Tuesday Poster Session
Category: Biliary/Pancreas
P4522 - Hepatic Artery Pseudoaneurysm Secondary due to Severe Acute Pancreatitis: A Rare but Fatal Vascular Complication
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mohamad Besher Adi, MD (he/him/his)
Ascension St. John Hospital
St. Clair Shores, MI
Presenting Author(s)
Muhammad Ismail, MD1, Mohamad Besher Adi, MD2, Baraa Alhallak Tonbr, MD3, Nafea Zayouna, MD4, Jacob Klein, MD5, Reham Haroun, MD6, Mohammed Barawi, MD7
1Henry Ford Health, Warren, MI; 2Ascension St. John Hospital, St. Clair Shores, MI; 3Henry Ford Health, Madison Heights, MI; 4Henry Ford, Warren, Michigan, Clinton Township, MI; 5Ascension Macomb-Oakland Hospital, Warren, MI; 6Henry Ford Warren, Warren, MI; 7Henry Ford Health, Detroit, MI
Introduction: Acute pancreatitis can result in a range of vascular complications, with venous thrombosis and arterial pseudoaneurysms among the most serious. While splenic artery pseudoaneurysms are more commonly encountered, hepatic artery pseudoaneurysms (HAPA) are rare and life-threatening, typically caused by enzymatic injury to arterial walls. Clinical manifestations may include hemobilia, gastrointestinal bleeding, or hemodynamic instability, making early detection crucial.
Case Description/
Methods:
A 66-year-old woman with mixed hyperlipidemia, obesity, radiation-induced esophageal strictures, and stage IV non-small cell lung carcinoma (on Lorlatinib since April 2023) presented with severe epigastric pain radiating to the back, nausea, and vomiting. Laboratory findings revealed a lipase >3000 IU/L and AST 57 IU/L. CTA demonstrated extensive peripancreatic inflammation consistent with acute pancreatitis. RUQ ultrasound showed cholelithiasis, while MRCP was unremarkable. The patient was managed conservatively and discharged with plans for outpatient laparoscopic cholecystectomy.
