Tuesday Poster Session
Category: Biliary/Pancreas
P4439 - From Cervix to Ampulla: A Rare Cause of Biliary Obstruction
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- AB
Abakar Baraka, MD
Department of Internal Medicine, University of Colorado Anschutz Medical Campus, Aurora, Colorado
Denver, CO
Presenting Author(s)
Abakar Baraka, MD1, Thomas Enke, MD2, Blake Niccum, MD3, Mohammad Bilal, MD, FACG4
1Department of Internal Medicine, University of Colorado Anschutz Medical Campus, Aurora, Colorado, Denver, CO; 2University of Colorado, Aurora, CO; 3University of Colorado Anschutz Medical Campus, Aurora, CO; 4University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Malignant biliary obstruction is most commonly caused by primary pancreaticobiliary tumors. Metastasis to the major ampulla resulting in malignant biliary obstruction is rare, particularly from cervical squamous cell carcinoma (SCC). We present a unique case of biliary obstruction due to metastatic cervical SCC involving the major ampulla diagnosed via endoscopic biopsy despite unremarkable cross-sectional imaging.
Case Description/
Methods: A 40-year-old woman with recurrent, metastatic, p16-positive, cervical SCC on tisotumab presented with painless jaundice. Laboratory tests showed elevated liver enzymes (aspartate aminotransferase 571 U/L, alanine transaminase 1361 U/L) and total bilirubin of 11.2 mg/dL. Cross-sectional imaging revealed marked dilation of intrahepatic, extrahepatic, and pancreatic ducts without a visible mass or apparent obstruction. Endoscopic ultrasound (EUS) showed a prominent ampulla with mildly abnormal mucosa during the endoscopic exam (Figure 1). Endosonographic exam revealed marked dilation of the biliary and pancreatic ducts, however no masses or obstructing lesions were visualized. Cholangiogram performed during subsequent endoscopic cholangiopancreatography (ERCP) demonstrated diffuse intrahepatic and extrahepatic dilation with abrupt tapering of the common bile duct at the ampulla. A biliary sphincterotomy was performed, and a fully covered metal stent was placed. Biopsies of the ampulla confirmed metastatic moderately differentiated SCC, positive for p16 and p40, consistent with cervical origin. Following stent placement and biliary decompression, the patient’s liver enzymes and bilirubin normalized.
Discussion: This case highlights a rare but important manifestation of metastatic cervical SCC to the major ampulla presenting as biliary obstruction. Unlike more common causes of malignant biliary obstruction, such as pancreatic adenocarcinoma or cholangiocarcinoma, metastatic spread to the ampulla is rare and may be radiographically occult. In this patient, cross-section imaging and EUS demonstrated significant biliary and pancreatic ductal dilation without an obvious mass. The diagnosis was only established through endoscopic visualization and biopsies. This underscores the value of pursuing tissue diagnosis when clinical suspicion for malignancy remains high despite non-revealing imaging. For patients with known malignancy and unexplained biliary obstruction, ampullary metastasis should remain in the differential.
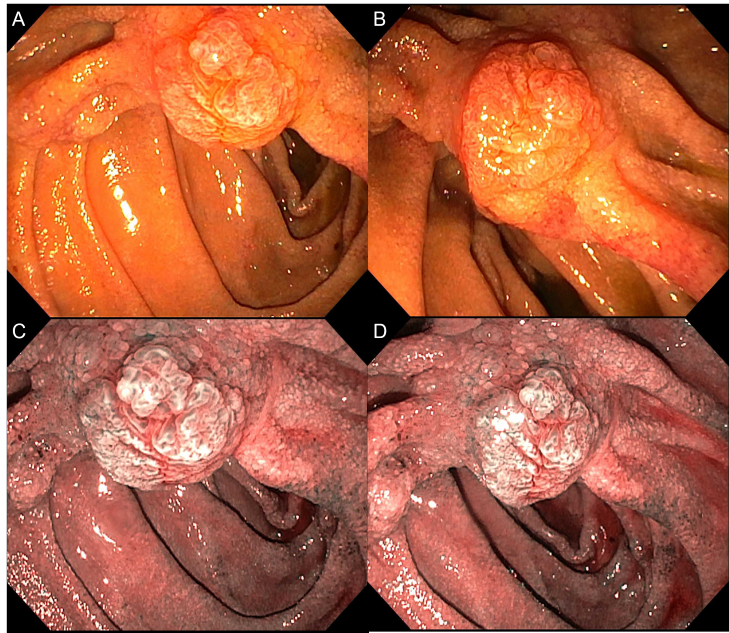
Figure: Figure 1. Prominent major ampulla with mildly abnormal mucosa visualized using high-definition white light endoscopy (A, B) and virtual chromoendoscopy (C, D).
