Tuesday Poster Session
Category: Biliary/Pancreas
P4463 - Biliary Complications Due to Stent-Assisted Coil Embolization of a Portal Vein Aneurysm
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Olivia Battistoni, MPH, BA
The Ohio State University College of Medicine
Columbus, OH
Presenting Author(s)
Olivia Battistoni, MPH, BA1, Madeleine Davis, BA1, Suraj Pai, MD2, Shaoli Sun, MD2, Marissa Guo, MD2, Fred Karaisz, MD2, Vivek Mendiratta, MD3
1The Ohio State University College of Medicine, Columbus, OH; 2The Ohio State University Wexner Medical Center, Columbus, OH; 3The Ohio State University Wexner Medical Center, Dublin, OH
Introduction: Portal vein aneurysm (PVA) is a rare entity with no clear consensus on the management of enlarging aneurysms. We describe a patient with an idiopathic PVA who underwent stent-assisted coil embolization complicated by biliary obstruction.
Case Description/
Methods: A 53-year-old woman with coronary artery disease and myelodysplastic syndrome presented for asymptomatic enlarging PVA. Her PVA was previously monitored for 15 years with surveillance imaging, but recent CT angiography showed significant enlargement from an original diameter of 2.3cm to 5.2cm by 6.4cm along with new cirrhosis (Figure 1). Given the rapid enlargement, interventional radiology performed a transhepatic coil embolization of the PVA. Two weeks later, the patient presented with new painless jaundice and pruritus. Lab studies showed total bilirubin of 32.9 mg/dL (direct bilirubin >20 mg/dL), ALP 2,675 U/L, ALT 152 U/L, and AST 128 U/L from previously normal baseline values. Imaging (ultrasound, CT, and MRI) revealed no evidence of biliary obstruction, and serologic workup and medication review for other etiologies of liver injury were negative. However, the suspicion for an obstructive process remained high so endoscopic ultrasound (EUS) guided liver biopsy and endoscopic retrograde cholangiopancreatography (ERCP) were performed. The liver biopsy revealed mild steatosis without evidence of cirrhosis. ERCP revealed narrowing of the common bile duct from presumed extrinsic compression due to the recently placed portal vein coils and subsequent bile leak (Figure 2). A biliary sphincterotomy was performed and a plastic stent was placed with rapid improvement in the patient’s cholestasis -- lab studies obtained one week later noted total bilirubin 3.6 mg/dL, ALP 2138 U/L, ALT 47 U/L, and AST 32 U/L.
Discussion: PVA is a focal portal venous dilation exceeding either 1.5cm in normal livers or 1.9cm in cirrhotic livers. They are rare, with fewer than 200 cases reported in the literature, and thus their management is non-standardized. Current guidelines recommend surgical intervention for PVAs with thrombosis or symptoms, while data on endovascular repair are limited. Our patient underwent stent-assisted coil embolization and later developed cholestatic liver injury. This case illustrates how endovascular PVA repair can cause extrinsic biliary obstruction even without biliary dilation on imaging, highlighting the need for a broad differential for post-procedural liver injury and awareness of this rare complication.
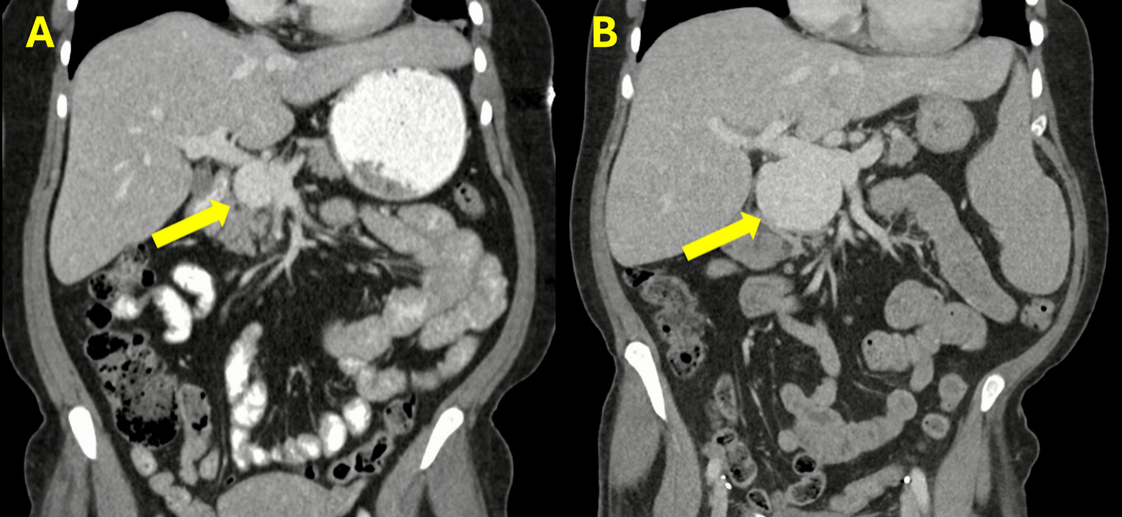
Figure: Figure 1: PVA (yellow arrow) detected incidentally 15 years prior to presentation. (B) PVA at presentation measuring 6.2 cm.
