Tuesday Poster Session
Category: Biliary/Pancreas
P4509 - A Tangled Tale: Type 2 Autoimmune Pancreatitis With a Sclerosing Twist
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rachael Hagen, DO (she/her/hers)
University of Connecticut Health
Farmington, CT
Presenting Author(s)
Rachael Hagen, DO1, Bianca Thakkar, DO1, Minh Thu T.. Nguyen, MD2, Norbert Promagan, MD3, Neil Parikh, MD4
1University of Connecticut Health, Farmington, CT; 2University of Connecticut, Farmington, CT; 3Hartford Hospital, Hartford, CT; 4Connecticut GI, Farmington, CT
Introduction: Autoimmune pancreatitis (AIP) is classified into two types: type 1, which is associated with elevated immunoglobulin subclass 4 (IgG4) levels, and the rarer type 2, which typically does not have elevated IgG4 and is often linked with inflammatory bowel disease (IBD). Obstructive jaundice is the most common presentation. Secondary sclerosing cholangitis (SSC) refers to a group of cholestatic liver diseases characterized by bile duct inflammation and fibrosis, leading to stricture formation. We present a case of AIP2 complicated by SSC, highlighting the associated diagnostic challenges.
Case Description/
Methods: A 39-year-old female with Crohn's disease on infliximab and methotrexate presented with one week of abdominal pain, pruritis, and jaundice. Laboratory results showed a normal WBC, mild lipase elevation (66 U/L), with elevated AST (426 U/L), ALT (408 U/L), and ALP (822 U/L). Abdominal ultrasound revealed increased liver echogenicity without ductal dilation.
Endoscopic ultrasound (EUS) revealed a hyperechoic, edematous pancreatic head concerning for AIP, along with common bile duct dilation (Fig 1). Pathology demonstrated reactive glandular cells. Endoscopic retrograde cholangiopancreatography (ERCP) identified biliary strictures, requiring sphincterotomy and stent placement, suspicious for SSC. IgG4 was low (3.3 mg/dl), and anti-mitochondrial antibodies were within normal limits.
One month later, EUS showed hyperechoic strands throughout the pancreas, and biopsy revealed chronic inflammation with occasional plasma cells (Fig 2A-B). She was treated with prednisone, resulting in clinical improvement. However, she was unable to tolerate tapering and required continued immunosuppression with mycophenolate. She developed type 3c diabetes and progressive biliary strictures.
Discussion: The patient’s low IgG4, pancreatic head fullness on imaging, positive response to immunosuppression, IBD association, and recurrent biliary strictures were highly suggestive of AIP2 complicated by SSC, despite inconclusive biopsy findings. Although granulocytic epithelial lesions are diagnostic of AIP2, they may have been missed due to sampling error. Early recognition is critical to prevent stricture formation and complications such as type 3c diabetes, which results from pancreatic exocrine insufficiency. This case underscores the importance of considering AIP2 in patients presenting with obstructive jaundice, particularly when there is a favorable response to steroids.
