Tuesday Poster Session
Category: Biliary/Pancreas
P4498 - The Black Ampulla: A Melanoma in Disguise
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- BJ
Bradley D. Johnson, DO
Geisinger Health System
Danville, PA
Presenting Author(s)
Bradley D. Johnson, DO1, Pranav Patel, MD1, Dema Shamoon, MD1, Aws Alameri, MD1, Rasiq Zackria, MD1, Harshit S. Khara, MD2, Bradley D. Confer, DO1, David L.. Diehl, MD1, Danial H. Shaikh, MD1
1Geisinger Health System, Danville, PA; 2Geisinger Health System, Danville, NJ
Introduction: Malignant melanoma, which only constitutes 1% of all skin cancers, is responsible for the majority of skin cancer-related deaths. Its aggressive nature and potential for early metastasis make it a clinical challenge. Autopsy studies have indicated that up to 15% of patients with metastatic melanoma exhibit gallbladder involvement, yet clinical presentations involving the common bile duct (CBD) or ampulla of Vater are rare.
We detail a unique presentation of metastatic melanoma with initially undetected primary, manifesting as biliary obstruction.
Case Description/
Methods: A 60-year-old female presented with a three-week history of nausea, vomiting, and diarrhea. She later developed jaundice, pale stools and intermittent right upper quadrant abdominal pain. Labs revealed: AST 205 U/L, ALT 285 U/L, alkaline phosphatase 263 U/L, total bilirubin 5.8 mg/dL, and lipase 735 U/L.
CT of the abdomen and pelvis demonstrated dilated intra- and extrahepatic bile ducts, with CBD measuring 1.4 cm in diameter.
MRCP revealed a T1 hyperintense mass at the pancreaticoduodenal groove near the major papilla, measuring 2 x 1.5 cm, along with small T1 hyperintense lesions in the pancreas, peritoneum, and mesenteric lymph nodes.
EUS identified a hypoechoic mass at the ampulla. Fine-needle biospy (FNB) of the lesion yielded black-colored fluid, which was confirmed to be melanoma after analysis. EGD also revealed a non-bleeding cratered gastric body ulcer; biopsy of which also confirmed metastatic melanoma.
ERCP showed a pigmented, irregular ampulla consistent with melanomatous involvement. A sphincterotomy was performed, and a covered metal stent was placed to relieve the obstruction.
A dermatological examination uncovered a red lesion on the patient's right lower abdomen, which upon biopsy, confirmed invasive malignant melanoma.
Discussion: This case illustrates a rare instance where metastatic melanoma presented primarily as biliary obstruction. Absence of a known cutaneous primary lesion at the time of diagnosis is known as melanoma of unknown primary (MUP), which occurs in approximately 3.2% of all melanoma cases.
The presence of T1 hyperintense lesions on MRCP can be indicative of melanoma due to melanin's para-magnetic properties. EUS-FNA played a pivotal role in obtaining diagnostic tissue, with the unusual finding of a black-colored aspirate further supporting the diagnosis. Management involved endoscopic intervention to alleviate biliary obstruction and systemic evaluation to identify the primary lesion.
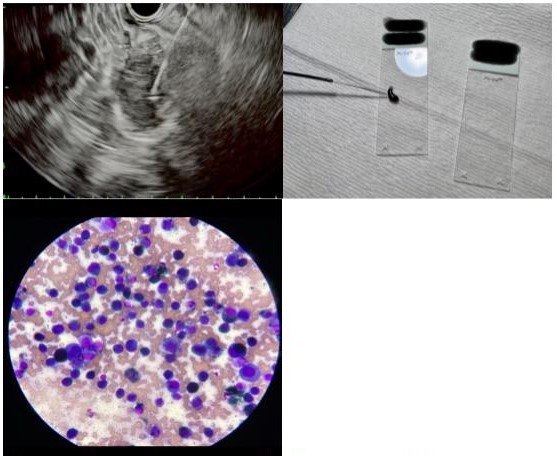
Figure: EUS-guided biopsy with expression of black fluid and histopathology

Figure: Black ampulla on ERCP, with stent placement (top row). Metastatic gastric nodule (bottom left). Abdominal wall nodule (bottom right).
Disclosures:
Bradley Johnson indicated no relevant financial relationships.
Pranav Patel indicated no relevant financial relationships.
Dema Shamoon indicated no relevant financial relationships.
Aws Alameri indicated no relevant financial relationships.
Rasiq Zackria indicated no relevant financial relationships.
Harshit Khara indicated no relevant financial relationships.
Bradley Confer indicated no relevant financial relationships.
David Diehl indicated no relevant financial relationships.
Danial Shaikh indicated no relevant financial relationships.
