Tuesday Poster Session
Category: Biliary/Pancreas
P4453 - Unmasking Type II Autoimmune Pancreatitis in Ulcerative Colitis: A Diagnostic and Therapeutic Challenge
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- RA
Rohan Aggarwal, MD (he/him/his)
Apollo Hospital
New Delhi, Delhi, India
Presenting Author(s)
Rohan Aggarwal, MD1, Vikarsh Bhardwaj, MD2, Sanjay Sikka, MD, FACG1, Amol Sharma, MD, MSc, FACG3, Malvika Gulati, MD1, Aishwarya Singh, MBBS1, Prackriti Masand, MD4, Sahil Kataria, MD4
1Apollo Hospital, New Delhi, Delhi, India; 2Apollo Hospital, Dothan, AL; 3Medical University of South Carolina, Charleston, SC; 4MAX Superspecialty Hospital and Vaishali, New Delhi, Delhi, India
Introduction: Ulcerative Colitis (UC) is often linked with extra-intestinal manifestations but Type II autoimmune pancreatitis (AIP-II) – remains under-recognized and rare. AIP-II is a steroid-responsive, immune-mediated form of pancreatitis that lacks IgG4 & systemic organ involvement, or reliable biomarkers. Its diagnosis is challenging due to its overlap with idiopathic pancreatitis and limitations of tissue acquisition in acute settings. We present a compelling case of probable AIP-II in a young patient with UC and axial spondyloarthritis (AS), highlighting key diagnostic considerations and the therapeutic utility of immunosuppression.
Case Description/
Methods: A 31-year-old male with a 2-year history of UC and HLA-B27-positive AS, previously treated with adalimumab, presented with acute epigastric pain and vomiting. He had two prior episodes of idiopathic acute pancreatitis. There was no history of alcohol or tobacco use, drug-induced pancreatitis, or trauma. Laboratory testing revealed leucocytosis and marked lipase elevation (3750 U/L), with normal hepatic and renal profiles. Infectious, autoimmune, genetic (PRSS1, SPINK1, CFTR, CPA1), and oncologic panels were unremarkable; serum IgG4 was within normal limits. Colonoscopy revealed active pancolitis (UCEIS 3/8), and histopathology confirmed moderate active colitis. Cross-sectional imaging (CT, MRCP) and EUS showed interstitial pancreatitis without necrosis, ductal stones, or mass lesions. Notably, MRCP identified multifocal pancreatic duct strictures and right hepatic duct irregularities, with no evidence of primary sclerosing cholangitis. Given the clinical phenotype, radiologic findings, negative biomarkers, and coexisting UC, a diagnosis of probable AIP-II was made in accordance with the ICDC. Pancreatic biopsy was deferred to avoid exacerbation. The patient was initiated on oral prednisolone, 5-ASA, and tofacitinib. Clinical resolution occurred within 5 days. Follow-up imaging after 2 weeks demonstrated complete resolution of pancreatic and biliary strictures. Lipase and CA 19-9 normalized.
Discussion: This case underscores the importance of considering AIP-II in patients with UC and recurrent idiopathic pancreatitis. Early diagnosis guided by clinical, serologic, and radiologic synthesis – rather than histology alone – is critical. Prompt steroid therapy can lead to rapid remission and obviate unnecessary interventions. Heightened awareness of AIP-II as a rare but treatable extraintestinal manifestation of UC is essential for improving outcomes.
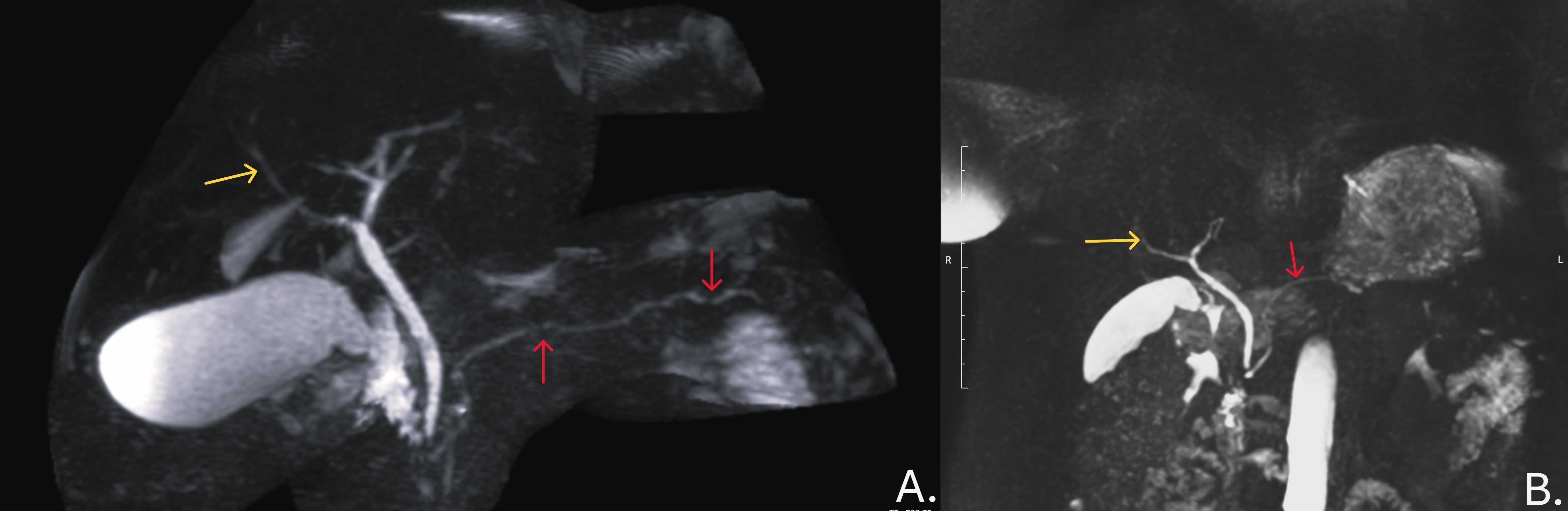
Figure: Fig1: Endoscopic and EUS images of the case: A) White-light high-definition colonoscopy image showing splenic flexure with superficial ulcers and marked erythema with friable mucosa. B) White-light high-definition colonoscopy image showing transverse colon with superficial ulcers with marked erythema. C) Red arrow showing normal portal vein flow with a yellow arrow showing normal common bile duct.