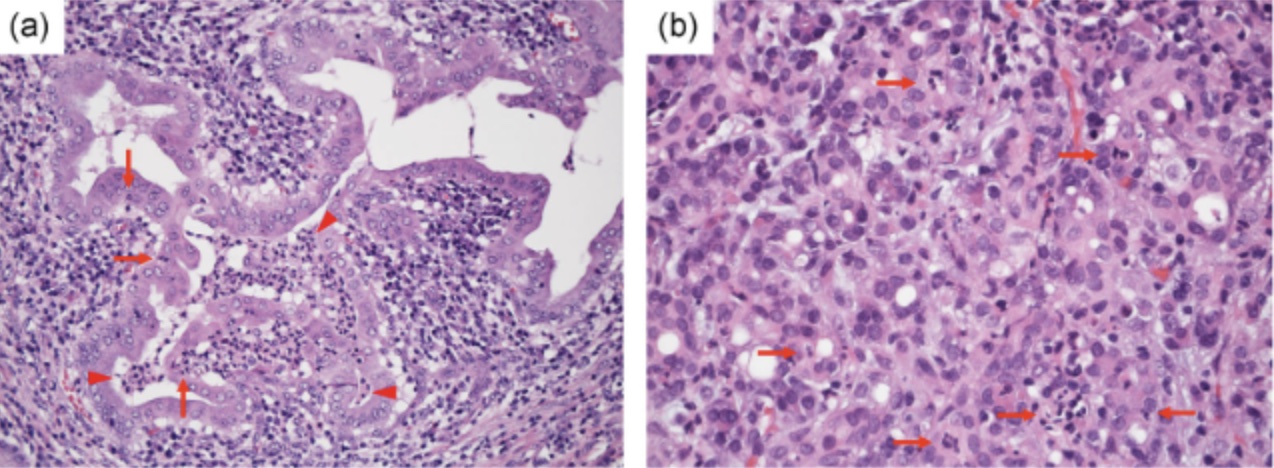
Figure: Figure 1. EUS demonstrating an abnormal, edematous pancreatic head with hyperechoic strands throughout the pancreas, consistent with AIP2.
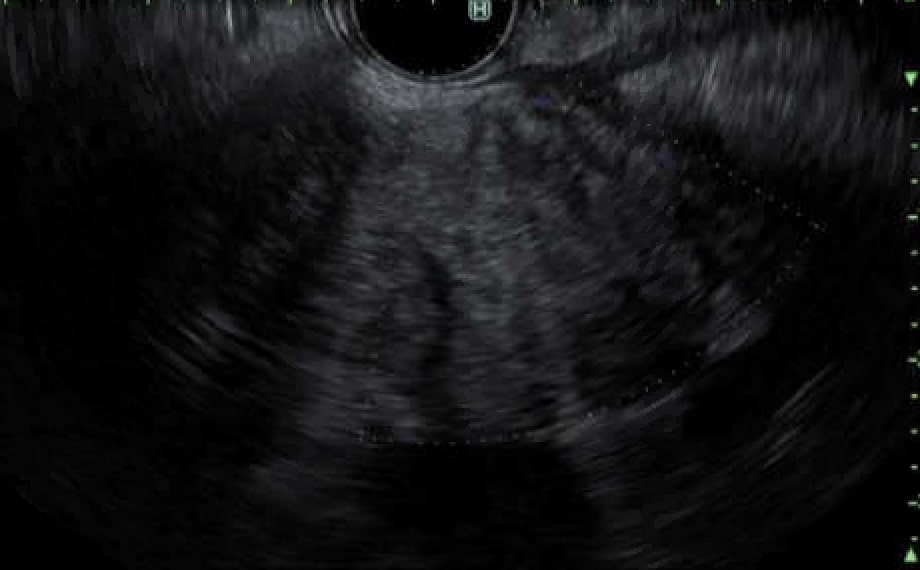
Figure: Figure 2. An example of the characteristic histological features of AIP2 on pathology (pathology slides are currently pending). (A) Granulocytic epithelial lesion with neutrophilic infiltrating in the lumina (arrowheads) and epithelium (arrows) in a resected specimen (Hematoxylin and eosin staining). (B) Acinar-ductal metaplasia with neutrophilic infiltration (arrows) in a lobule seen in a biopsy specimen (Hematoxylin and eosin staining).
Reference: Notohara K, Kamisawa T, Fukushima N, et al. Guidance for diagnosing autoimmune pancreatitis with biopsy tissues. Pathology International 2020; 70(10):699-711. https://doi.org/10.1111/pin.12994
Disclosures:
Rachael Hagen indicated no relevant financial relationships.
Bianca Thakkar indicated no relevant financial relationships.
Minh Thu Nguyen indicated no relevant financial relationships.
Norbert Promagan indicated no relevant financial relationships.
Neil Parikh indicated no relevant financial relationships.
