Tuesday Poster Session
Category: Colon
P4544 - Performance of a Modified Ideomotor Apraxia Test in Patients With Constipation and Dyssynergic Pattern and Dyssynergic Defecation Compared to Healthy Volunteers

Josealberto S. Arenas-Martinez, MD
Instituto Nacional de Ciencias Medicas y Nutricion Salvador Zubiran
Mexico City, Distrito Federal, Mexico
Presenting Author(s)
1Instituto Nacional de Ciencias Medicas y Nutricion Salvador Zubiran, Mexico City, Distrito Federal, Mexico; 2Instituo Nacional de Ciencias Médicas y Nutrición Salvador Zubiran, Ciudad de Mexico, Distrito Federal, Mexico; 3INCMNSZ, México, San Luis Potosi, Mexico
Introduction:
Dyssynergic defecation (DD) is characterized by impaired coordination of rectal propulsive force and/or pelvic floor relaxation. Its pathophysiology remains unclear, but factors such as lack of childhood learning or loss of execution ability have been proposed. While ideomotor apraxia tests are validated in other settings, no clinical tools exist for DD, motivating this pilot study to evaluate ideomotor apraxia in DD. The objective was to compare the performance of patients with DD in a modified ideomotor apraxia test with healthy volunteers (HV).
Methods:
Cross-sectional comparative study. Consecutive patients referred for high-resolution anorectal manometry due to functional constipation and DD were recruited. HV without gastrointestinal or neurological symptoms were invited to participate. The modified ideomotor apraxia test included seven categories: 1) gesture imitation (0–8 points), 2) execution of a verbal command (0–8 points), 3) gesture recognition (0–2 points), 4) gesture evaluation (0–4 points), 5) description of a real object (0–4 points), 6) execution of an activity using real objects (0–4 points), and 7) imitation of thoracic and diaphragmatic breathing (0–6 points). Higher scores indicated better performance. A single researcher administered the test. Demographic, clinical, and manometric data were collected. Mann-Whitney U and Fisher's exact tests were used for comparisons.
Results:
A total of 30 patients with DD (22 women, median age 56.5 years) and 60 HV (39 women, median age 55.5 years) were included. The DD group had a median BMI of 25 vs. 27.3 in HV (p = 0.020). Group A was divided into Group A1 (failed balloon expulsion, n=11) and Group A2 (successful expulsion, n=19). DD patients scored lower than HV in gesture imitation, verbal command execution, and breathing imitation (table 1). Median total score was 28 (26–30.8) in DD vs. 34 (32–35.3) in HV (p < 0.001), see Figure 1. Two patients with neurological comorbidities had the lowest scores (16 and 21 points). No significant differences were found between A1 and A2, but both differed from HV (p < 0.001).
Discussion:
Patients with DD had significantly lower ideomotor apraxia test scores than HV, regardless of balloon expulsion results, suggesting a link between ideomotor apraxia and DD. This pilot study demonstrates the importance of incorporating neurological evaluations in patients with DD for a better understanding of its pathophysiology and management.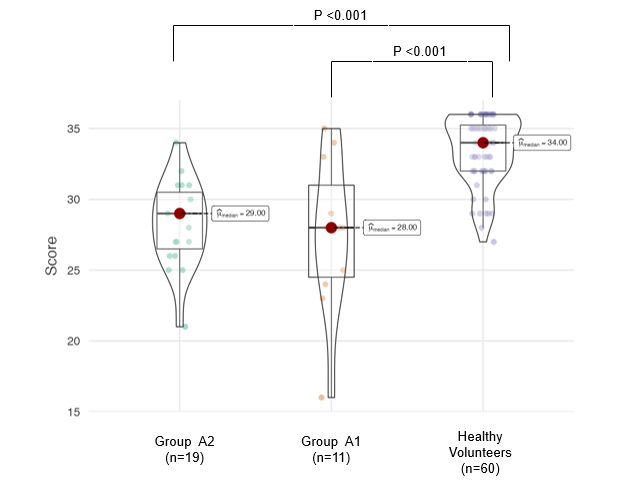
Figure: Figure 1. Comparison of Total Scores on the Modified Ideomotor Apraxia Test Between Patients with Dyssynergic Defecation and Healthy Volunteers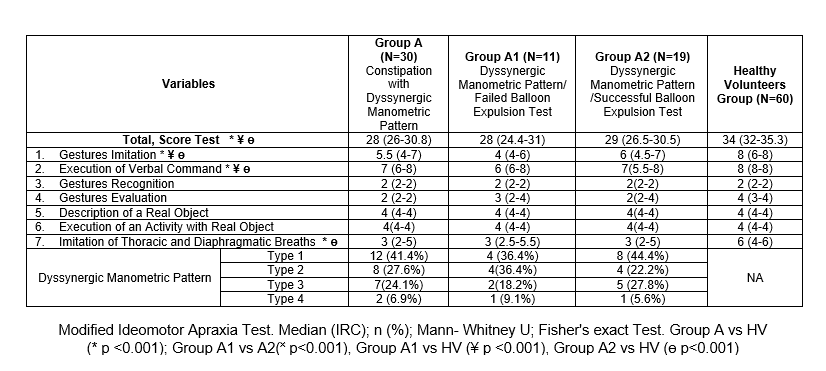
Figure: Table 1. Median Scores for Each Item of the Modified Ideomotor Apraxia Test in Patients with Dyssynergic Defecation and Healthy Volunteers
Disclosures:
Abigal Fuentes-Montalvo indicated no relevant financial relationships.
Josealberto Arenas-Martinez indicated no relevant financial relationships.
Ana Ordoñez-Vazquez indicated no relevant financial relationships.
Enrique Coss-Adame indicated no relevant financial relationships.
Daniel Carmona-Guerrero indicated no relevant financial relationships.
Abigal Fuentes-Montalvo, MD1, Josealberto S. Arenas-Martinez, MD1, Ana Ordoñez-Vazquez, MD2, Enrique Coss-Adame, MD1, Daniel Carmona-Guerrero, 3. P4544 - Performance of a Modified Ideomotor Apraxia Test in Patients With Constipation and Dyssynergic Pattern and Dyssynergic Defecation Compared to Healthy Volunteers, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