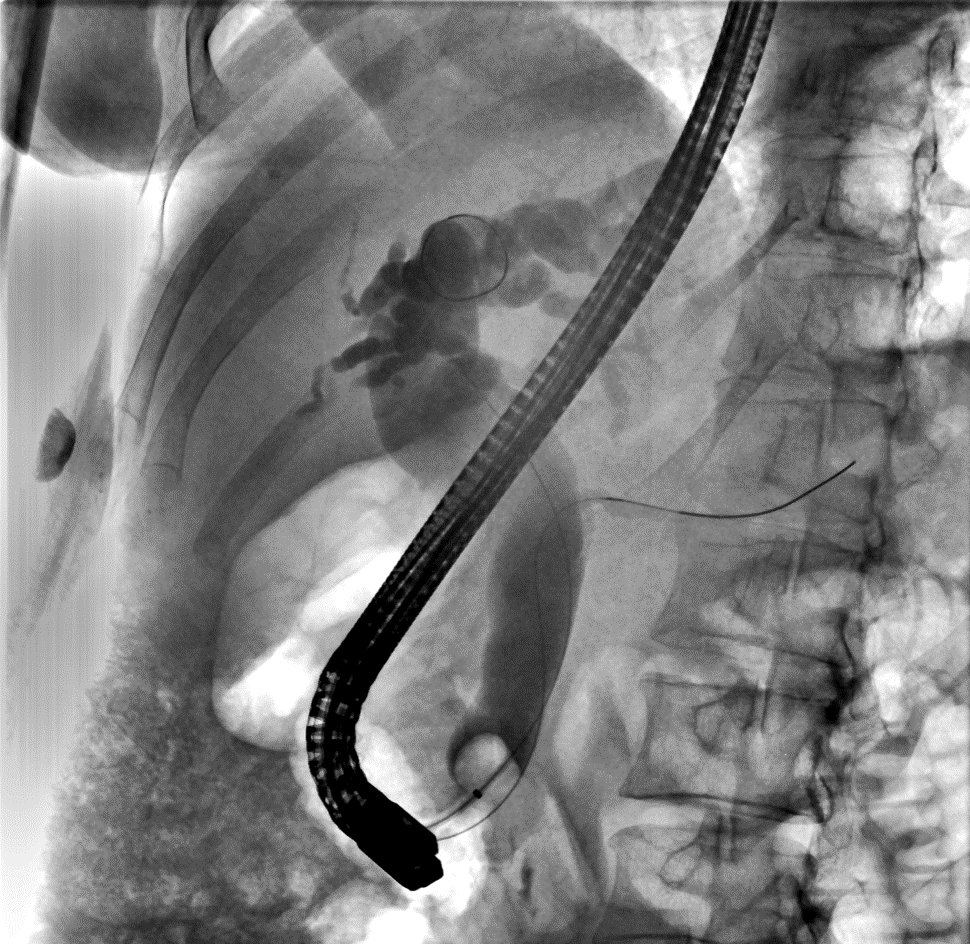
Figure: Figure 2. Cholangiogram with marked dilation of the intrahepatic and extrahepatic bile ducts with smooth tapering at the level of the ampulla.
Disclosures:
Abakar Baraka indicated no relevant financial relationships.
Thomas Enke indicated no relevant financial relationships.
