Tuesday Poster Session
Category: Biliary/Pancreas
P4505 - A Rare Metabolic Storm: Euglycemic Diabetic Ketoacidosis and Hypertriglyceridemia-Induced Pancreatitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Panida Charnvitayapong, MD (she/her/hers)
University of Miami Miller School of Medicine at JFK Medical Center
Atlantis, FL
Presenting Author(s)
Panida Charnvitayapong, MD1, Bebika Subedi, MD1, Michelle Cheung, DO1, Aviv Katz, DO2
1University of Miami Miller School of Medicine at JFK Medical Center, Atlantis, FL; 2HCA Florida Healthcare, Atlantis, FL
Introduction: The simultaneous presentation of euglycemic diabetic ketoacidosis (DKA), hypertriglyceridemia (HTG), and acute pancreatitis is extremely rare and can lead to severe morbidity and mortality. This triad poses both diagnostic and therapeutic challenges.
Case Description/
Methods: A 46-year-old woman with a past medical history of type 2 diabetes and hyperlipidemia came to the emergency department with right upper quadrant and epigastric pain radiating to her flank that started on the day of admission. She described the pain as persistent with no relieving factors, worse on palpation, and associated nausea but no vomiting. Otherwise denied any chest pain or shortness of breath.
CT abdomen and pelvis showed proximal peripancreatic edema and gastric distension. RUQ ultrasound revealed an edematous pancreatic head and hepatic steatosis but no gallstones or cholecystitis. Vital signs were stable, and labs were remarkable for a mildly elevated lipase (359), AST/ALT of 42/20, and a high anion gap metabolic acidosis (anion gap 18). Blood glucose was only slightly increased, but serum acetones were positive. Her triglycerides were markedly elevated at 1575 mg/dL. She noted she had recently stopped taking an SGLT2 inhibitor about a week prior.
The clinical picture revealed a combination of acute pancreatitis, euglycemic DKA, and severe HTG. She was admitted to the ICU and managed with IV insulin, fluids, and electrolyte correction. Her condition gradually improved with supportive care, including pain control and early reintroduction of oral intake. At discharge, her SGLT2 inhibitor was discontinued, and she was advised to continue statin and fibrate therapy with close outpatient follow-up.
Discussion: Determining the sequence of events in this triad is complex. It remains unclear whether DKA led to HTG and then pancreatitis or if pancreatitis triggered the metabolic cascade. In DKA, insulin deficiency and lipolysis can result in significant HTG, which may precipitate pancreatitis. Conversely, acute pancreatitis can destabilize glycemic control and precipitate DKA. Additionally, research has shown that euglycemic DKA is an uncommon side effect of SGLT2 inhibitors, complicating our case.
Regardless of the initiating factor, management is centered on ICU-level care, insulin therapy, fluid resuscitation, early feeding, and medication reconciliation. This case highlights the importance of recognizing this difficult clinical scenario and early treatment for better outcomes.
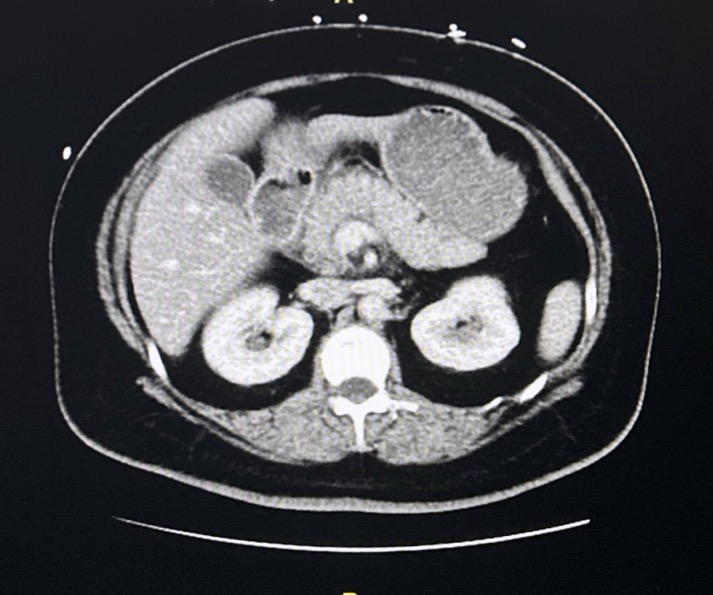
Figure: CT abdomen/pelvis: Acute pancreatitis with proximal peripancreatic edema. Gastric distension and suspected reactive distal gastric and pyloric congestion.
Disclosures:
Panida Charnvitayapong indicated no relevant financial relationships.
Bebika Subedi indicated no relevant financial relationships.
Michelle Cheung indicated no relevant financial relationships.
Aviv Katz indicated no relevant financial relationships.
