Tuesday Poster Session
Category: Colon
P4537 - Analysis of Mortality Patterns in Chronic Vascular Diseases of the Intestine Using CDC WONDER Data (1999–2020)

Ammad Javaid Chaudhary, MD
Henry Ford Health
Detroit, MI
Presenting Author(s)
1Brigham and Women's Hospital, Boston, MA; 2Henry Ford Health, Detroit, MI; 3King Edward Medical University, Lahore, Punjab, Pakistan; 4Nawaz Sharif Medical College, Lahore, Punjab, Pakistan; 5Dow University of Health Sciences, Karachi, Sindh, Pakistan; 6Services Institute of Medical Sciences, Lahore, Punjab, Pakistan
Introduction:
Chronic vascular disorders of the intestine, such as chronic mesenteric ischemia and ischemic colitis, are rare but can lead to high mortality if untreated. This study examines mortality trends in U.S. adults aged 25+ from 1999 to 2020, stratified by demographics, to inform early recognition and intervention strategies. Although mortality from intestinal vascular diseases has declined over the past two decades, persistent disparities—especially among women, non-Hispanic Blacks, and those in rural and Western regions—highlight the need for targeted public health interventions and policy reforms. AI tools were used to enhance writing clarity.
Methods: CDC WONDER mortality data (1999–2020) were retrospectively analyzed. Age-adjusted mortality rates (AAMRs) per 100,000 for liver metastasis were calculated. Trends were assessed by Annual Percent Change (APC), stratified by age, sex, race/ethnicity, and region.
Results: From 1999 to 2020, intestinal vascular diseases caused 254,535 deaths among U.S. adults aged 25 and older. The age-adjusted mortality rate (AAMR) declined from 5.29 to 4.73, with four trend periods: an initial increase (1999–2001, APC: 6.4), continued rise (2001–2005), a long decline (2005–2018, APC: -2.2), and a slight reversal (2018–2020, APC: 1.7). Women had higher AAMRs than men (5.66 vs. 4.81). Among women, trends mirrored the overall pattern, with a recent uptick from 2018–2020 (APC: 0.4). Racial disparities were evident, with non-Hispanic Blacks showing the highest AAMR (6.07; AAPC: -0.9), followed by non-Hispanic Whites (5.41; AAPC: -0.5), Hispanics (4.47; AAPC: -1.4), and other non-Hispanic races (3.41; AAPC: -0.3). Regionally, all U.S. areas showed declining AAMRs, with the Northeast leading (AAPC: -0.9). Rural areas had slightly higher AAMRs than urban ones (5.61 vs. 5.28), with rural mortality increasing (AAPC: 0.8) while urban areas declined (AAPC: -0.9). Rhode Island had the highest state-level AAMR (7.4), while Hawaii had the lowest (3.3). Mortality increased with age, peaking in those aged 85+ (crude rate: 63.19), and was lowest in ages 25–34 (0.11). Most deaths (85.2%) occurred in medical facilities, followed by nursing homes (6%) and private residences (4%).