Four days later, she returned with recurrent epigastric pain, nausea, and vomiting. Labs showed lipase 1995 IU/L, ALP 182, AST 112, ALT 42. Repeat MRCP revealed a new hepatic artery pseudoaneurysm, confirmed on CTA as a 10 mm pseudoaneurysm in the right hepatic lobe.
Digital subtraction angiography identified long-segment aneurysms in branches of the right hepatic artery and a short-segment aneurysm in the segment 4 branch of the left hepatic artery. Successful endovascular coil embolization was performed without complications. The patient recovered well and was discharged on hospital day 7, with a cholecystectomy planned in 3 weeks.
Discussion: HAPA is a rare but serious complication of acute pancreatitis, often resulting from inflammatory extension or enzymatic degradation of the arterial wall. Given the high risk of rupture and bleeding, prompt diagnosis is essential. CTA is the preferred non-invasive imaging modality, while digital subtraction angiography is the gold standard for both diagnosis and treatment. Endovascular embolization is minimally invasive and highly effective. HAPA should be considered in pancreatitis patients with new-onset GI bleeding, unexplained anemia, or hemodynamic changes.
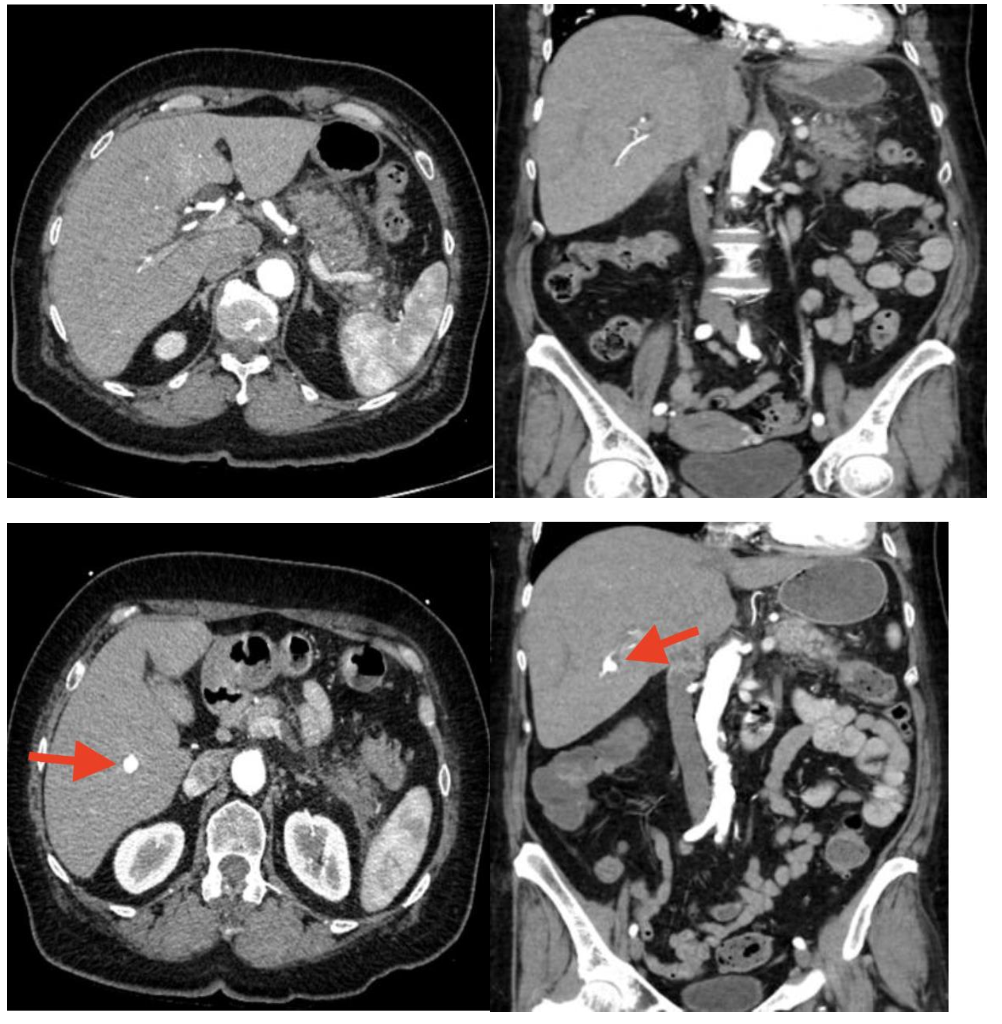
Figure: CTA from first admission (upper panel). CTA from second admission with newly developed HAPA (lower panel)
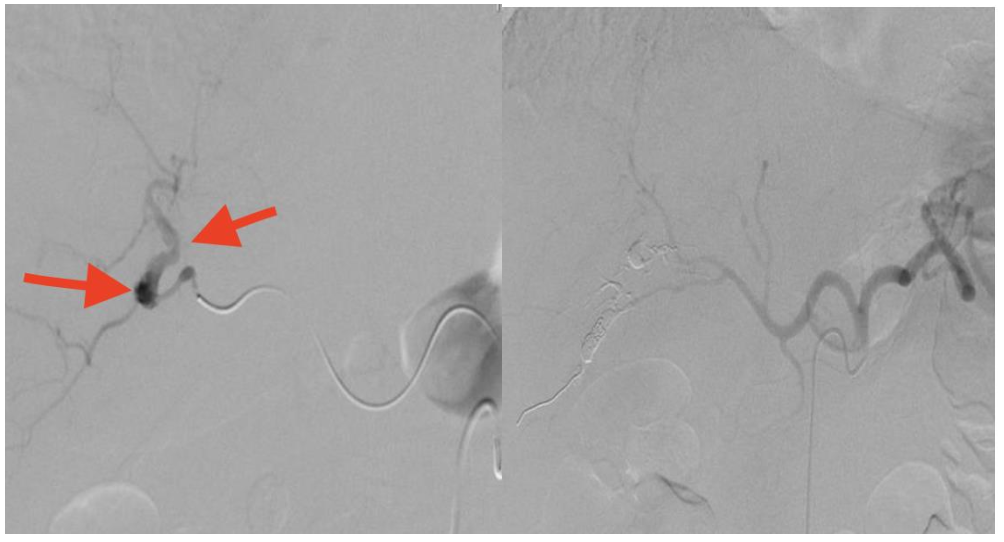
Figure: Digital subtraction angiography shows long segment aneurysm of the two branches of the right hepatic artery and short segment aneurysm involving segment 4th branch of the left hepatic artery (left). Post embolization (Right)
Disclosures:
Muhammad Ismail indicated no relevant financial relationships.
Mohamad Besher Adi indicated no relevant financial relationships.
Baraa Alhallak Tonbr indicated no relevant financial relationships.
Nafea Zayouna indicated no relevant financial relationships.
Jacob Klein indicated no relevant financial relationships.
Reham Haroun indicated no relevant financial relationships.
Mohammed Barawi indicated no relevant financial relationships.