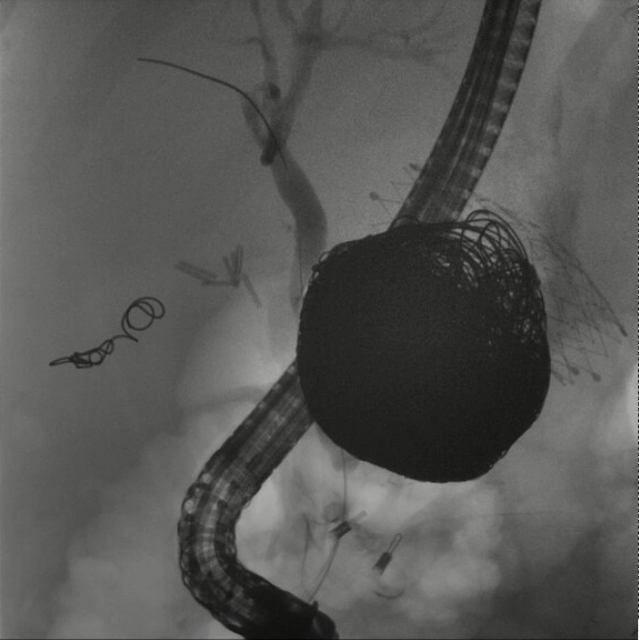
Figure: Figure 2: ERCP demonstrating mid common bile duct stricture in proximity to the coil embolization of the PVA.
Disclosures:
Olivia Battistoni indicated no relevant financial relationships.
Madeleine Davis indicated no relevant financial relationships.
Suraj Pai indicated no relevant financial relationships.
Shaoli Sun indicated no relevant financial relationships.
Marissa Guo indicated no relevant financial relationships.
Fred Karaisz indicated no relevant financial relationships.
Vivek Mendiratta indicated no relevant financial relationships.
Olivia Battistoni, MPH, BA1, Madeleine Davis, BA1, Suraj Pai, MD2, Shaoli Sun, MD2, Marissa Guo, MD2, Fred Karaisz, MD2, Vivek Mendiratta, MD3. P4463 - Biliary Complications Due to Stent-Assisted Coil Embolization of a Portal Vein Aneurysm, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1The Ohio State University College of Medicine, Columbus, OH; 2The Ohio State University Wexner Medical Center, Columbus, OH; 3The Ohio State University Wexner Medical Center, Dublin, OH
Introduction: Portal vein aneurysm (PVA) is a rare entity with no clear consensus on the management of enlarging aneurysms. We describe a patient with an idiopathic PVA who underwent stent-assisted coil embolization complicated by biliary obstruction.
Case Description/
Methods: A 53-year-old woman with coronary artery disease and myelodysplastic syndrome presented for asymptomatic enlarging PVA. Her PVA was previously monitored for 15 years with surveillance imaging, but recent CT angiography showed significant enlargement from an original diameter of 2.3cm to 5.2cm by 6.4cm along with new cirrhosis (Figure 1). Given the rapid enlargement, interventional radiology performed a transhepatic coil embolization of the PVA. Two weeks later, the patient presented with new painless jaundice and pruritus. Lab studies showed total bilirubin of 32.9 mg/dL (direct bilirubin >20 mg/dL), ALP 2,675 U/L, ALT 152 U/L, and AST 128 U/L from previously normal baseline values. Imaging (ultrasound, CT, and MRI) revealed no evidence of biliary obstruction, and serologic workup and medication review for other etiologies of liver injury were negative. However, the suspicion for an obstructive process remained high so endoscopic ultrasound (EUS) guided liver biopsy and endoscopic retrograde cholangiopancreatography (ERCP) were performed. The liver biopsy revealed mild steatosis without evidence of cirrhosis. ERCP revealed narrowing of the common bile duct from presumed extrinsic compression due to the recently placed portal vein coils and subsequent bile leak (Figure 2). A biliary sphincterotomy was performed and a plastic stent was placed with rapid improvement in the patient’s cholestasis -- lab studies obtained one week later noted total bilirubin 3.6 mg/dL, ALP 2138 U/L, ALT 47 U/L, and AST 32 U/L.