Discussion: 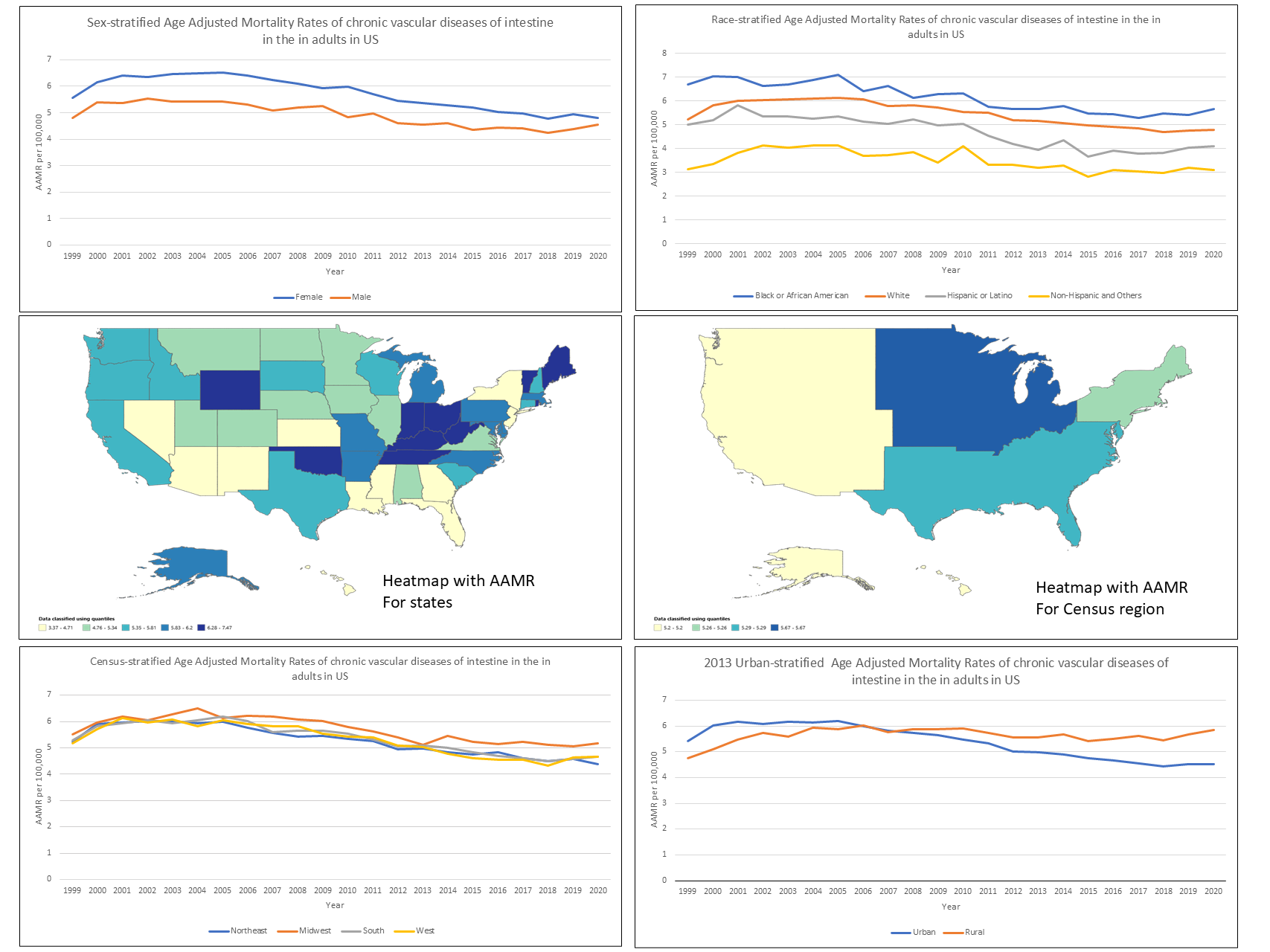
Figure: Trends in age-adjusted mortality rates (AAMRs) for chronic vascular diseases of the intestine-related deaths among patients with hepatic neoplasms in the U.S. (1999–2020), stratified by region, age, sex, race/ethnicity, urbanisation, and state-level distribution.
Disclosures:
Hafsa Shahid indicated no relevant financial relationships.
Ammad Chaudhary indicated no relevant financial relationships.
Fatima Sial indicated no relevant financial relationships.
Muhammad Ubaid Hussain indicated no relevant financial relationships.
Rimsha Adnan indicated no relevant financial relationships.
Mudasar Nisar indicated no relevant financial relationships.
Syed-Mohammed Jafri: Abbvie – Speakers Bureau. Gilead – Speakers Bureau. Intercept – Speakers Bureau. Ironwood – Speakers Bureau. Takeda – Speakers Bureau.
Hafsa Shahid, MD1, Ammad Javaid. Chaudhary, MD2, Fatima Sial, MBBS3, Muhammad Ubaid Hussain, 4, Rimsha Adnan, 5, Mudasar Nisar, 6, Syed-Mohammed Jafri, MD2. P4537 - Analysis of Mortality Patterns in Chronic Vascular Diseases of the Intestine Using CDC WONDER Data (1999–2020), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