Rachael Hagen, DO1, Bianca Thakkar, DO1, Minh Thu T.. Nguyen, MD2, Norbert Promagan, MD3, Neil Parikh, MD4. P4509 - A Tangled Tale: Type 2 Autoimmune Pancreatitis With a Sclerosing Twist, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Connecticut Health, Farmington, CT; 2University of Connecticut, Farmington, CT; 3Hartford Hospital, Hartford, CT; 4Connecticut GI, Farmington, CT
Introduction: Autoimmune pancreatitis (AIP) is classified into two types: type 1, which is associated with elevated immunoglobulin subclass 4 (IgG4) levels, and the rarer type 2, which typically does not have elevated IgG4 and is often linked with inflammatory bowel disease (IBD). Obstructive jaundice is the most common presentation. Secondary sclerosing cholangitis (SSC) refers to a group of cholestatic liver diseases characterized by bile duct inflammation and fibrosis, leading to stricture formation. We present a case of AIP2 complicated by SSC, highlighting the associated diagnostic challenges.
Case Description/
Methods: A 39-year-old female with Crohn's disease on infliximab and methotrexate presented with one week of abdominal pain, pruritis, and jaundice. Laboratory results showed a normal WBC, mild lipase elevation (66 U/L), with elevated AST (426 U/L), ALT (408 U/L), and ALP (822 U/L). Abdominal ultrasound revealed increased liver echogenicity without ductal dilation.
Endoscopic ultrasound (EUS) revealed a hyperechoic, edematous pancreatic head concerning for AIP, along with common bile duct dilation (Fig 1). Pathology demonstrated reactive glandular cells. Endoscopic retrograde cholangiopancreatography (ERCP) identified biliary strictures, requiring sphincterotomy and stent placement, suspicious for SSC. IgG4 was low (3.3 mg/dl), and anti-mitochondrial antibodies were within normal limits.
One month later, EUS showed hyperechoic strands throughout the pancreas, and biopsy revealed chronic inflammation with occasional plasma cells (Fig 2A-B). She was treated with prednisone, resulting in clinical improvement. However, she was unable to tolerate tapering and required continued immunosuppression with mycophenolate. She developed type 3c diabetes and progressive biliary strictures.
Discussion: The patient’s low IgG4, pancreatic head fullness on imaging, positive response to immunosuppression, IBD association, and recurrent biliary strictures were highly suggestive of AIP2 complicated by SSC, despite inconclusive biopsy findings. Although granulocytic epithelial lesions are diagnostic of AIP2, they may have been missed due to sampling error. Early recognition is critical to prevent stricture formation and complications such as type 3c diabetes, which results from pancreatic exocrine insufficiency. This case underscores the importance of considering AIP2 in patients presenting with obstructive jaundice, particularly when there is a favorable response to steroids.
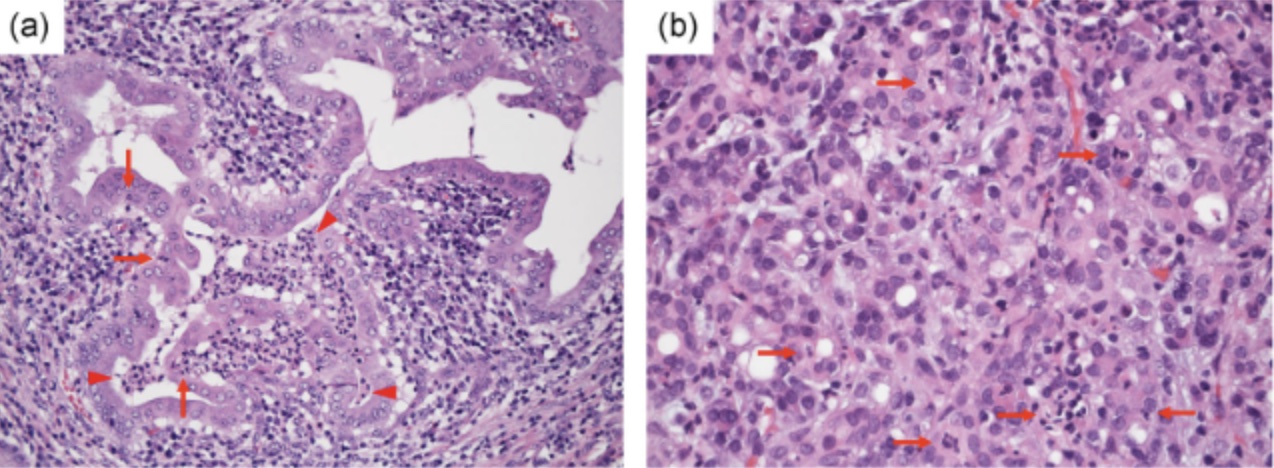
Figure: Figure 1. EUS demonstrating an abnormal, edematous pancreatic head with hyperechoic strands throughout the pancreas, consistent with AIP2.