Discussion: PVA is a focal portal venous dilation exceeding either 1.5cm in normal livers or 1.9cm in cirrhotic livers. They are rare, with fewer than 200 cases reported in the literature, and thus their management is non-standardized. Current guidelines recommend surgical intervention for PVAs with thrombosis or symptoms, while data on endovascular repair are limited. Our patient underwent stent-assisted coil embolization and later developed cholestatic liver injury. This case illustrates how endovascular PVA repair can cause extrinsic biliary obstruction even without biliary dilation on imaging, highlighting the need for a broad differential for post-procedural liver injury and awareness of this rare complication.
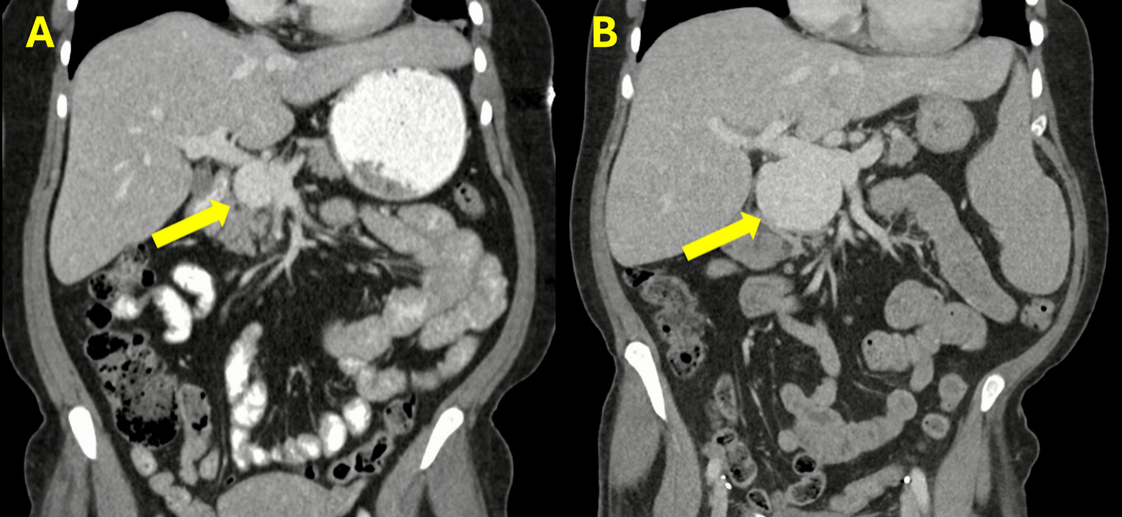
Figure: Figure 1: PVA (yellow arrow) detected incidentally 15 years prior to presentation. (B) PVA at presentation measuring 6.2 cm.
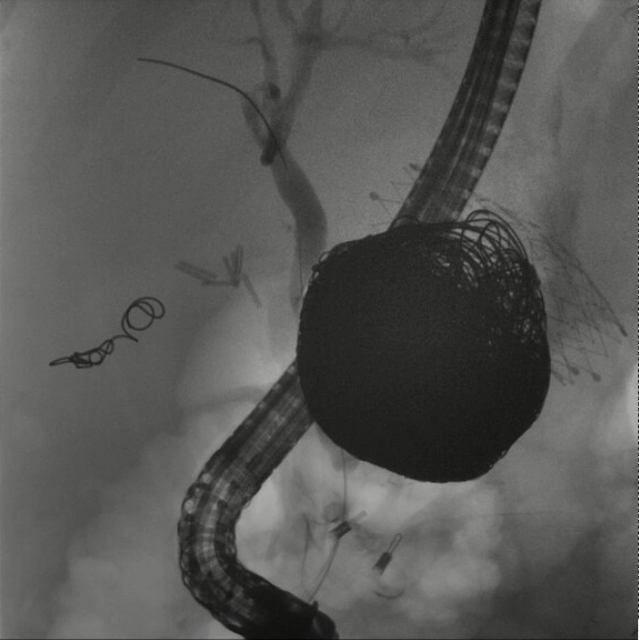
Figure: Figure 2: ERCP demonstrating mid common bile duct stricture in proximity to the coil embolization of the PVA.
Disclosures:
Olivia Battistoni indicated no relevant financial relationships.
Madeleine Davis indicated no relevant financial relationships.
Suraj Pai indicated no relevant financial relationships.
Shaoli Sun indicated no relevant financial relationships.
Marissa Guo indicated no relevant financial relationships.
Fred Karaisz indicated no relevant financial relationships.
Vivek Mendiratta indicated no relevant financial relationships.
Olivia Battistoni, MPH, BA1, Madeleine Davis, BA1, Suraj Pai, MD2, Shaoli Sun, MD2, Marissa Guo, MD2, Fred Karaisz, MD2, Vivek Mendiratta, MD3. P4463 - Biliary Complications Due to Stent-Assisted Coil Embolization of a Portal Vein Aneurysm, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
