Tuesday Poster Session
Category: Biliary/Pancreas
P4411 - Very Important Perpetrator: A Patient with Chronic Secretory Diarrhea
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SP
Shree A. Patel, MD (he/him/his)
Emory University School of Medicine
Atlanta, GA
Presenting Author(s)
Shree A. Patel, MD1, Ted G. Xiao, MD, MS1, Youssef Saklawi, MD2
1Emory University School of Medicine, Atlanta, GA; 2Emory University, Atlanta, GA
Introduction: Chronic secretory diarrhea has a limited differential diagnosis—if initial work-up is unrevealing, a thorough evaluation for neuroendocrine tumors should be pursued.
Case Description/
Methods: A 46-year-old male with insulin-dependent type 2 diabetes mellitus who presents with a two-year history of chronic watery diarrhea. He reports 6–7 loose, tea-colored stools per day, occurring independently of fasting and persisting at night. There is no associated hematochezia, melena, abdominal pain, or dyspepsia. One year prior, he was hospitalized for similar symptoms. Stool studies, including cultures as well as ova/parasite testing, were unrevealing. Fecal fat was normal, but pancreatic elastase was low at 48. Anti-tTG IgG was elevated at 53.6, with a negative anti-tTG IgA. Stool studies were consistent with secretory diarrhea. Subsequent VIP levels were found to be elevated at 116 pg/mL. However, CT imaging showed no identifiable tumor. Subsequent MRI, performed a year later due to barriers to follow-up, again showed no tumor. The patient then underwent an esophagogastroduodenoscopy and colonoscopy which was only notable for grade B reflux esophagitis. Repeat VIP levels were normal at 20 pg/mL confounding this patient’s work-up. Subsequently, Chromogranin A levels were found to be elevated at 1,314. The patient returned to the hospital with severe fatigue, anemia, hypokalemia, and persistent diarrhea. Despite volume repletion and sodium bicarbonate, he had persistent non-anion gap metabolic acidosis. Given ongoing symptoms, a PET Dotatate scan was performed, revealing focal pancreatic uptake suggestive of a neuroendocrine tumor (VIPoma). He was discharged home with planned follow-up for endoscopic ultrasound and initiation of octreotide for symptom management.
Discussion: This case highlights the importance of maintaining a high index of suspicion for VIPoma in chronic secretory diarrhea, even with fluctuating VIP levels and negative initial imaging. In this case, persistent symptoms and abnormal laboratory values warranted continued investigation including the utilization of neuroendocrine markers such as Chromogranin A and functional imaging. Timely identification of VIPoma is critical, as delayed diagnosis can lead to significant morbidity due to chronic electrolyte disturbances, dehydration, and metabolic derangements. This case underscores the need for a comprehensive diagnostic approach in patients with suspected VIPoma.
*ChatGPT used for grammar review
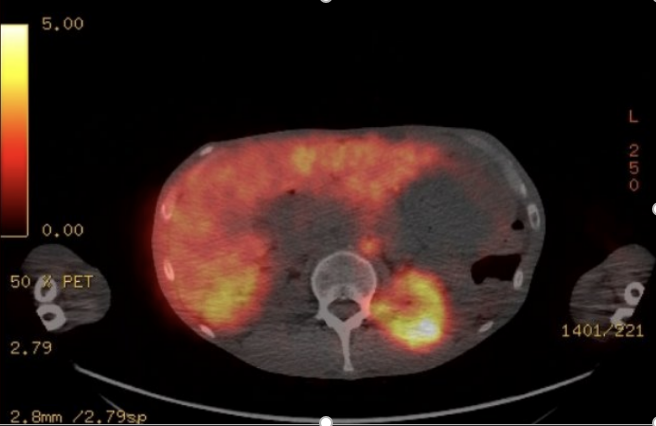
Figure: PET CT Cu64 Dotatate Scan showing focal radiotracer uptake within the pancreatic body representing underlying neuroendocrine tumor
Disclosures:
Shree Patel indicated no relevant financial relationships.
Ted Xiao indicated no relevant financial relationships.
Youssef Saklawi indicated no relevant financial relationships.
