Tuesday Poster Session
Category: Biliary/Pancreas
P4510 - Low Phospholipid-Associated Cholelithiasis Syndrome Presenting as Recurrent Cholangitis Post-Cholecystectomy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Amine Rakab, MD (he/him/his)
Division of Medical Education, Weill Cornell Medicine
Doha, Ad Dawhah, Qatar
Presenting Author(s)
Faris Bandar Alrashdan, MD1, Ramy Mahmoud Fathy Elbarody, BS2, Bisher Sawaf, MD3, Amine Rakab, MD4, Lanah Almatroud, BS5, Mahmoud Salah Abdalhakeem Mohammed, MD6, Haidara Bohsas, MD7, Yusuf Omar Hallak, MD8, Atheer Abdullah Ali Aldra, BS9, Abdulaziz Althafery, MD10, Nashaat Kamal Hamdy Elkalagi, MD11
1King Salman Specialist Hospital, ElRiyad, Ar Riyad, Saudi Arabia; 2The University of Toledo, Ar Riyad, Ar Riyad, Saudi Arabia; 3University of Toledo Medical Center, Toledo, OH; 4Division of Medical Education, Weill Cornell Medicine, Doha, Ad Dawhah, Qatar; 5Michigan, East Lansing, MI; 6Gastroenterology Consultant, Head of Gastroenterology Department, King Salman Specialist Hospital, Hail Health Cluster, Ar Riyad, Ha'il, Saudi Arabia; 7University of Aleppo, Aleppo, Halab, Syria; 8The University of Toledo, Toledo, OH; 9Gastroenterology department, King Salman specialist hospital, Hail health cluster, Hail, Ha'il, Saudi Arabia; 10Consultant radiologist MRI, King Salman specialist Hospital Hail KSA, Hail, Ha'il, Saudi Arabia; 11Lecture of Internal Medicine, Faculty of Medicine, Arish university, Al arish, Al Qahirah, Egypt
Introduction: Low phospholipid-associated cholelithiasis (LPAC) syndrome is a rare, underrecognized genetic disorder involving intrahepatic and extrahepatic cholesterol stone formation due to impaired phosphatidylcholine secretion from ABCB4 gene mutations. It typically affects individuals under 40 and presents with recurrent biliary symptoms, even post-cholecystectomy. Diagnosis is often delayed due to low clinical awareness. We report a case of LPAC in a young adult with chronic relapsing cholangitis post-cholecystectomy to highlight its diagnostic and therapeutic challenges.
Case Description/
Methods: A 32-year-old male with prior laparoscopic cholecystectomy presented with acute epigastric pain and vomiting. He had undergone multiple ERCPs over several years for bile duct stone removal and stenting. Imaging showed persistent intrahepatic and extrahepatic biliary dilation with obstructive stones. During this admission, he developed septic shock from acute cholangitis. Emergency ERCP retrieved a 1 × 2 cm stone, pus, and debris, followed by biliary stenting and clinical improvement (Figure 1). Labs showed elevated WBCs, liver enzymes, and bilirubin. Imaging revealed ongoing biliary obstruction. Despite cholecystectomy, he had recurrent choledocholithiasis, prompting hepatobiliary referral. He was diagnosed with LPAC and started on ursodeoxycholic acid (UDCA). Follow-up imaging showed improved biliary dilation and reduced stone burden. No anatomic anomalies or abscesses were identified.
Discussion: LPAC should be considered in young patients with persistent biliary symptoms after cholecystectomy. In our case, repeated ERCPs were required to manage recurrent cholangitis before diagnosis. Multiple interventions without lasting resolution highlight the challenge of diagnosing LPAC without genetic testing, which confirms only 30–50% of cases. Imaging findings, such as biliary dilation with intraductal stones and a CBD stent as seen on MRCP, can support the diagnosis (Figure 2). UDCA led to stabilization, consistent with the literature showing symptom relief in over 90% of patients. Cholecystectomy alone is insufficient; long-term UDCA is essential. Greater clinical awareness and early treatment are key to preventing complications such as biliary cirrhosis or cholangiocarcinoma. This case highlights the need to consider LPAC in recurrent cholangitis and supports a combined approach of imaging, therapeutic ERCP, and medical therapy for remission.