Blake Niccum indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Abakar Baraka, MD1, Thomas Enke, MD2, Blake Niccum, MD3, Mohammad Bilal, MD, FACG4. P4439 - From Cervix to Ampulla: A Rare Cause of Biliary Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Internal Medicine, University of Colorado Anschutz Medical Campus, Aurora, Colorado, Denver, CO; 2University of Colorado, Aurora, CO; 3University of Colorado Anschutz Medical Campus, Aurora, CO; 4University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Malignant biliary obstruction is most commonly caused by primary pancreaticobiliary tumors. Metastasis to the major ampulla resulting in malignant biliary obstruction is rare, particularly from cervical squamous cell carcinoma (SCC). We present a unique case of biliary obstruction due to metastatic cervical SCC involving the major ampulla diagnosed via endoscopic biopsy despite unremarkable cross-sectional imaging.
Case Description/
Methods: A 40-year-old woman with recurrent, metastatic, p16-positive, cervical SCC on tisotumab presented with painless jaundice. Laboratory tests showed elevated liver enzymes (aspartate aminotransferase 571 U/L, alanine transaminase 1361 U/L) and total bilirubin of 11.2 mg/dL. Cross-sectional imaging revealed marked dilation of intrahepatic, extrahepatic, and pancreatic ducts without a visible mass or apparent obstruction. Endoscopic ultrasound (EUS) showed a prominent ampulla with mildly abnormal mucosa during the endoscopic exam (Figure 1). Endosonographic exam revealed marked dilation of the biliary and pancreatic ducts, however no masses or obstructing lesions were visualized. Cholangiogram performed during subsequent endoscopic cholangiopancreatography (ERCP) demonstrated diffuse intrahepatic and extrahepatic dilation with abrupt tapering of the common bile duct at the ampulla. A biliary sphincterotomy was performed, and a fully covered metal stent was placed. Biopsies of the ampulla confirmed metastatic moderately differentiated SCC, positive for p16 and p40, consistent with cervical origin. Following stent placement and biliary decompression, the patient’s liver enzymes and bilirubin normalized.
Discussion: This case highlights a rare but important manifestation of metastatic cervical SCC to the major ampulla presenting as biliary obstruction. Unlike more common causes of malignant biliary obstruction, such as pancreatic adenocarcinoma or cholangiocarcinoma, metastatic spread to the ampulla is rare and may be radiographically occult. In this patient, cross-section imaging and EUS demonstrated significant biliary and pancreatic ductal dilation without an obvious mass. The diagnosis was only established through endoscopic visualization and biopsies. This underscores the value of pursuing tissue diagnosis when clinical suspicion for malignancy remains high despite non-revealing imaging. For patients with known malignancy and unexplained biliary obstruction, ampullary metastasis should remain in the differential.
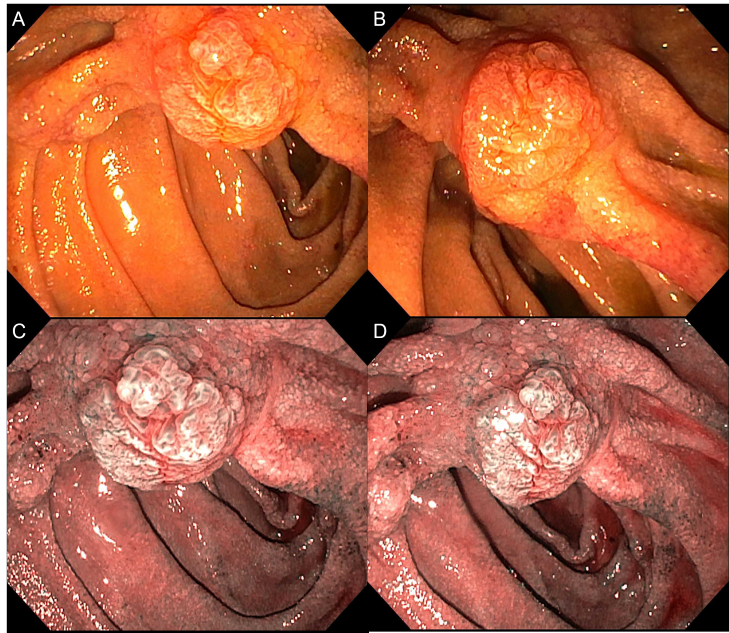
Figure: Figure 1. Prominent major ampulla with mildly abnormal mucosa visualized using high-definition white light endoscopy (A, B) and virtual chromoendoscopy (C, D).