Bradley D. Johnson, DO1, Pranav Patel, MD1, Dema Shamoon, MD1, Aws Alameri, MD1, Rasiq Zackria, MD1, Harshit S. Khara, MD2, Bradley D. Confer, DO1, David L.. Diehl, MD1, Danial H. Shaikh, MD1. P4498 - The Black Ampulla: A Melanoma in Disguise, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Geisinger Health System, Danville, PA; 2Geisinger Health System, Danville, NJ
Introduction: Malignant melanoma, which only constitutes 1% of all skin cancers, is responsible for the majority of skin cancer-related deaths. Its aggressive nature and potential for early metastasis make it a clinical challenge. Autopsy studies have indicated that up to 15% of patients with metastatic melanoma exhibit gallbladder involvement, yet clinical presentations involving the common bile duct (CBD) or ampulla of Vater are rare.
We detail a unique presentation of metastatic melanoma with initially undetected primary, manifesting as biliary obstruction.
Case Description/
Methods: A 60-year-old female presented with a three-week history of nausea, vomiting, and diarrhea. She later developed jaundice, pale stools and intermittent right upper quadrant abdominal pain. Labs revealed: AST 205 U/L, ALT 285 U/L, alkaline phosphatase 263 U/L, total bilirubin 5.8 mg/dL, and lipase 735 U/L.
CT of the abdomen and pelvis demonstrated dilated intra- and extrahepatic bile ducts, with CBD measuring 1.4 cm in diameter.
MRCP revealed a T1 hyperintense mass at the pancreaticoduodenal groove near the major papilla, measuring 2 x 1.5 cm, along with small T1 hyperintense lesions in the pancreas, peritoneum, and mesenteric lymph nodes.
EUS identified a hypoechoic mass at the ampulla. Fine-needle biospy (FNB) of the lesion yielded black-colored fluid, which was confirmed to be melanoma after analysis. EGD also revealed a non-bleeding cratered gastric body ulcer; biopsy of which also confirmed metastatic melanoma.
ERCP showed a pigmented, irregular ampulla consistent with melanomatous involvement. A sphincterotomy was performed, and a covered metal stent was placed to relieve the obstruction.
A dermatological examination uncovered a red lesion on the patient's right lower abdomen, which upon biopsy, confirmed invasive malignant melanoma.
Discussion: This case illustrates a rare instance where metastatic melanoma presented primarily as biliary obstruction. Absence of a known cutaneous primary lesion at the time of diagnosis is known as melanoma of unknown primary (MUP), which occurs in approximately 3.2% of all melanoma cases.
The presence of T1 hyperintense lesions on MRCP can be indicative of melanoma due to melanin's para-magnetic properties. EUS-FNA played a pivotal role in obtaining diagnostic tissue, with the unusual finding of a black-colored aspirate further supporting the diagnosis. Management involved endoscopic intervention to alleviate biliary obstruction and systemic evaluation to identify the primary lesion.
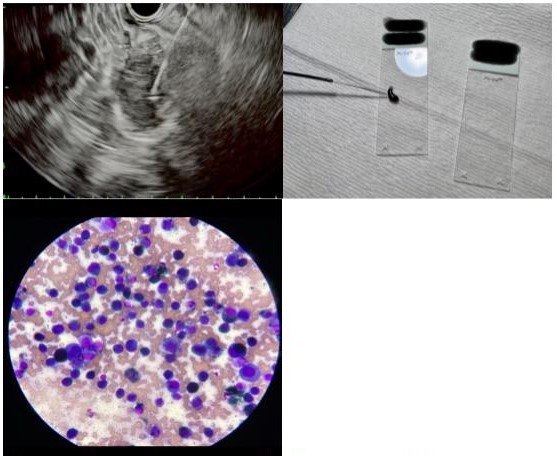
Figure: EUS-guided biopsy with expression of black fluid and histopathology

Figure: Black ampulla on ERCP, with stent placement (top row). Metastatic gastric nodule (bottom left). Abdominal wall nodule (bottom right).
Disclosures:
Bradley Johnson indicated no relevant financial relationships.
Pranav Patel indicated no relevant financial relationships.
Dema Shamoon indicated no relevant financial relationships.
Aws Alameri indicated no relevant financial relationships.
Rasiq Zackria indicated no relevant financial relationships.
Harshit Khara indicated no relevant financial relationships.
Bradley Confer indicated no relevant financial relationships.
David Diehl indicated no relevant financial relationships.
Danial Shaikh indicated no relevant financial relationships.
Bradley D. Johnson, DO1, Pranav Patel, MD1, Dema Shamoon, MD1, Aws Alameri, MD1, Rasiq Zackria, MD1, Harshit S. Khara, MD2, Bradley D. Confer, DO1, David L.. Diehl, MD1, Danial H. Shaikh, MD1. P4498 - The Black Ampulla: A Melanoma in Disguise, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

