Tuesday Poster Session
Category: Biliary/Pancreas
P4444 - Beyond Colectomy: A Case of PSC Resolution in Refractory Ulcerative Colitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Donya Yazdi (she/her/hers)
Texas Liver Institute
Austin, TX
Presenting Author(s)
Donya Yazdi, 1, Marouane Bouchareb, MD2, Lisa D. Pedicone, PhD1, Fred Poordad, MD1, Andres Gomez-Aldana, MD1, Eugenia Tsai, MD1, Jan Petrasek, MD, PhD1, Eric Lawitz, MD3, Fabian Rodas, MD1, Carmen Landaverde, MD1
1Texas Liver Institute, Austin, TX; 2Austin Radiological Association, Austin, TX; 3Texas Liver Institute, San Antonio, TX
Introduction: Primary sclerosing cholangitis (PSC) is a chronic, autoimmune cholestatic liver disease marked by inflammation and fibrosis of the bile ducts. It can lead to biliary strictures, cirrhosis, cholangiocarcinoma and ultimately liver failure. Although its etiology remains unclear, it is strongly associated with inflammatory bowel disease (IBD), particularly ulcerative colitis (UC), which coexists in 70-80% of PSC cases. Disease course is variable: some patients remain asymptomatic for years, while others rapidly progress to end-stage liver disease or develop cholangiocarcinoma. There is no curative treatment for PSC. Liver transplantation is the only definitive treatment, though PSC recurrence occurs in up to 25% of recipients. We present a case of PSC resolution following colectomy.
Case Description/
Methods: In March 2017, a 40-year-old female (BMI: 30.2 kg/m2) with UC, diagnosed in 2011, presented to clinic with elevated liver enzymes. Further workup was remarkable for an atypical pANCA of 1:320. Magnetic Resonance Cholangiopancreatography (MRCP) showed subtle intrahepatic and extrahepatic ductal beading suggestive of PSC, without dominant strictures. She was started on ursodeoxycholic acid 300 mg BID. Bile acids were measured on 06/15/17 after starting ursodeoxycholic acid and were within normal limits at 12 µmol (reference range: 0-19 µmol/L). Due to refractory UC, she underwent total colectomy in February 2018, followed by ileostomy takedown in July. Subsequent labs showed sustained normalization of liver enzymes by May 2020, persistent to date. A 2023 MRCP showed minimal residual biliary beading, and by March 2025, imaging showed no biliary abnormalities.
Discussion: While colectomy is not generally considered curative for PSC, a cohort study on PSC-IBD patients conducted by Nordenvall et al. showed improved outcomes when colectomy preceded PSC diagnosis. Colectomy is shown to relieve UC symptoms but does not alter PSC course. However, in this case, PSC features were resolved after colectomy, possibly due to early, mild presentation. Therefore, while colectomy is not considered therapeutic for PSC, in early-stage cases with concurrent UC, it may offer unexpected benefits. Further research is necessary to explore this potential link.