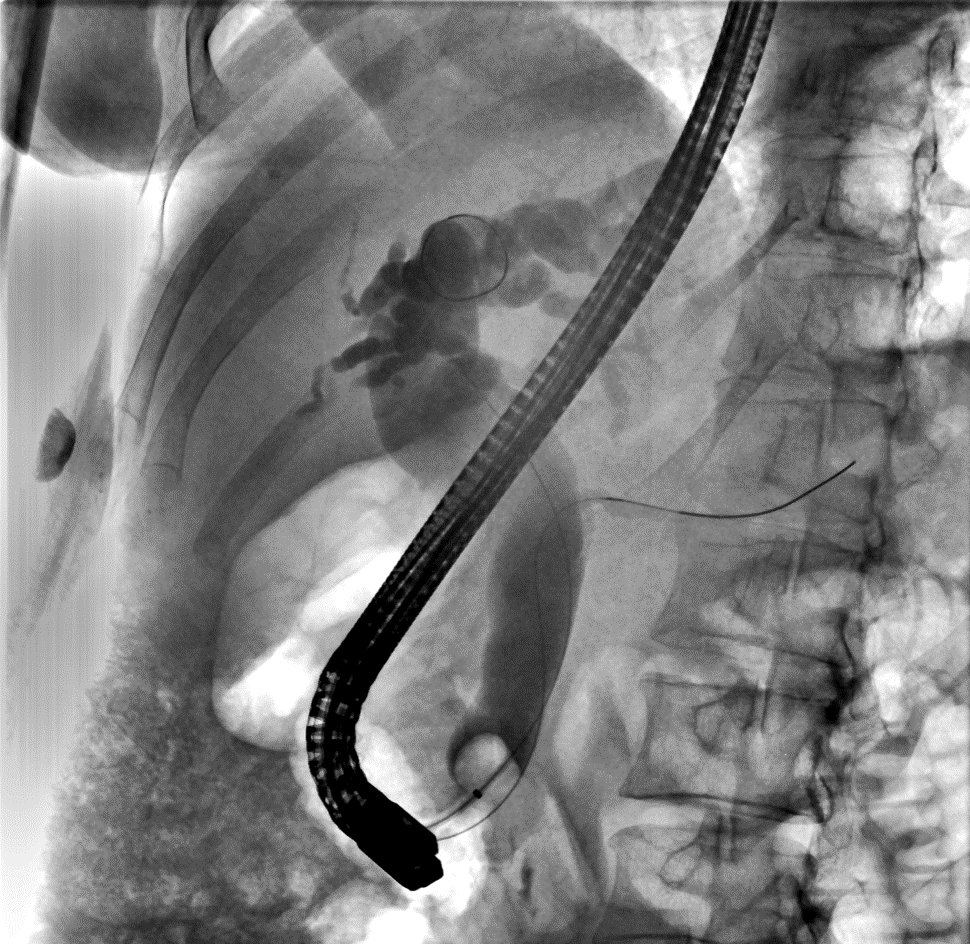
Figure: Figure 2. Cholangiogram with marked dilation of the intrahepatic and extrahepatic bile ducts with smooth tapering at the level of the ampulla.
Disclosures:
Abakar Baraka indicated no relevant financial relationships.
Thomas Enke indicated no relevant financial relationships.
Blake Niccum indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Abakar Baraka, MD1, Thomas Enke, MD2, Blake Niccum, MD3, Mohammad Bilal, MD, FACG4. P4439 - From Cervix to Ampulla: A Rare Cause of Biliary Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