Figure: Fig2: Magnetic Resonance Cholangiopancreatography (MRCP) images from case: A) Marked multiple narrowing in main pancreatic duct without upstream dilatation (red arrows) and right hepatic duct branch narrowing (yellow arrow) B) Post-steroid 2-week response as normal main pancreatic duct without any focal stricturing (red arrow) and resolution of narrowing at right hepatic duct branch (yellow arrow).
Disclosures:
Rohan Aggarwal indicated no relevant financial relationships.
Vikarsh Bhardwaj indicated no relevant financial relationships.
Sanjay Sikka indicated no relevant financial relationships.
Amol Sharma indicated no relevant financial relationships.
Malvika Gulati indicated no relevant financial relationships.
Aishwarya Singh indicated no relevant financial relationships.
Prackriti Masand indicated no relevant financial relationships.
Sahil Kataria indicated no relevant financial relationships.
Rohan Aggarwal, MD1, Vikarsh Bhardwaj, MD2, Sanjay Sikka, MD, FACG1, Amol Sharma, MD, MSc, FACG3, Malvika Gulati, MD1, Aishwarya Singh, MBBS1, Prackriti Masand, MD4, Sahil Kataria, MD4. P4453 - Unmasking Type II Autoimmune Pancreatitis in Ulcerative Colitis: A Diagnostic and Therapeutic Challenge, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Apollo Hospital, New Delhi, Delhi, India; 2Apollo Hospital, Dothan, AL; 3Medical University of South Carolina, Charleston, SC; 4MAX Superspecialty Hospital and Vaishali, New Delhi, Delhi, India
Introduction: Ulcerative Colitis (UC) is often linked with extra-intestinal manifestations but Type II autoimmune pancreatitis (AIP-II) – remains under-recognized and rare. AIP-II is a steroid-responsive, immune-mediated form of pancreatitis that lacks IgG4 & systemic organ involvement, or reliable biomarkers. Its diagnosis is challenging due to its overlap with idiopathic pancreatitis and limitations of tissue acquisition in acute settings. We present a compelling case of probable AIP-II in a young patient with UC and axial spondyloarthritis (AS), highlighting key diagnostic considerations and the therapeutic utility of immunosuppression.
Case Description/
Methods: A 31-year-old male with a 2-year history of UC and HLA-B27-positive AS, previously treated with adalimumab, presented with acute epigastric pain and vomiting. He had two prior episodes of idiopathic acute pancreatitis. There was no history of alcohol or tobacco use, drug-induced pancreatitis, or trauma. Laboratory testing revealed leucocytosis and marked lipase elevation (3750 U/L), with normal hepatic and renal profiles. Infectious, autoimmune, genetic (PRSS1, SPINK1, CFTR, CPA1), and oncologic panels were unremarkable; serum IgG4 was within normal limits. Colonoscopy revealed active pancolitis (UCEIS 3/8), and histopathology confirmed moderate active colitis. Cross-sectional imaging (CT, MRCP) and EUS showed interstitial pancreatitis without necrosis, ductal stones, or mass lesions. Notably, MRCP identified multifocal pancreatic duct strictures and right hepatic duct irregularities, with no evidence of primary sclerosing cholangitis. Given the clinical phenotype, radiologic findings, negative biomarkers, and coexisting UC, a diagnosis of probable AIP-II was made in accordance with the ICDC. Pancreatic biopsy was deferred to avoid exacerbation. The patient was initiated on oral prednisolone, 5-ASA, and tofacitinib. Clinical resolution occurred within 5 days. Follow-up imaging after 2 weeks demonstrated complete resolution of pancreatic and biliary strictures. Lipase and CA 19-9 normalized.
