Tuesday Poster Session
Category: Biliary/Pancreas
P4500 - Acute Pancreatitis Following Transjugular Liver Biopsy: A Rare Complication
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ahmed Shehadah, MD (he/him/his)
United Health Services, Wilson Medical Center
Binghamton, NY
Presenting Author(s)
Ahmed Shehadah, MD1, Alshaima Yousef, MD2, Usama Sakhawat, MD3, Khandokar Talib, MD4, Gowthami Ramar, MD1, AbdulSubhan Talpur, MD1, Fawad Talat, MD1, Timothy Chan, BS5, Amanke Oranu, MD1, Toseef Javaid, MD3
1United Health Services, Wilson Medical Center, Binghamton, NY; 2Rochester General Hospital, Rochester, NY; 3United Health Services, Wilson Medical Center, Johnson City, NY; 4United Health Services, Johnson City, NY; 5SUNY Upstate Medical University, Syracuse, NY
Introduction: Liver biopsy is the gold standard for diagnosing many hepatic and biliary disorders. While transjugular liver biopsy (TJLB) is preferred for having a better safety profile especially in patients with coagulopathy or ascites, it still carries risks similar to percutaneous biopsy. Hemobilia is a rare but recognized complication that can lead to biliary obstruction and, in extremely rare cases, acute pancreatitis. We present a unique case of acute pancreatitis secondary to biliary obstruction from hemobilia following TJLB.
Case Description/
Methods: A 49-year-old male with a history of chronically elevated liver enzymes, atrial fibrillation on apixaban presented with severe epigastric abdominal pain radiating to the back, associated with nonbloody nausea and vomiting. He denied melena, hematochezia, or fever.
Two days prior to admission, he underwent a TJLB. The procedure was uncomplicated, and the patient tolerated it well the same day. Hemodynamic measurements were normal with a hepatic venous pressure gradient of 3 mmHg.
On presentation, vital signs were stable. Laboratory tests revealed leukocytosis, hemoglobin 13.5 g/dL, total bilirubin 2.4 mg/dL, markedly elevated lipase >4000 U/L, and normal triglyceride levels. Liver enzymes were moderately elevated. By the next day, hemoglobin had dropped to 10.6 g/dL and total bilirubin rose to 3.6 mg/dL.
A CT scan of the abdomen and pelvis was unremarkable for any intraabdominal pathology. Right upper quadrant ultrasound showed gallbladder wall thickening, a small amount of pericholecystic fluid, and a nondilated common bile duct (1.4 mm). HIDA scan did not demonstrate bile leak or biliary obstruction. MRCP revealed a new, elongated, nonenhancing filling defect with round margins in the distal common bile duct, measuring 2.6 cm × 0.6 cm, with a CBD diameter of 1.1 cm and mild intrahepatic ductal dilation.
The patient was started on broad-spectrum antibiotics. Apixaban was held, and thromboprophylaxis was avoided. Gastroenterology team performed ERCP to relieve the biliary ductal obstruction from hemobilia.
Discussion: Despite stable vital signs and an unremarkable CT scan, the patient had classic symptoms of acute pancreatitis, a significant drop in hemoglobin, and MRCP findings consistent with biliary obstruction due to hemobilia, along with a suspected self-limited bile leak. While TJLB has a better safety profile than percutaneous liver biopsy, complications can still occur, needing a high index of suspicion to arrive at the correct diagnosis.
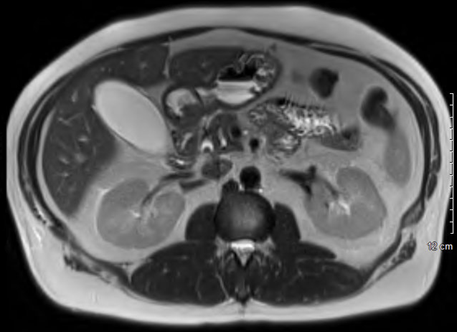
Figure: Magnetic Resonance Cholangiopancreatography: An elongated, nonenhancing filling defect identified within the distal common bile duct measuring up to 1.1cm in diameter. Gallbladder is distended with trace pericholecystic fluid. Not seen in this image - mild intrahepatic biliary ductal dilation.
Disclosures:
Ahmed Shehadah indicated no relevant financial relationships.
Alshaima Yousef indicated no relevant financial relationships.
Usama Sakhawat indicated no relevant financial relationships.
Khandokar Talib indicated no relevant financial relationships.
Gowthami Ramar indicated no relevant financial relationships.
AbdulSubhan Talpur indicated no relevant financial relationships.
Fawad Talat indicated no relevant financial relationships.
Timothy Chan indicated no relevant financial relationships.
Amanke Oranu indicated no relevant financial relationships.
Toseef Javaid indicated no relevant financial relationships.