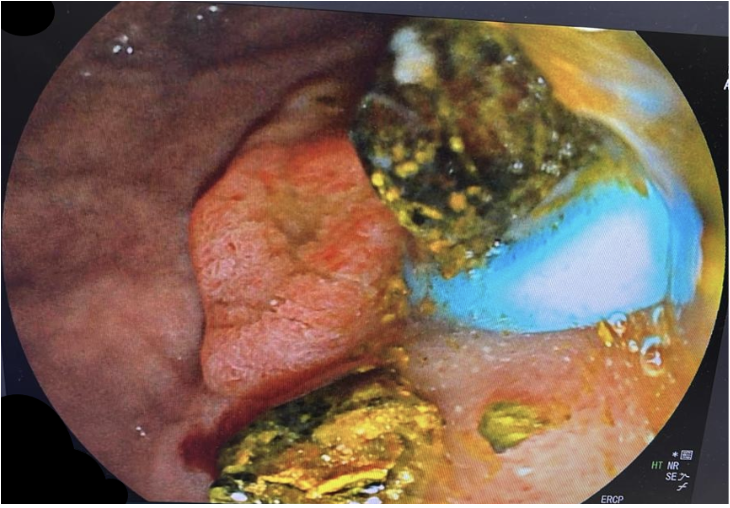
Figure: Figure 1 - Endoscopic retrograde cholangiopancreatography (ERCP) image showing a large common bile duct (CBD) stone and extraction of pus and debris in a patient with acute cholangitis and septic shock. A plastic stent was placed after ductal clearance.

Figure: Figure 2 - Magnetic resonance cholangiopancreatography (MRCP) demonstrating intrahepatic and extrahepatic biliary dilatation with multiple intraductal stones and a CBD stent in place, consistent with ongoing cholangitis in LPAC syndrome.
Disclosures:
Faris Bandar Alrashdan indicated no relevant financial relationships.
Ramy Mahmoud Fathy Elbarody indicated no relevant financial relationships.
Bisher Sawaf indicated no relevant financial relationships.
Amine Rakab indicated no relevant financial relationships.
Lanah Almatroud indicated no relevant financial relationships.
Mahmoud Salah Abdalhakeem Mohammed indicated no relevant financial relationships.
Haidara Bohsas indicated no relevant financial relationships.
Yusuf Omar Hallak indicated no relevant financial relationships.
Atheer Abdullah Ali Aldra indicated no relevant financial relationships.
Abdulaziz Althafery indicated no relevant financial relationships.
Nashaat Kamal Hamdy Elkalagi indicated no relevant financial relationships.
Faris Bandar Alrashdan, MD1, Ramy Mahmoud Fathy Elbarody, BS2, Bisher Sawaf, MD3, Amine Rakab, MD4, Lanah Almatroud, BS5, Mahmoud Salah Abdalhakeem Mohammed, MD6, Haidara Bohsas, MD7, Yusuf Omar Hallak, MD8, Atheer Abdullah Ali Aldra, BS9, Abdulaziz Althafery, MD10, Nashaat Kamal Hamdy Elkalagi, MD11. P4510 - Low Phospholipid-Associated Cholelithiasis Syndrome Presenting as Recurrent Cholangitis Post-Cholecystectomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1King Salman Specialist Hospital, ElRiyad, Ar Riyad, Saudi Arabia; 2The University of Toledo, Ar Riyad, Ar Riyad, Saudi Arabia; 3University of Toledo Medical Center, Toledo, OH; 4Division of Medical Education, Weill Cornell Medicine, Doha, Ad Dawhah, Qatar; 5Michigan, East Lansing, MI; 6Gastroenterology Consultant, Head of Gastroenterology Department, King Salman Specialist Hospital, Hail Health Cluster, Ar Riyad, Ha'il, Saudi Arabia; 7University of Aleppo, Aleppo, Halab, Syria; 8The University of Toledo, Toledo, OH; 9Gastroenterology department, King Salman specialist hospital, Hail health cluster, Hail, Ha'il, Saudi Arabia; 10Consultant radiologist MRI, King Salman specialist Hospital Hail KSA, Hail, Ha'il, Saudi Arabia; 11Lecture of Internal Medicine, Faculty of Medicine, Arish university, Al arish, Al Qahirah, Egypt
Introduction: Low phospholipid-associated cholelithiasis (LPAC) syndrome is a rare, underrecognized genetic disorder involving intrahepatic and extrahepatic cholesterol stone formation due to impaired phosphatidylcholine secretion from ABCB4 gene mutations. It typically affects individuals under 40 and presents with recurrent biliary symptoms, even post-cholecystectomy. Diagnosis is often delayed due to low clinical awareness. We report a case of LPAC in a young adult with chronic relapsing cholangitis post-cholecystectomy to highlight its diagnostic and therapeutic challenges.