<
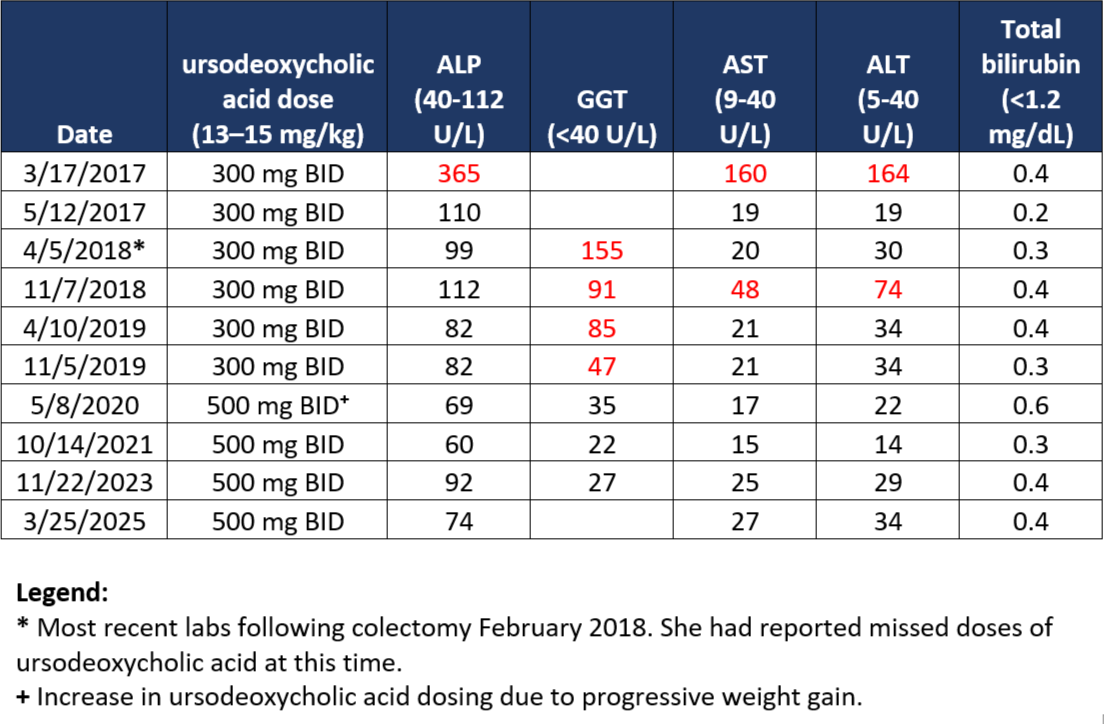
Figure: Summary of Clinical Laboratory Studies
Disclosures:
Donya Yazdi indicated no relevant financial relationships.
Marouane Bouchareb indicated no relevant financial relationships.
Lisa D. Pedicone indicated no relevant financial relationships.
Fred Poordad indicated no relevant financial relationships.
Andres Gomez-Aldana indicated no relevant financial relationships.
Eugenia Tsai indicated no relevant financial relationships.
Jan Petrasek indicated no relevant financial relationships.
Eric Lawitz: 89 Bio INC – Consultant, Grant/Research Support, Speakers Bureau. Abbvie – Speakers Bureau. Akero Therapeitics – Grant/Research Support. Alnylam Phamaceuticals INC – Grant/Research Support. Amgen – Grant/Research Support. Aztrazeneca – Consultant, Grant/Research Support. Bioscience – Grant/Research Support. Boehringer Ingelheim – Consultant, Grant/Research Support. Bristol-Myers Squibb – Grant/Research Support. Corcept Therapeutics – Consultant, Grant/Research Support. Cour Pharmaceuticals Inc – Grant/Research Support. Cymabay Therapeutics – Grant/Research Support. Eli Lily and Company – Consultant, Grant/Research Support. Enanta Pharmaceuticals – Grant/Research Support. Enyo Pharma – Grant/Research Support. Exalenz – Grant/Research Support. Galectin Therapeutics – Grant/Research Support. Galmed Pharmaceuticals – Grant/Research Support. Genfit – Grant/Research Support. Gilead Sciences – Grant/Research Support, Speakers Bureau. GlaxoSmithKline – Grant/Research Support. Hanmi Pharmaceuticals – Grant/Research Support. Hightide Biopharma – Grant/Research Support. Intercept Pharmaceuticals – Grant/Research Support, Speakers Bureau. Inventiva – Grant/Research Support. Ipsen – Grant/Research Support. Jansen Pharmaceuticals – Grant/Research Support. Madrigal Pharmaceuticals – Grant/Research Support, Speakers Bureau. Merck & Co – Consultant, Grant/Research Support. NGM Biopharmaceuticals Inc – Grant/Research Support. Northsea Therapeutics – Grant/Research Support. Novartis – Grant/Research Support. Novo Nordisk Inc – Consultant, Grant/Research Support. Organovo – Consultant, Grant/Research Support. Poxel Co – Grant/Research Support. Regeneron – Consultant, Grant/Research Support. Sagimet Biosciences – Consultant, Grant/Research Support. Takeda – Grant/Research Support. Terns pharmaceuticals – Grant/Research Support. Viking Therapeutics – Grant/Research Support. Zydus Pharmaceuticals – Grant/Research Support.
Fabian Rodas indicated no relevant financial relationships.
Carmen Landaverde indicated no relevant financial relationships.