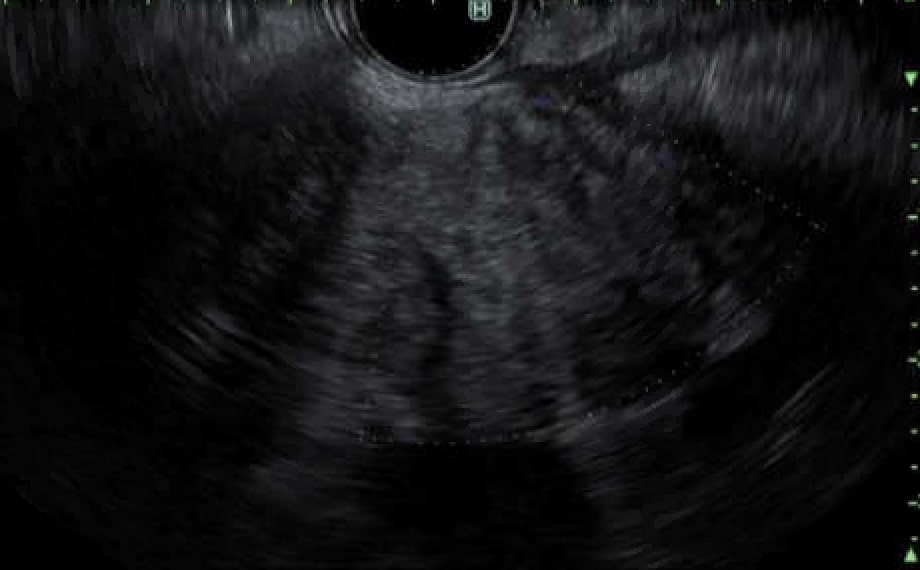
Figure: Figure 2. An example of the characteristic histological features of AIP2 on pathology (pathology slides are currently pending). (A) Granulocytic epithelial lesion with neutrophilic infiltrating in the lumina (arrowheads) and epithelium (arrows) in a resected specimen (Hematoxylin and eosin staining). (B) Acinar-ductal metaplasia with neutrophilic infiltration (arrows) in a lobule seen in a biopsy specimen (Hematoxylin and eosin staining).
Reference: Notohara K, Kamisawa T, Fukushima N, et al. Guidance for diagnosing autoimmune pancreatitis with biopsy tissues. Pathology International 2020; 70(10):699-711. https://doi.org/10.1111/pin.12994
Disclosures:
Rachael Hagen indicated no relevant financial relationships.
Bianca Thakkar indicated no relevant financial relationships.
Minh Thu Nguyen indicated no relevant financial relationships.
Norbert Promagan indicated no relevant financial relationships.
Neil Parikh indicated no relevant financial relationships.
Rachael Hagen, DO1, Bianca Thakkar, DO1, Minh Thu T.. Nguyen, MD2, Norbert Promagan, MD3, Neil Parikh, MD4. P4509 - A Tangled Tale: Type 2 Autoimmune Pancreatitis With a Sclerosing Twist, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
