Tuesday Poster Session
Category: Biliary/Pancreas
P4408 - A Rare Case of Metastatic Malignant Melanoma Mimicking Pancreatic Adenocarcinoma
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Sneh Sonaiya, MD, MPH, MBA
Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas
Las Vegas, NV
Presenting Author(s)
Sneh Sonaiya, MD, MPH, MBA, Pei Xue, MD, Rajan Amin, MD, Vignan Manne, MD
Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV
Introduction: Malignant melanoma is an aggressive skin cancer with prognosis largely dependent on stage at diagnosis—5-year survival is approximately 99.4% for localized disease but drops to 29.8% for distant metastases. Common metastatic sites include lymph nodes, lungs, brain, liver, and GI tract. Rarely, widespread melanoma may mimic other malignancies on imaging, such as pancreatic or gastrointestinal cancers, creating diagnostic challenges. We present a case of metastatic melanoma initially suspected to be pancreatic adenocarcinoma based on imaging.
Case Description/
Methods: A 60-year-old woman with hypertension and type 2 diabetes presented with three days of abdominal pain, distension, and anorexia. Initial CT imaging revealed a heterogeneous mass at the pancreatic head concerning for pancreatic adenocarcinoma, along with widespread metastases involving the liver, adrenal glands, retroperitoneum, and tumor thrombi extending into the IVC and renal veins, as well as numerous pulmonary and subcutaneous nodules [Figure 1]. IR-guided biopsy was deferred due to a lack of an adequate window, and EGD with EUS was performed. EUS showed widespread metastatic lesions but no pancreatic mass or ductal dilation. EGD revealed ulcerated gastric nodules, which were biopsied [Figure 2]. Tumor markers (CA 19-9, CEA, CA 27.29) were normal, with mild elevation in CA-125 (59 U/mL). Biopsies from gastric and hepatic lesions stained positive for pan-melanoma antigen, S100, and SOX10, with minimal patchy staining for cytokeratin AE1/AE3, confirming metastatic melanoma. Unfortunately, the patient’s condition deteriorated, and she passed away before oncology follow-up.