Donya Yazdi, 1, Marouane Bouchareb, MD2, Lisa D. Pedicone, PhD1, Fred Poordad, MD1, Andres Gomez-Aldana, MD1, Eugenia Tsai, MD1, Jan Petrasek, MD, PhD1, Eric Lawitz, MD3, Fabian Rodas, MD1, Carmen Landaverde, MD1. P4444 - Beyond Colectomy: A Case of PSC Resolution in Refractory Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Texas Liver Institute, Austin, TX; 2Austin Radiological Association, Austin, TX; 3Texas Liver Institute, San Antonio, TX
Introduction: Primary sclerosing cholangitis (PSC) is a chronic, autoimmune cholestatic liver disease marked by inflammation and fibrosis of the bile ducts. It can lead to biliary strictures, cirrhosis, cholangiocarcinoma and ultimately liver failure. Although its etiology remains unclear, it is strongly associated with inflammatory bowel disease (IBD), particularly ulcerative colitis (UC), which coexists in 70-80% of PSC cases. Disease course is variable: some patients remain asymptomatic for years, while others rapidly progress to end-stage liver disease or develop cholangiocarcinoma. There is no curative treatment for PSC. Liver transplantation is the only definitive treatment, though PSC recurrence occurs in up to 25% of recipients. We present a case of PSC resolution following colectomy.
Case Description/
Methods: In March 2017, a 40-year-old female (BMI: 30.2 kg/m2) with UC, diagnosed in 2011, presented to clinic with elevated liver enzymes. Further workup was remarkable for an atypical pANCA of 1:320. Magnetic Resonance Cholangiopancreatography (MRCP) showed subtle intrahepatic and extrahepatic ductal beading suggestive of PSC, without dominant strictures. She was started on ursodeoxycholic acid 300 mg BID. Bile acids were measured on 06/15/17 after starting ursodeoxycholic acid and were within normal limits at 12 µmol (reference range: 0-19 µmol/L). Due to refractory UC, she underwent total colectomy in February 2018, followed by ileostomy takedown in July. Subsequent labs showed sustained normalization of liver enzymes by May 2020, persistent to date. A 2023 MRCP showed minimal residual biliary beading, and by March 2025, imaging showed no biliary abnormalities.
Discussion: While colectomy is not generally considered curative for PSC, a cohort study on PSC-IBD patients conducted by Nordenvall et al. showed improved outcomes when colectomy preceded PSC diagnosis. Colectomy is shown to relieve UC symptoms but does not alter PSC course. However, in this case, PSC features were resolved after colectomy, possibly due to early, mild presentation. Therefore, while colectomy is not considered therapeutic for PSC, in early-stage cases with concurrent UC, it may offer unexpected benefits. Further research is necessary to explore this potential link.
<
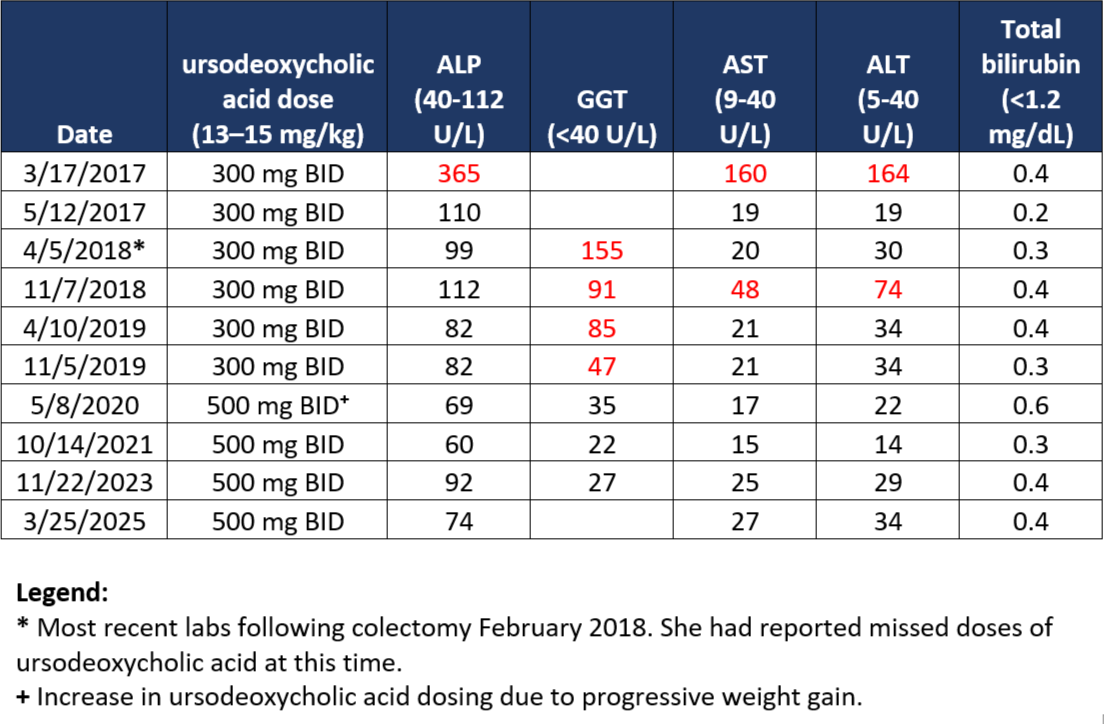
Figure: Summary of Clinical Laboratory Studies
Disclosures:
Donya Yazdi indicated no relevant financial relationships.