Muhammad Ismail, MD1, Mohamad Besher Adi, MD2, Baraa Alhallak Tonbr, MD3, Nafea Zayouna, MD4, Jacob Klein, MD5, Reham Haroun, MD6, Mohammed Barawi, MD7. P4522 - Hepatic Artery Pseudoaneurysm Secondary due to Severe Acute Pancreatitis: A Rare but Fatal Vascular Complication, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Henry Ford Health, Warren, MI; 2Ascension St. John Hospital, St. Clair Shores, MI; 3Henry Ford Health, Madison Heights, MI; 4Henry Ford, Warren, Michigan, Clinton Township, MI; 5Ascension Macomb-Oakland Hospital, Warren, MI; 6Henry Ford Warren, Warren, MI; 7Henry Ford Health, Detroit, MI
Introduction: Acute pancreatitis can result in a range of vascular complications, with venous thrombosis and arterial pseudoaneurysms among the most serious. While splenic artery pseudoaneurysms are more commonly encountered, hepatic artery pseudoaneurysms (HAPA) are rare and life-threatening, typically caused by enzymatic injury to arterial walls. Clinical manifestations may include hemobilia, gastrointestinal bleeding, or hemodynamic instability, making early detection crucial.
Case Description/
Methods:
A 66-year-old woman with mixed hyperlipidemia, obesity, radiation-induced esophageal strictures, and stage IV non-small cell lung carcinoma (on Lorlatinib since April 2023) presented with severe epigastric pain radiating to the back, nausea, and vomiting. Laboratory findings revealed a lipase >3000 IU/L and AST 57 IU/L. CTA demonstrated extensive peripancreatic inflammation consistent with acute pancreatitis. RUQ ultrasound showed cholelithiasis, while MRCP was unremarkable. The patient was managed conservatively and discharged with plans for outpatient laparoscopic cholecystectomy.
Four days later, she returned with recurrent epigastric pain, nausea, and vomiting. Labs showed lipase 1995 IU/L, ALP 182, AST 112, ALT 42. Repeat MRCP revealed a new hepatic artery pseudoaneurysm, confirmed on CTA as a 10 mm pseudoaneurysm in the right hepatic lobe.