Discussion: The case highlights a rare presentation of metastatic melanoma initially mistaken for pancreatic adenocarcinoma. The absence of a pancreatic mass or ductal dilation on EUS, along with normal tumor markers, prompted reconsideration. Melanoma of unknown primary, though rare, often presents with widespread disease. In this case, histology from hepatic and gastric lesions confirmed the diagnosis. This case demonstrates metastatic melanoma can mimic gastrointestinal malignancies, underscoring the importance of maintaining a broad differential in cases of metastatic disease. After the patient’s passing, the family reported a previously unexamined skin lesion—a detail that may have altered the diagnostic course. This case also highlights the value of a thorough physical exam and the need to avoid anchoring bias when imaging suggests a specific diagnosis.
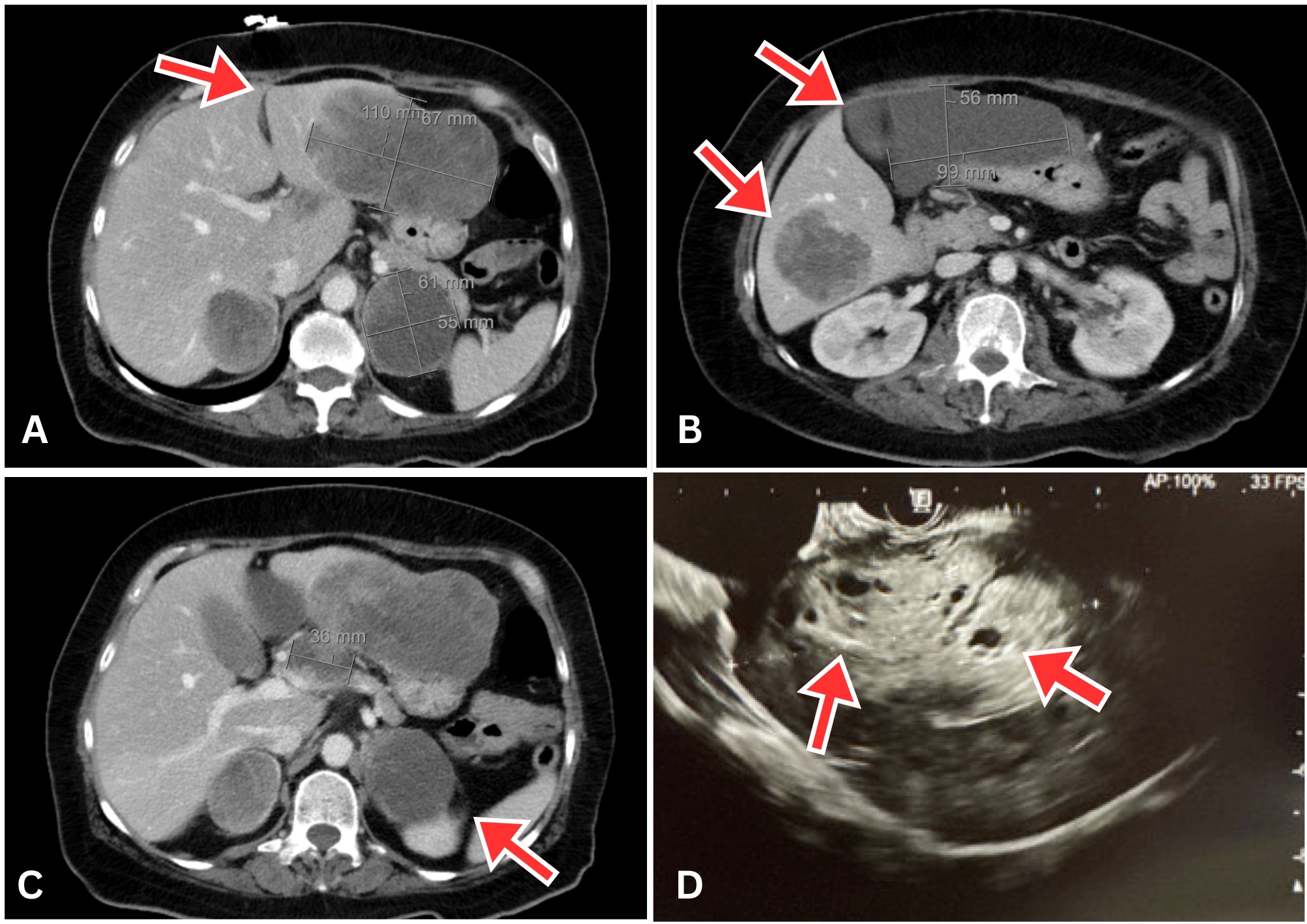
Figure: A–C. Axial contrast-enhanced CT images of the abdomen showing a large exophytic heterogeneous mass at the pancreatic head (3.7 × 3.2 cm) abutting the caudate lobe of the liver. Extensive metastatic disease is noted, including large lesions in the liver, bilateral adrenal glands, and retroperitoneum (red arrows).
D. Endoscopic ultrasound (EUS) of the liver demonstrating multiple hypoechoic lesions (red arrows) consistent with hepatic metastases. Notably, no pancreatic mass or pancreatic ductal dilation was visualized on EUS.
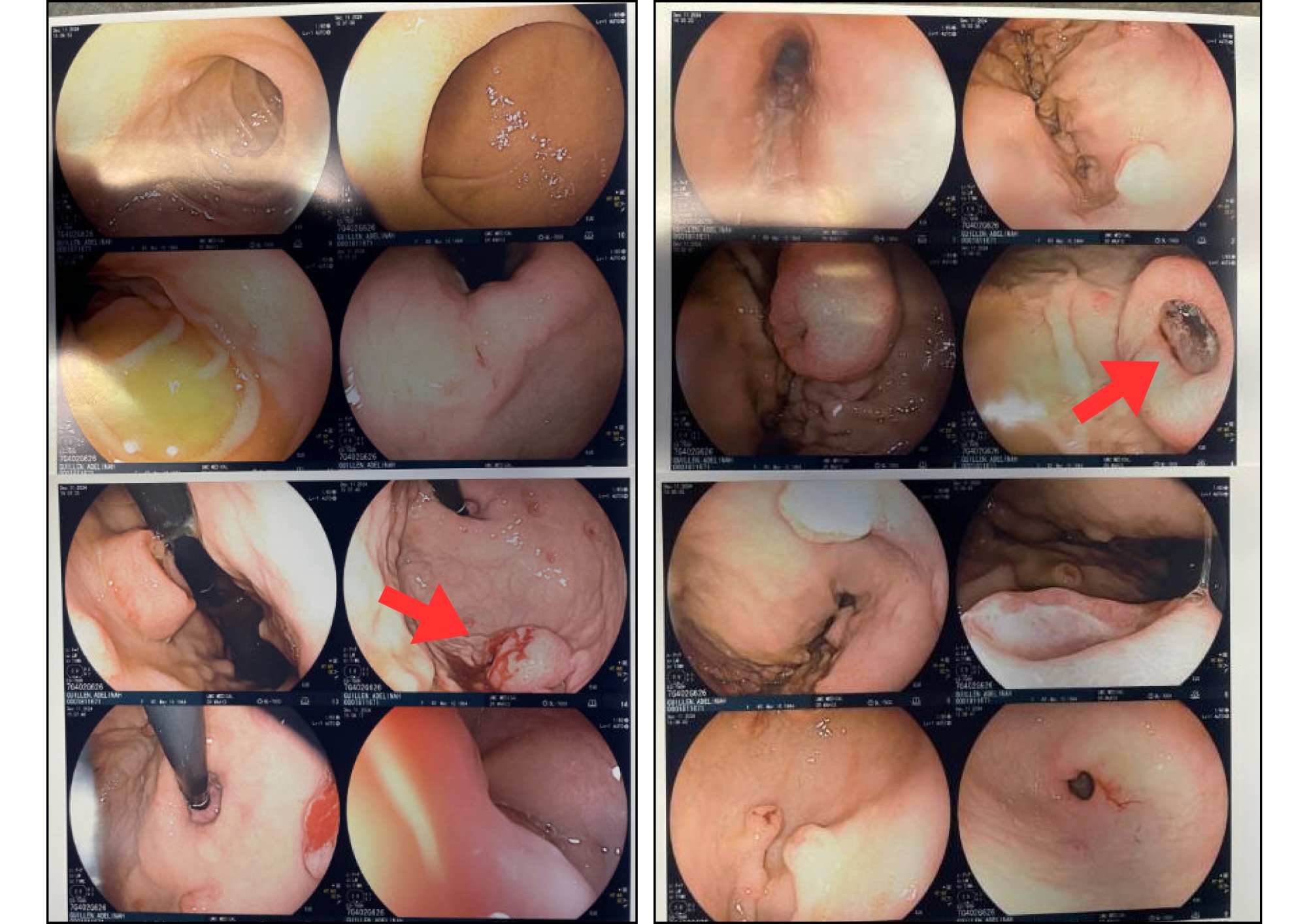
Figure: Esophagogastroduodenoscopy (EGD) revealed multiple ulcerated gastric nodules (red arrows).
These lesions were biopsied and, in conjunction with EUS-guided liver biopsy, were histologically confirmed to be metastatic malignant melanoma.
Disclosures:
Sneh Sonaiya indicated no relevant financial relationships.
Pei Xue indicated no relevant financial relationships.
Rajan Amin indicated no relevant financial relationships.
Vignan Manne indicated no relevant financial relationships.
Sneh Sonaiya, MD, MPH, MBA, Pei Xue, MD, Rajan Amin, MD, Vignan Manne, MD. P4408 - A Rare Case of Metastatic Malignant Melanoma Mimicking Pancreatic Adenocarcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV
