Tuesday Poster Session
Category: Colon
P4579 - Trends and Disparities in Diverticular Disease Mortality in the United States Between 1999-2020

Samiksha Jain, MBBS (she/her/hers)
Guntur Medical College, India
Guntur, Andhra Pradesh, India
Presenting Author(s)
1St Francis Medical Center, Monroe, LA, Mumbai, Maharashtra, India; 2Guntur Medical College, India, Guntur, Andhra Pradesh, India; 3Al-Tibri Medical College, Karachi, Sindh, Pakistan; 4Detroit Medical Center Sinai Grace Hospital, Detroit, MI; 5Case Western Reserve University / MetroHealth, Cleveland, OH
Introduction:
Over the past two decades, there has been an increase in the incidence of diverticular disease in the United States, however, mortality data remain unexplored. This study aims to analyze temporal trends and demographic disparities in diverticular disease mortality in American adults aged 45 years and older from 1999-2020.
Methods:
Retrospective analysis of the Centers for Disease Control and Prevention's Wide-Ranging Online Data for Epidemiologic Research database was conducted. Mortality related to diverticular disease was identified using the ICD-10 code K57. Age-adjusted mortality rates (AAMRs) and crude death rates (CDRs) per 100,000 persons were calculated. Trends were analyzed using Joinpoint regression to determine average annual percentage change (AAPC). Temporal trends were analyzed in terms of sex, race, geographical distribution, and patient age-related mortality. Despite significant overall decline in diverticular disease mortality between 1999 and 2020, notable disparities persist. Females, NH Whites, residents of West, and nonmetropolitan areas experienced disproportionately higher mortality rates. These findings highlight the need for targeted public health efforts to reduce mortality in high-risk populations.
Results: A total of 66,632 deaths were reported. Overall AAMR was 2.58, with a statistically significant AAPC of -2.51 (p< 0.001). Females had a higher AAMR (2.91 vs. 2.06) but a smaller decline in mortality compared to males (AAPC:-2.45 vs. -2.60;p< 0.001 for both). When stratified by race, the highest AAMR was observed for non-Hispanic (NH) Whites (2.76), followed by NH Black/African Americans (2.2), Hispanic/Latino individuals (1.92), NH American Indian/Alaska Natives (1.8), and NH Asian/Pacific Islanders (0.88). All races experienced statistically significant declines in AAMR, with the greatest decline noted among Hispanics (AAPC:-3.28;p< 0.001). Geographically, the highest AAMR was reported in West (2.82) and Midwest (2.68). AAMRs declined across all census regions, with West experiencing the steepest decrease (AAPC:-3.15;p< 0.001). AAMR was higher in nonmetropolitan areas (3.03) compared to metropolitan areas (2.49), though both showed similar rates of decline (nonmetropolitan AAPC:-2.56; metropolitan AAPC:-2.52;p< 0.001 for both). CDR was highest in adults aged 85 and older (22.9). While all 10-year age groups saw a decline in CDR, the most significant drop was also seen in this age group (AAPC:-3.05;p< 0.001).
Discussion: 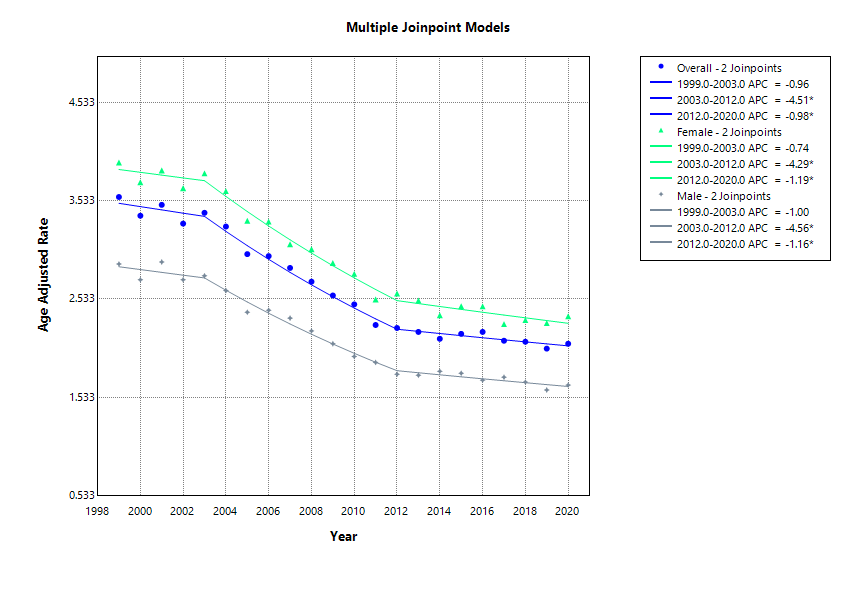
Figure: Trends in diverticular disease mortality (overall and for each sex) from 1999-2020.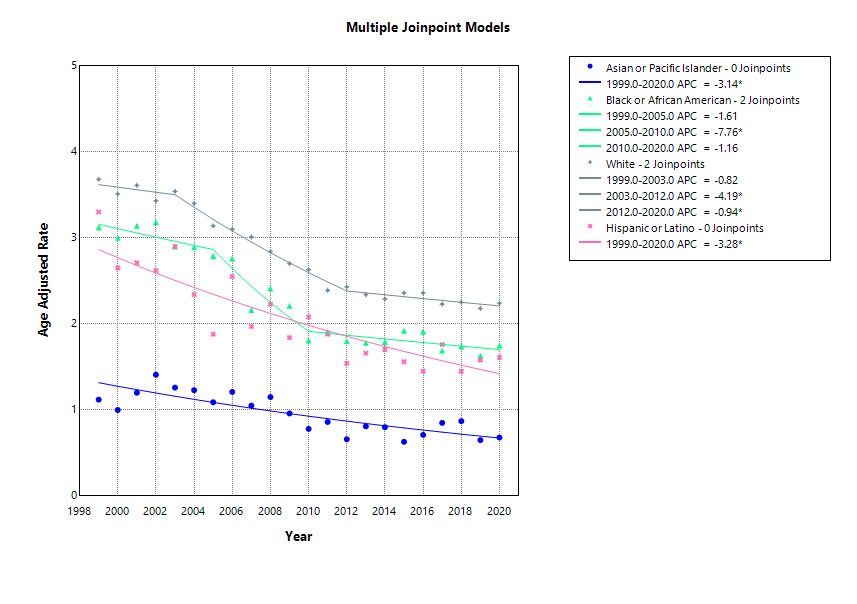
Figure: Trends in diverticular disease mortality for each racial group from 1999-2020.
Disclosures:
Dhruv Gandhi indicated no relevant financial relationships.
Samiksha Jain indicated no relevant financial relationships.
Wajdan Ahmad indicated no relevant financial relationships.
Ayesha Cheema indicated no relevant financial relationships.
Shamitha Hejmadi indicated no relevant financial relationships.
Rishi Chowdhary indicated no relevant financial relationships.
Dhruv Gandhi, MD1, Samiksha Jain, MBBS2, Wajdan Ahmad, MBBS3, Ayesha Cheema, MBBS3, Shamitha Hejmadi, MD4, Rishi Chowdhary, MD5. P4579 - Trends and Disparities in Diverticular Disease Mortality in the United States Between 1999-2020, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