Marouane Bouchareb indicated no relevant financial relationships.
Lisa D. Pedicone indicated no relevant financial relationships.
Fred Poordad indicated no relevant financial relationships.
Andres Gomez-Aldana indicated no relevant financial relationships.
Eugenia Tsai indicated no relevant financial relationships.
Jan Petrasek indicated no relevant financial relationships.
Eric Lawitz: 89 Bio INC – Consultant, Grant/Research Support, Speakers Bureau. Abbvie – Speakers Bureau. Akero Therapeitics – Grant/Research Support. Alnylam Phamaceuticals INC – Grant/Research Support. Amgen – Grant/Research Support. Aztrazeneca – Consultant, Grant/Research Support. Bioscience – Grant/Research Support. Boehringer Ingelheim – Consultant, Grant/Research Support. Bristol-Myers Squibb – Grant/Research Support. Corcept Therapeutics – Consultant, Grant/Research Support. Cour Pharmaceuticals Inc – Grant/Research Support. Cymabay Therapeutics – Grant/Research Support. Eli Lily and Company – Consultant, Grant/Research Support. Enanta Pharmaceuticals – Grant/Research Support. Enyo Pharma – Grant/Research Support. Exalenz – Grant/Research Support. Galectin Therapeutics – Grant/Research Support. Galmed Pharmaceuticals – Grant/Research Support. Genfit – Grant/Research Support. Gilead Sciences – Grant/Research Support, Speakers Bureau. GlaxoSmithKline – Grant/Research Support. Hanmi Pharmaceuticals – Grant/Research Support. Hightide Biopharma – Grant/Research Support. Intercept Pharmaceuticals – Grant/Research Support, Speakers Bureau. Inventiva – Grant/Research Support. Ipsen – Grant/Research Support. Jansen Pharmaceuticals – Grant/Research Support. Madrigal Pharmaceuticals – Grant/Research Support, Speakers Bureau. Merck & Co – Consultant, Grant/Research Support. NGM Biopharmaceuticals Inc – Grant/Research Support. Northsea Therapeutics – Grant/Research Support. Novartis – Grant/Research Support. Novo Nordisk Inc – Consultant, Grant/Research Support. Organovo – Consultant, Grant/Research Support. Poxel Co – Grant/Research Support. Regeneron – Consultant, Grant/Research Support. Sagimet Biosciences – Consultant, Grant/Research Support. Takeda – Grant/Research Support. Terns pharmaceuticals – Grant/Research Support. Viking Therapeutics – Grant/Research Support. Zydus Pharmaceuticals – Grant/Research Support.
Fabian Rodas indicated no relevant financial relationships.
Carmen Landaverde indicated no relevant financial relationships.
Donya Yazdi, 1, Marouane Bouchareb, MD2, Lisa D. Pedicone, PhD1, Fred Poordad, MD1, Andres Gomez-Aldana, MD1, Eugenia Tsai, MD1, Jan Petrasek, MD, PhD1, Eric Lawitz, MD3, Fabian Rodas, MD1, Carmen Landaverde, MD1. P4444 - Beyond Colectomy: A Case of PSC Resolution in Refractory Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