Introduction: Malignant melanoma is an aggressive skin cancer with prognosis largely dependent on stage at diagnosis—5-year survival is approximately 99.4% for localized disease but drops to 29.8% for distant metastases. Common metastatic sites include lymph nodes, lungs, brain, liver, and GI tract. Rarely, widespread melanoma may mimic other malignancies on imaging, such as pancreatic or gastrointestinal cancers, creating diagnostic challenges. We present a case of metastatic melanoma initially suspected to be pancreatic adenocarcinoma based on imaging.
Case Description/
Methods: A 60-year-old woman with hypertension and type 2 diabetes presented with three days of abdominal pain, distension, and anorexia. Initial CT imaging revealed a heterogeneous mass at the pancreatic head concerning for pancreatic adenocarcinoma, along with widespread metastases involving the liver, adrenal glands, retroperitoneum, and tumor thrombi extending into the IVC and renal veins, as well as numerous pulmonary and subcutaneous nodules [Figure 1]. IR-guided biopsy was deferred due to a lack of an adequate window, and EGD with EUS was performed. EUS showed widespread metastatic lesions but no pancreatic mass or ductal dilation. EGD revealed ulcerated gastric nodules, which were biopsied [Figure 2]. Tumor markers (CA 19-9, CEA, CA 27.29) were normal, with mild elevation in CA-125 (59 U/mL). Biopsies from gastric and hepatic lesions stained positive for pan-melanoma antigen, S100, and SOX10, with minimal patchy staining for cytokeratin AE1/AE3, confirming metastatic melanoma. Unfortunately, the patient’s condition deteriorated, and she passed away before oncology follow-up.
Discussion: The case highlights a rare presentation of metastatic melanoma initially mistaken for pancreatic adenocarcinoma. The absence of a pancreatic mass or ductal dilation on EUS, along with normal tumor markers, prompted reconsideration. Melanoma of unknown primary, though rare, often presents with widespread disease. In this case, histology from hepatic and gastric lesions confirmed the diagnosis. This case demonstrates metastatic melanoma can mimic gastrointestinal malignancies, underscoring the importance of maintaining a broad differential in cases of metastatic disease. After the patient’s passing, the family reported a previously unexamined skin lesion—a detail that may have altered the diagnostic course. This case also highlights the value of a thorough physical exam and the need to avoid anchoring bias when imaging suggests a specific diagnosis.