Case Description/
Methods: A 32-year-old male with prior laparoscopic cholecystectomy presented with acute epigastric pain and vomiting. He had undergone multiple ERCPs over several years for bile duct stone removal and stenting. Imaging showed persistent intrahepatic and extrahepatic biliary dilation with obstructive stones. During this admission, he developed septic shock from acute cholangitis. Emergency ERCP retrieved a 1 × 2 cm stone, pus, and debris, followed by biliary stenting and clinical improvement (Figure 1). Labs showed elevated WBCs, liver enzymes, and bilirubin. Imaging revealed ongoing biliary obstruction. Despite cholecystectomy, he had recurrent choledocholithiasis, prompting hepatobiliary referral. He was diagnosed with LPAC and started on ursodeoxycholic acid (UDCA). Follow-up imaging showed improved biliary dilation and reduced stone burden. No anatomic anomalies or abscesses were identified.
Discussion: LPAC should be considered in young patients with persistent biliary symptoms after cholecystectomy. In our case, repeated ERCPs were required to manage recurrent cholangitis before diagnosis. Multiple interventions without lasting resolution highlight the challenge of diagnosing LPAC without genetic testing, which confirms only 30–50% of cases. Imaging findings, such as biliary dilation with intraductal stones and a CBD stent as seen on MRCP, can support the diagnosis (Figure 2). UDCA led to stabilization, consistent with the literature showing symptom relief in over 90% of patients. Cholecystectomy alone is insufficient; long-term UDCA is essential. Greater clinical awareness and early treatment are key to preventing complications such as biliary cirrhosis or cholangiocarcinoma. This case highlights the need to consider LPAC in recurrent cholangitis and supports a combined approach of imaging, therapeutic ERCP, and medical therapy for remission.
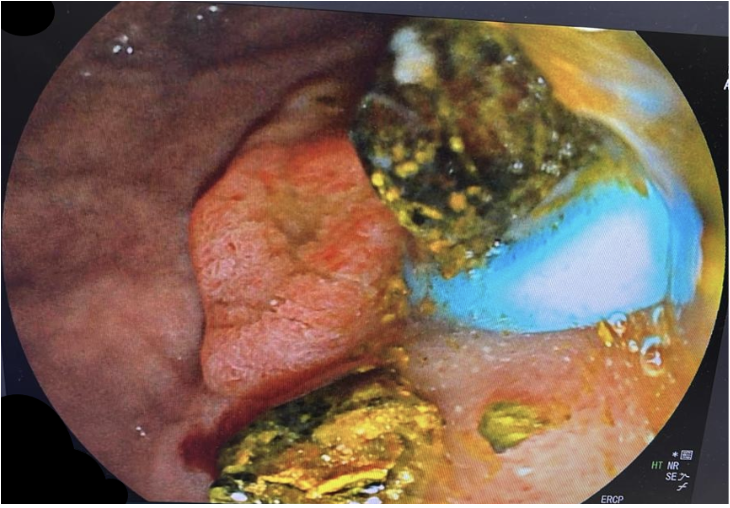
Figure: Figure 1 - Endoscopic retrograde cholangiopancreatography (ERCP) image showing a large common bile duct (CBD) stone and extraction of pus and debris in a patient with acute cholangitis and septic shock. A plastic stent was placed after ductal clearance.

Figure: Figure 2 - Magnetic resonance cholangiopancreatography (MRCP) demonstrating intrahepatic and extrahepatic biliary dilatation with multiple intraductal stones and a CBD stent in place, consistent with ongoing cholangitis in LPAC syndrome.
Disclosures:
Faris Bandar Alrashdan indicated no relevant financial relationships.
Ramy Mahmoud Fathy Elbarody indicated no relevant financial relationships.
Bisher Sawaf indicated no relevant financial relationships.
Amine Rakab indicated no relevant financial relationships.
Lanah Almatroud indicated no relevant financial relationships.
Mahmoud Salah Abdalhakeem Mohammed indicated no relevant financial relationships.
Haidara Bohsas indicated no relevant financial relationships.
Yusuf Omar Hallak indicated no relevant financial relationships.
Atheer Abdullah Ali Aldra indicated no relevant financial relationships.
Abdulaziz Althafery indicated no relevant financial relationships.
Nashaat Kamal Hamdy Elkalagi indicated no relevant financial relationships.
Faris Bandar Alrashdan, MD1, Ramy Mahmoud Fathy Elbarody, BS2, Bisher Sawaf, MD3, Amine Rakab, MD4, Lanah Almatroud, BS5, Mahmoud Salah Abdalhakeem Mohammed, MD6, Haidara Bohsas, MD7, Yusuf Omar Hallak, MD8, Atheer Abdullah Ali Aldra, BS9, Abdulaziz Althafery, MD10, Nashaat Kamal Hamdy Elkalagi, MD11. P4510 - Low Phospholipid-Associated Cholelithiasis Syndrome Presenting as Recurrent Cholangitis Post-Cholecystectomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