Digital subtraction angiography identified long-segment aneurysms in branches of the right hepatic artery and a short-segment aneurysm in the segment 4 branch of the left hepatic artery. Successful endovascular coil embolization was performed without complications. The patient recovered well and was discharged on hospital day 7, with a cholecystectomy planned in 3 weeks.
Discussion: HAPA is a rare but serious complication of acute pancreatitis, often resulting from inflammatory extension or enzymatic degradation of the arterial wall. Given the high risk of rupture and bleeding, prompt diagnosis is essential. CTA is the preferred non-invasive imaging modality, while digital subtraction angiography is the gold standard for both diagnosis and treatment. Endovascular embolization is minimally invasive and highly effective. HAPA should be considered in pancreatitis patients with new-onset GI bleeding, unexplained anemia, or hemodynamic changes.
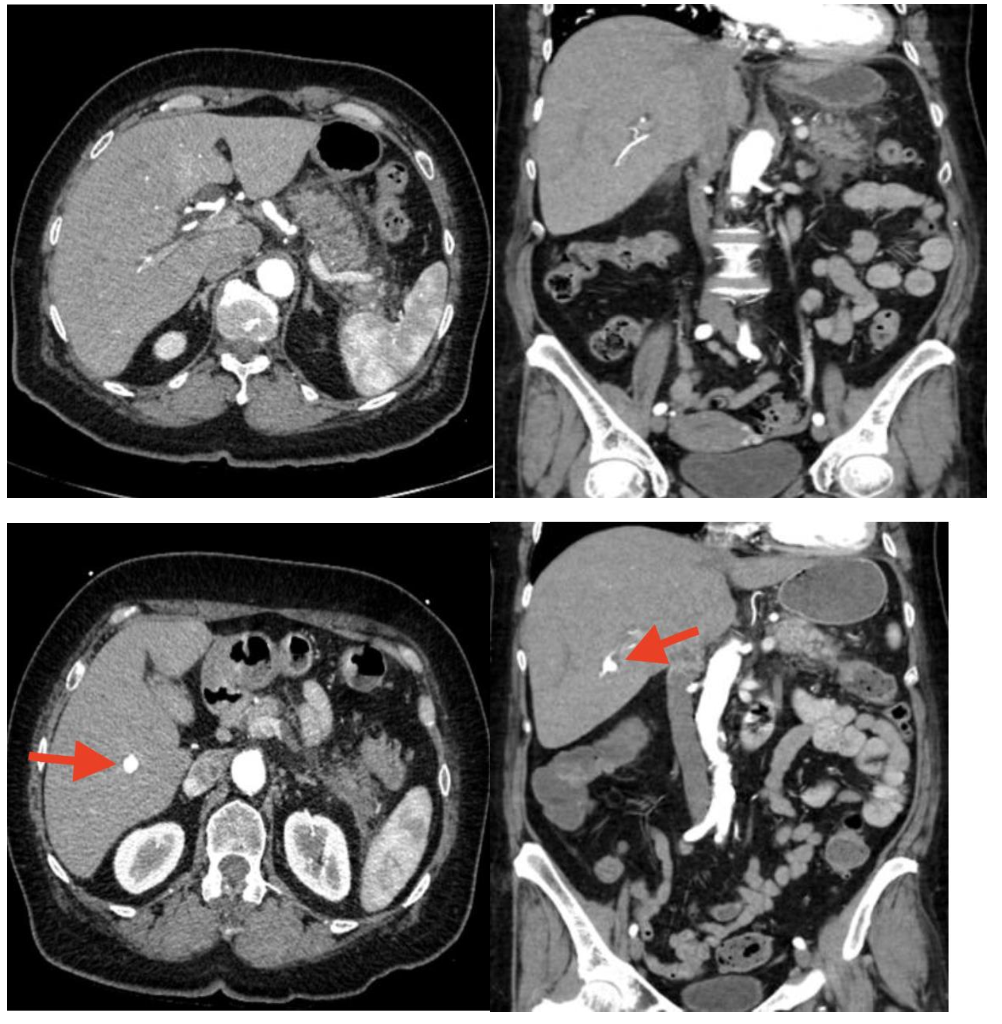
Figure: CTA from first admission (upper panel). CTA from second admission with newly developed HAPA (lower panel)
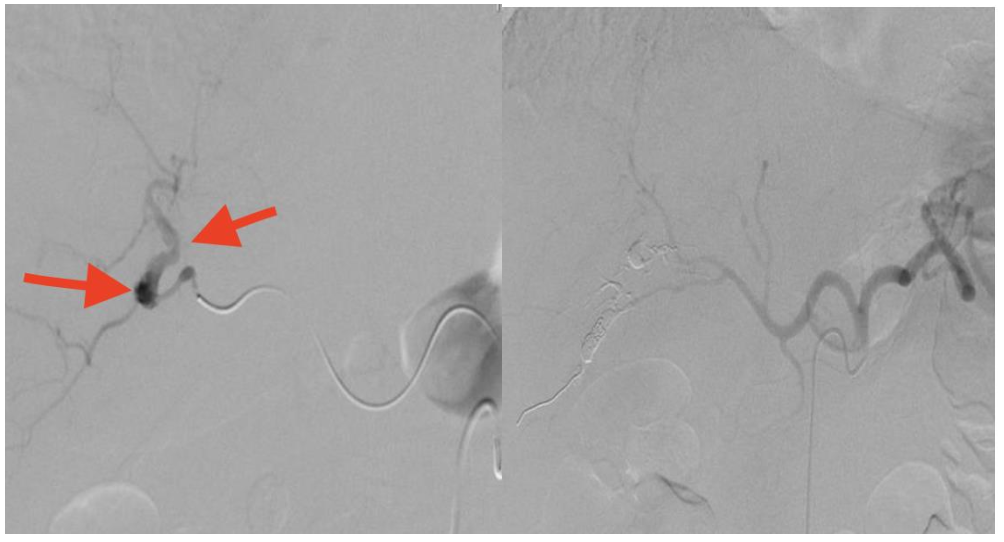
Figure: Digital subtraction angiography shows long segment aneurysm of the two branches of the right hepatic artery and short segment aneurysm involving segment 4th branch of the left hepatic artery (left). Post embolization (Right)
Disclosures:
Muhammad Ismail indicated no relevant financial relationships.
Mohamad Besher Adi indicated no relevant financial relationships.
Baraa Alhallak Tonbr indicated no relevant financial relationships.
Nafea Zayouna indicated no relevant financial relationships.
Jacob Klein indicated no relevant financial relationships.
Reham Haroun indicated no relevant financial relationships.
Mohammed Barawi indicated no relevant financial relationships.
Muhammad Ismail, MD1, Mohamad Besher Adi, MD2, Baraa Alhallak Tonbr, MD3, Nafea Zayouna, MD4, Jacob Klein, MD5, Reham Haroun, MD6, Mohammed Barawi, MD7. P4522 - Hepatic Artery Pseudoaneurysm Secondary due to Severe Acute Pancreatitis: A Rare but Fatal Vascular Complication, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