Panida Charnvitayapong, MD1, Bebika Subedi, MD1, Michelle Cheung, DO1, Aviv Katz, DO2. P4505 - A Rare Metabolic Storm: Euglycemic Diabetic Ketoacidosis and Hypertriglyceridemia-Induced Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Miami Miller School of Medicine at JFK Medical Center, Atlantis, FL; 2HCA Florida Healthcare, Atlantis, FL
Introduction: The simultaneous presentation of euglycemic diabetic ketoacidosis (DKA), hypertriglyceridemia (HTG), and acute pancreatitis is extremely rare and can lead to severe morbidity and mortality. This triad poses both diagnostic and therapeutic challenges.
Case Description/
Methods: A 46-year-old woman with a past medical history of type 2 diabetes and hyperlipidemia came to the emergency department with right upper quadrant and epigastric pain radiating to her flank that started on the day of admission. She described the pain as persistent with no relieving factors, worse on palpation, and associated nausea but no vomiting. Otherwise denied any chest pain or shortness of breath.
CT abdomen and pelvis showed proximal peripancreatic edema and gastric distension. RUQ ultrasound revealed an edematous pancreatic head and hepatic steatosis but no gallstones or cholecystitis. Vital signs were stable, and labs were remarkable for a mildly elevated lipase (359), AST/ALT of 42/20, and a high anion gap metabolic acidosis (anion gap 18). Blood glucose was only slightly increased, but serum acetones were positive. Her triglycerides were markedly elevated at 1575 mg/dL. She noted she had recently stopped taking an SGLT2 inhibitor about a week prior.
The clinical picture revealed a combination of acute pancreatitis, euglycemic DKA, and severe HTG. She was admitted to the ICU and managed with IV insulin, fluids, and electrolyte correction. Her condition gradually improved with supportive care, including pain control and early reintroduction of oral intake. At discharge, her SGLT2 inhibitor was discontinued, and she was advised to continue statin and fibrate therapy with close outpatient follow-up.
Discussion: Determining the sequence of events in this triad is complex. It remains unclear whether DKA led to HTG and then pancreatitis or if pancreatitis triggered the metabolic cascade. In DKA, insulin deficiency and lipolysis can result in significant HTG, which may precipitate pancreatitis. Conversely, acute pancreatitis can destabilize glycemic control and precipitate DKA. Additionally, research has shown that euglycemic DKA is an uncommon side effect of SGLT2 inhibitors, complicating our case.
Regardless of the initiating factor, management is centered on ICU-level care, insulin therapy, fluid resuscitation, early feeding, and medication reconciliation. This case highlights the importance of recognizing this difficult clinical scenario and early treatment for better outcomes.
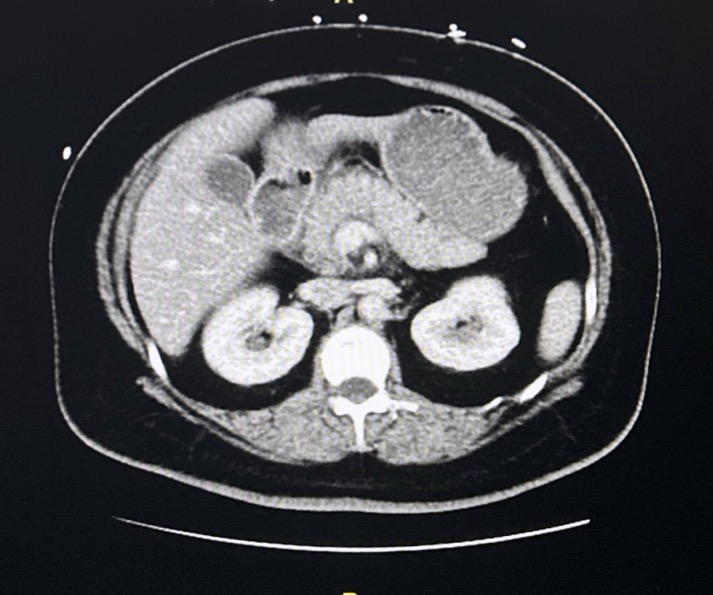
Figure: CT abdomen/pelvis: Acute pancreatitis with proximal peripancreatic edema. Gastric distension and suspected reactive distal gastric and pyloric congestion.
Disclosures:
Panida Charnvitayapong indicated no relevant financial relationships.
Bebika Subedi indicated no relevant financial relationships.
Michelle Cheung indicated no relevant financial relationships.
Aviv Katz indicated no relevant financial relationships.
Panida Charnvitayapong, MD1, Bebika Subedi, MD1, Michelle Cheung, DO1, Aviv Katz, DO2. P4505 - A Rare Metabolic Storm: Euglycemic Diabetic Ketoacidosis and Hypertriglyceridemia-Induced Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