Discussion: This case underscores the importance of considering AIP-II in patients with UC and recurrent idiopathic pancreatitis. Early diagnosis guided by clinical, serologic, and radiologic synthesis – rather than histology alone – is critical. Prompt steroid therapy can lead to rapid remission and obviate unnecessary interventions. Heightened awareness of AIP-II as a rare but treatable extraintestinal manifestation of UC is essential for improving outcomes.
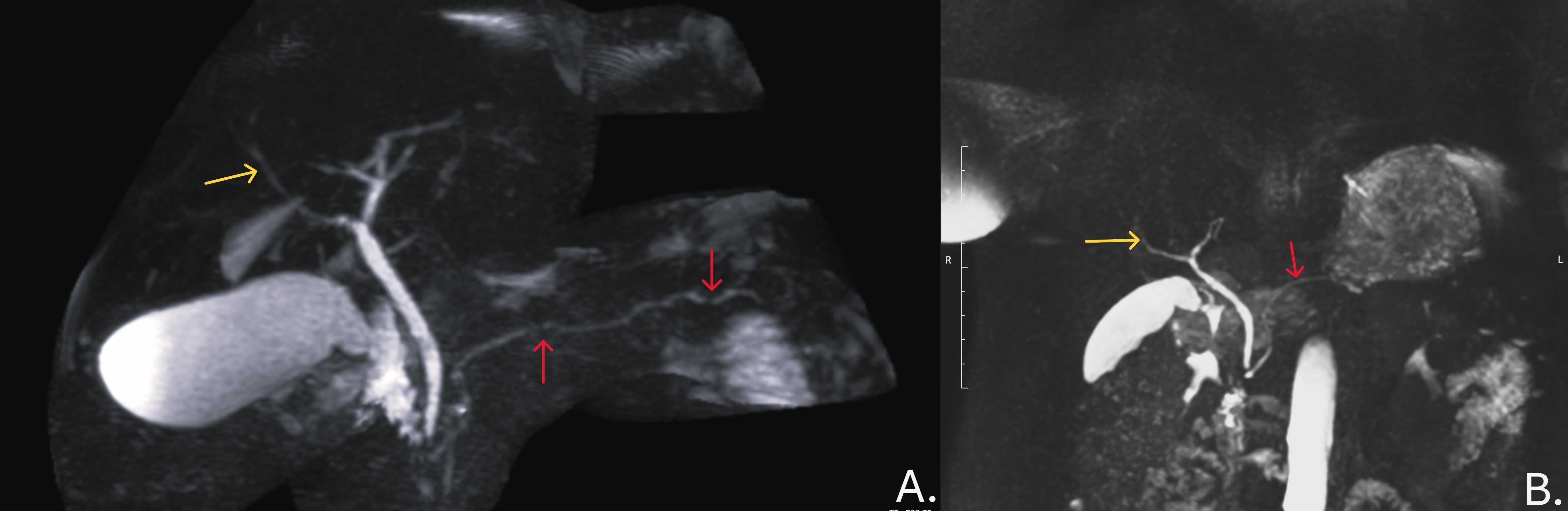
Figure: Fig1: Endoscopic and EUS images of the case: A) White-light high-definition colonoscopy image showing splenic flexure with superficial ulcers and marked erythema with friable mucosa. B) White-light high-definition colonoscopy image showing transverse colon with superficial ulcers with marked erythema. C) Red arrow showing normal portal vein flow with a yellow arrow showing normal common bile duct.

Figure: Fig2: Magnetic Resonance Cholangiopancreatography (MRCP) images from case: A) Marked multiple narrowing in main pancreatic duct without upstream dilatation (red arrows) and right hepatic duct branch narrowing (yellow arrow) B) Post-steroid 2-week response as normal main pancreatic duct without any focal stricturing (red arrow) and resolution of narrowing at right hepatic duct branch (yellow arrow).
Disclosures:
Rohan Aggarwal indicated no relevant financial relationships.
Vikarsh Bhardwaj indicated no relevant financial relationships.
Sanjay Sikka indicated no relevant financial relationships.
Amol Sharma indicated no relevant financial relationships.
Malvika Gulati indicated no relevant financial relationships.
Aishwarya Singh indicated no relevant financial relationships.
Prackriti Masand indicated no relevant financial relationships.
Sahil Kataria indicated no relevant financial relationships.
Rohan Aggarwal, MD1, Vikarsh Bhardwaj, MD2, Sanjay Sikka, MD, FACG1, Amol Sharma, MD, MSc, FACG3, Malvika Gulati, MD1, Aishwarya Singh, MBBS1, Prackriti Masand, MD4, Sahil Kataria, MD4. P4453 - Unmasking Type II Autoimmune Pancreatitis in Ulcerative Colitis: A Diagnostic and Therapeutic Challenge, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