Shree A. Patel, MD1, Ted G. Xiao, MD, MS1, Youssef Saklawi, MD2. P4411 - Very Important Perpetrator: A Patient with Chronic Secretory Diarrhea, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Emory University School of Medicine, Atlanta, GA; 2Emory University, Atlanta, GA
Introduction: Chronic secretory diarrhea has a limited differential diagnosis—if initial work-up is unrevealing, a thorough evaluation for neuroendocrine tumors should be pursued.
Case Description/
Methods: A 46-year-old male with insulin-dependent type 2 diabetes mellitus who presents with a two-year history of chronic watery diarrhea. He reports 6–7 loose, tea-colored stools per day, occurring independently of fasting and persisting at night. There is no associated hematochezia, melena, abdominal pain, or dyspepsia. One year prior, he was hospitalized for similar symptoms. Stool studies, including cultures as well as ova/parasite testing, were unrevealing. Fecal fat was normal, but pancreatic elastase was low at 48. Anti-tTG IgG was elevated at 53.6, with a negative anti-tTG IgA. Stool studies were consistent with secretory diarrhea. Subsequent VIP levels were found to be elevated at 116 pg/mL. However, CT imaging showed no identifiable tumor. Subsequent MRI, performed a year later due to barriers to follow-up, again showed no tumor. The patient then underwent an esophagogastroduodenoscopy and colonoscopy which was only notable for grade B reflux esophagitis. Repeat VIP levels were normal at 20 pg/mL confounding this patient’s work-up. Subsequently, Chromogranin A levels were found to be elevated at 1,314. The patient returned to the hospital with severe fatigue, anemia, hypokalemia, and persistent diarrhea. Despite volume repletion and sodium bicarbonate, he had persistent non-anion gap metabolic acidosis. Given ongoing symptoms, a PET Dotatate scan was performed, revealing focal pancreatic uptake suggestive of a neuroendocrine tumor (VIPoma). He was discharged home with planned follow-up for endoscopic ultrasound and initiation of octreotide for symptom management.
Discussion: This case highlights the importance of maintaining a high index of suspicion for VIPoma in chronic secretory diarrhea, even with fluctuating VIP levels and negative initial imaging. In this case, persistent symptoms and abnormal laboratory values warranted continued investigation including the utilization of neuroendocrine markers such as Chromogranin A and functional imaging. Timely identification of VIPoma is critical, as delayed diagnosis can lead to significant morbidity due to chronic electrolyte disturbances, dehydration, and metabolic derangements. This case underscores the need for a comprehensive diagnostic approach in patients with suspected VIPoma.
*ChatGPT used for grammar review
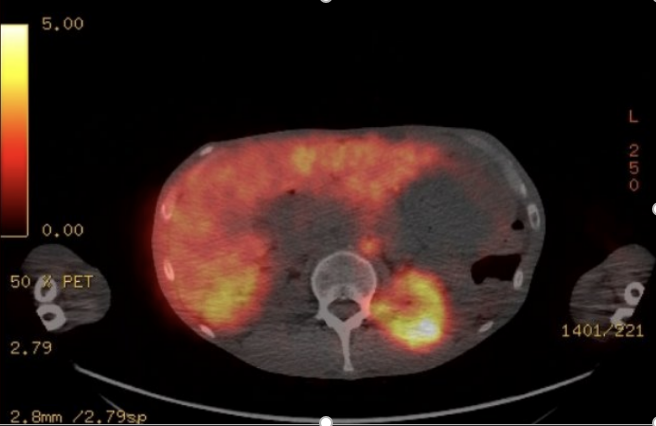
Figure: PET CT Cu64 Dotatate Scan showing focal radiotracer uptake within the pancreatic body representing underlying neuroendocrine tumor
Disclosures:
Shree Patel indicated no relevant financial relationships.
Ted Xiao indicated no relevant financial relationships.
Youssef Saklawi indicated no relevant financial relationships.
Shree A. Patel, MD1, Ted G. Xiao, MD, MS1, Youssef Saklawi, MD2. P4411 - Very Important Perpetrator: A Patient with Chronic Secretory Diarrhea, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
