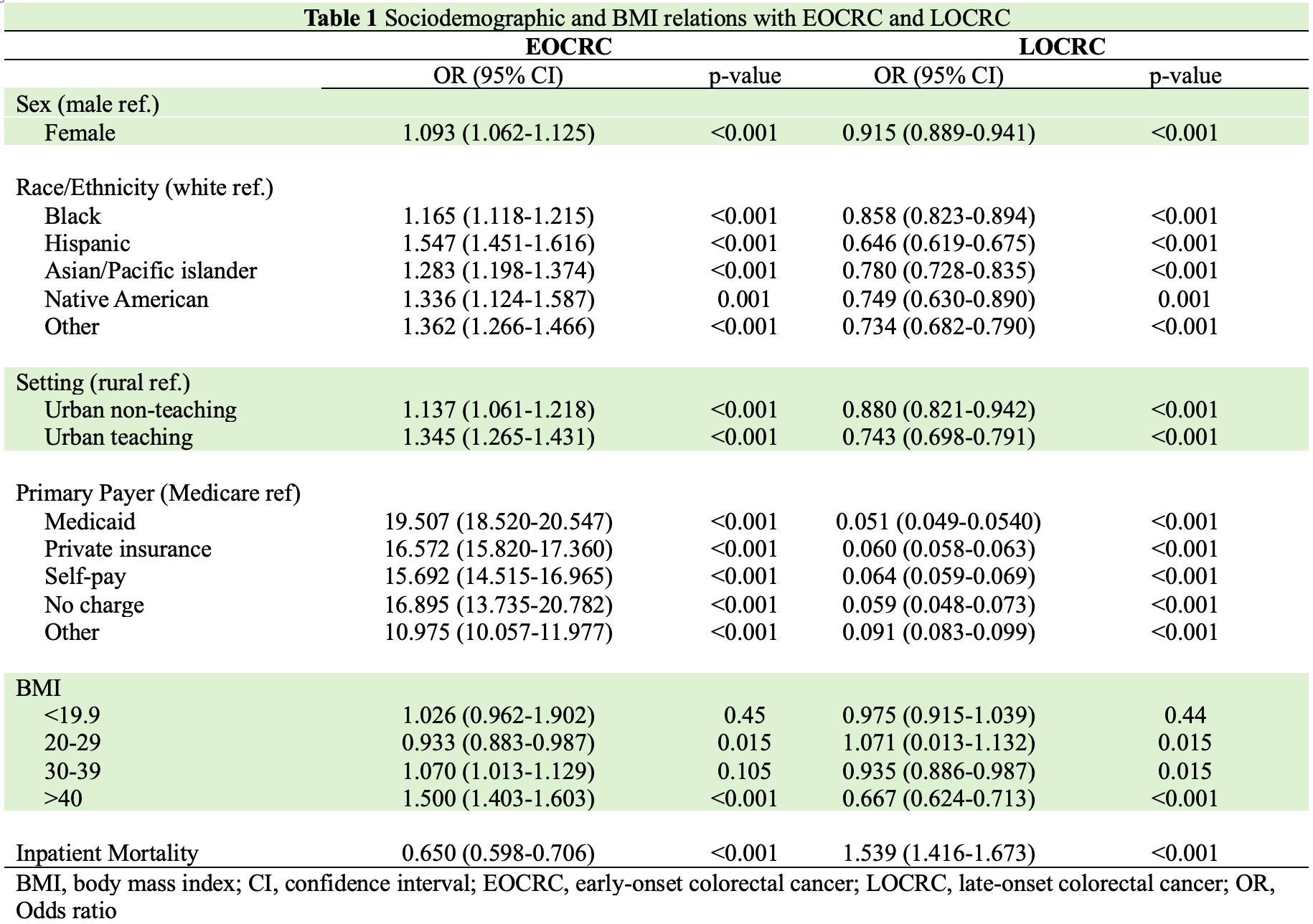
Figure: Sociodemographic and BMI relationships with EOCRC and LOCRC
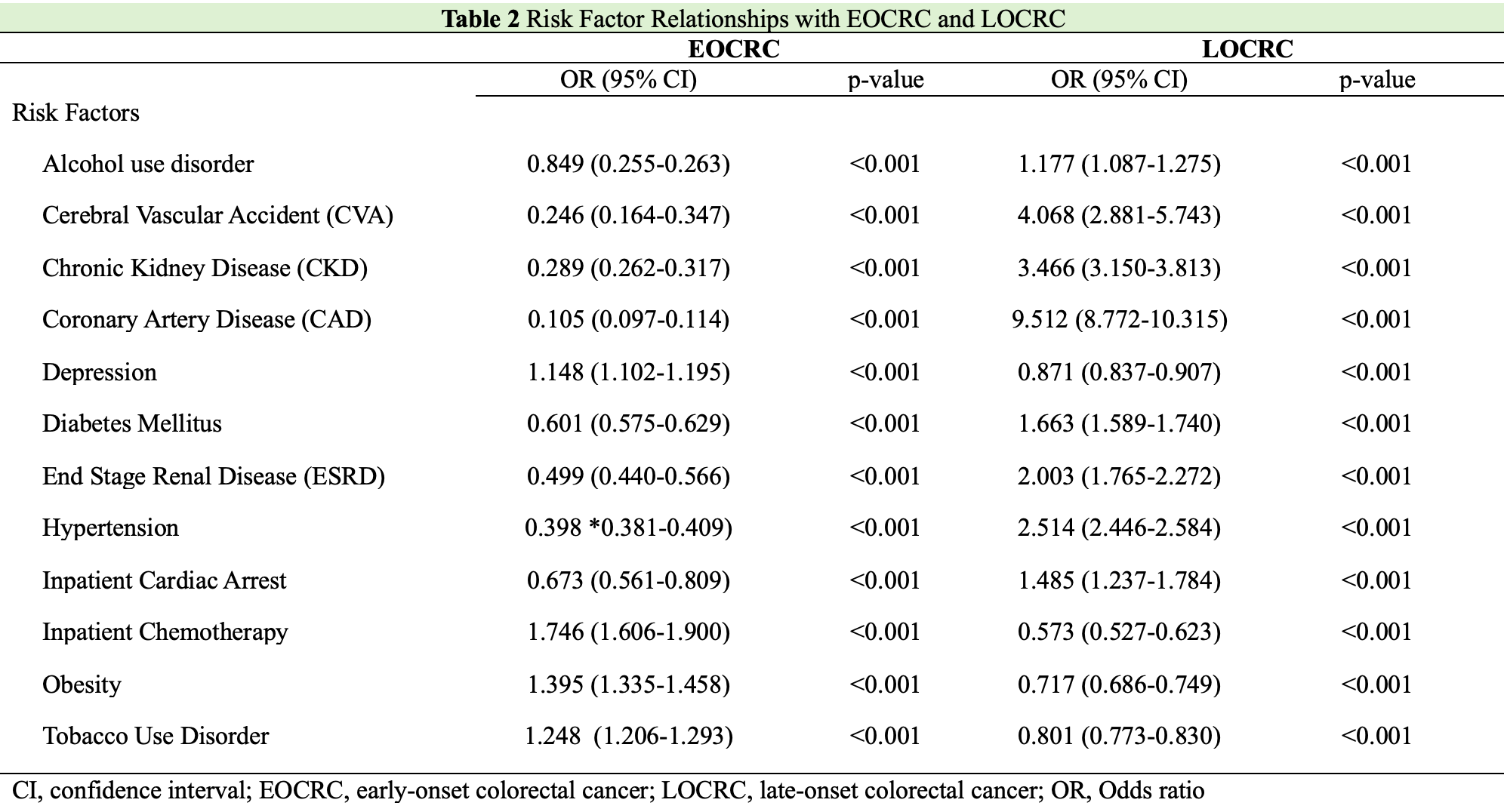
Figure: Risk factor relationships with EOCRC and LOCRC
Disclosures:
Manali Shah indicated no relevant financial relationships.
Ravi Upadhyay indicated no relevant financial relationships.
Lawanya Singh indicated no relevant financial relationships.
Sharon Li: AstraZeneca – Advisory Committee/Board Member.
Manali Shah, MD1, Ravi Upadhyay, MD1, Lawanya Singh, MD2, Sharon Li, MD3. P4587 - Obesity and Sociodemographic Patterns in Early vs Late-Onset Colorectal Cancer Hospitalizations, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