Ahmed Shehadah, MD1, Alshaima Yousef, MD2, Usama Sakhawat, MD3, Khandokar Talib, MD4, Gowthami Ramar, MD1, AbdulSubhan Talpur, MD1, Fawad Talat, MD1, Timothy Chan, BS5, Amanke Oranu, MD1, Toseef Javaid, MD3. P4500 - Acute Pancreatitis Following Transjugular Liver Biopsy: A Rare Complication, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1United Health Services, Wilson Medical Center, Binghamton, NY; 2Rochester General Hospital, Rochester, NY; 3United Health Services, Wilson Medical Center, Johnson City, NY; 4United Health Services, Johnson City, NY; 5SUNY Upstate Medical University, Syracuse, NY
Introduction: Liver biopsy is the gold standard for diagnosing many hepatic and biliary disorders. While transjugular liver biopsy (TJLB) is preferred for having a better safety profile especially in patients with coagulopathy or ascites, it still carries risks similar to percutaneous biopsy. Hemobilia is a rare but recognized complication that can lead to biliary obstruction and, in extremely rare cases, acute pancreatitis. We present a unique case of acute pancreatitis secondary to biliary obstruction from hemobilia following TJLB.
Case Description/
Methods: A 49-year-old male with a history of chronically elevated liver enzymes, atrial fibrillation on apixaban presented with severe epigastric abdominal pain radiating to the back, associated with nonbloody nausea and vomiting. He denied melena, hematochezia, or fever.
Two days prior to admission, he underwent a TJLB. The procedure was uncomplicated, and the patient tolerated it well the same day. Hemodynamic measurements were normal with a hepatic venous pressure gradient of 3 mmHg.
On presentation, vital signs were stable. Laboratory tests revealed leukocytosis, hemoglobin 13.5 g/dL, total bilirubin 2.4 mg/dL, markedly elevated lipase >4000 U/L, and normal triglyceride levels. Liver enzymes were moderately elevated. By the next day, hemoglobin had dropped to 10.6 g/dL and total bilirubin rose to 3.6 mg/dL.
A CT scan of the abdomen and pelvis was unremarkable for any intraabdominal pathology. Right upper quadrant ultrasound showed gallbladder wall thickening, a small amount of pericholecystic fluid, and a nondilated common bile duct (1.4 mm). HIDA scan did not demonstrate bile leak or biliary obstruction. MRCP revealed a new, elongated, nonenhancing filling defect with round margins in the distal common bile duct, measuring 2.6 cm × 0.6 cm, with a CBD diameter of 1.1 cm and mild intrahepatic ductal dilation.
The patient was started on broad-spectrum antibiotics. Apixaban was held, and thromboprophylaxis was avoided. Gastroenterology team performed ERCP to relieve the biliary ductal obstruction from hemobilia.
Discussion: Despite stable vital signs and an unremarkable CT scan, the patient had classic symptoms of acute pancreatitis, a significant drop in hemoglobin, and MRCP findings consistent with biliary obstruction due to hemobilia, along with a suspected self-limited bile leak. While TJLB has a better safety profile than percutaneous liver biopsy, complications can still occur, needing a high index of suspicion to arrive at the correct diagnosis.
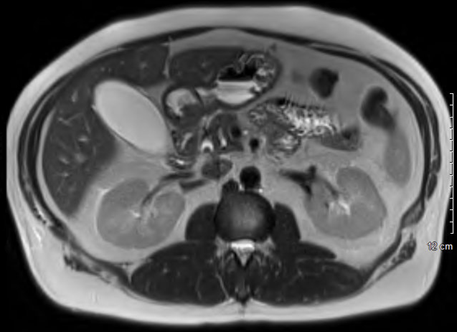
Figure: Magnetic Resonance Cholangiopancreatography: An elongated, nonenhancing filling defect identified within the distal common bile duct measuring up to 1.1cm in diameter. Gallbladder is distended with trace pericholecystic fluid. Not seen in this image - mild intrahepatic biliary ductal dilation.
Disclosures:
Ahmed Shehadah indicated no relevant financial relationships.
Alshaima Yousef indicated no relevant financial relationships.
Usama Sakhawat indicated no relevant financial relationships.
Khandokar Talib indicated no relevant financial relationships.
Gowthami Ramar indicated no relevant financial relationships.
AbdulSubhan Talpur indicated no relevant financial relationships.
Fawad Talat indicated no relevant financial relationships.
Timothy Chan indicated no relevant financial relationships.
Amanke Oranu indicated no relevant financial relationships.
Toseef Javaid indicated no relevant financial relationships.
Ahmed Shehadah, MD1, Alshaima Yousef, MD2, Usama Sakhawat, MD3, Khandokar Talib, MD4, Gowthami Ramar, MD1, AbdulSubhan Talpur, MD1, Fawad Talat, MD1, Timothy Chan, BS5, Amanke Oranu, MD1, Toseef Javaid, MD3. P4500 - Acute Pancreatitis Following Transjugular Liver Biopsy: A Rare Complication, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