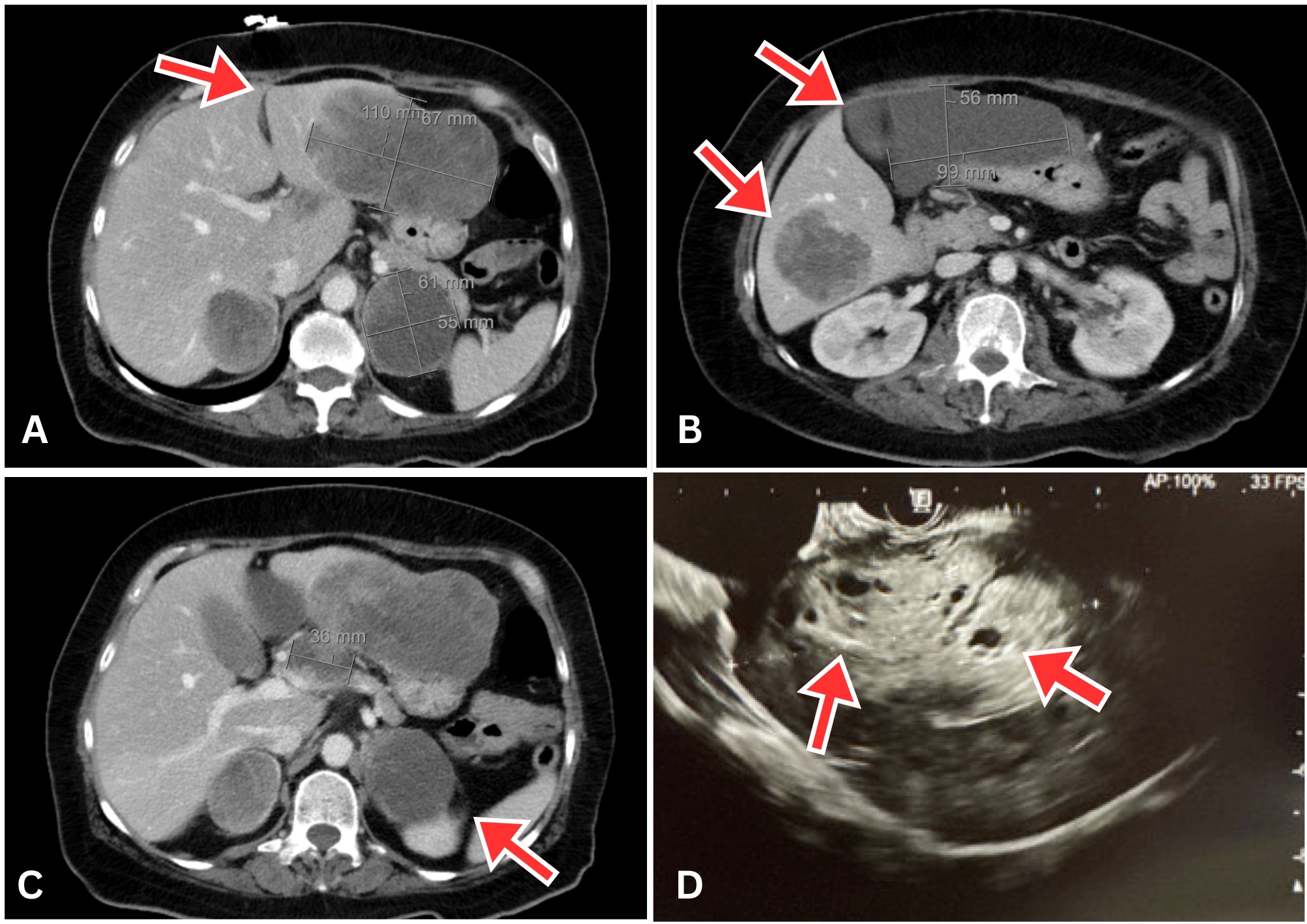
Figure: A–C. Axial contrast-enhanced CT images of the abdomen showing a large exophytic heterogeneous mass at the pancreatic head (3.7 × 3.2 cm) abutting the caudate lobe of the liver. Extensive metastatic disease is noted, including large lesions in the liver, bilateral adrenal glands, and retroperitoneum (red arrows).
D. Endoscopic ultrasound (EUS) of the liver demonstrating multiple hypoechoic lesions (red arrows) consistent with hepatic metastases. Notably, no pancreatic mass or pancreatic ductal dilation was visualized on EUS.
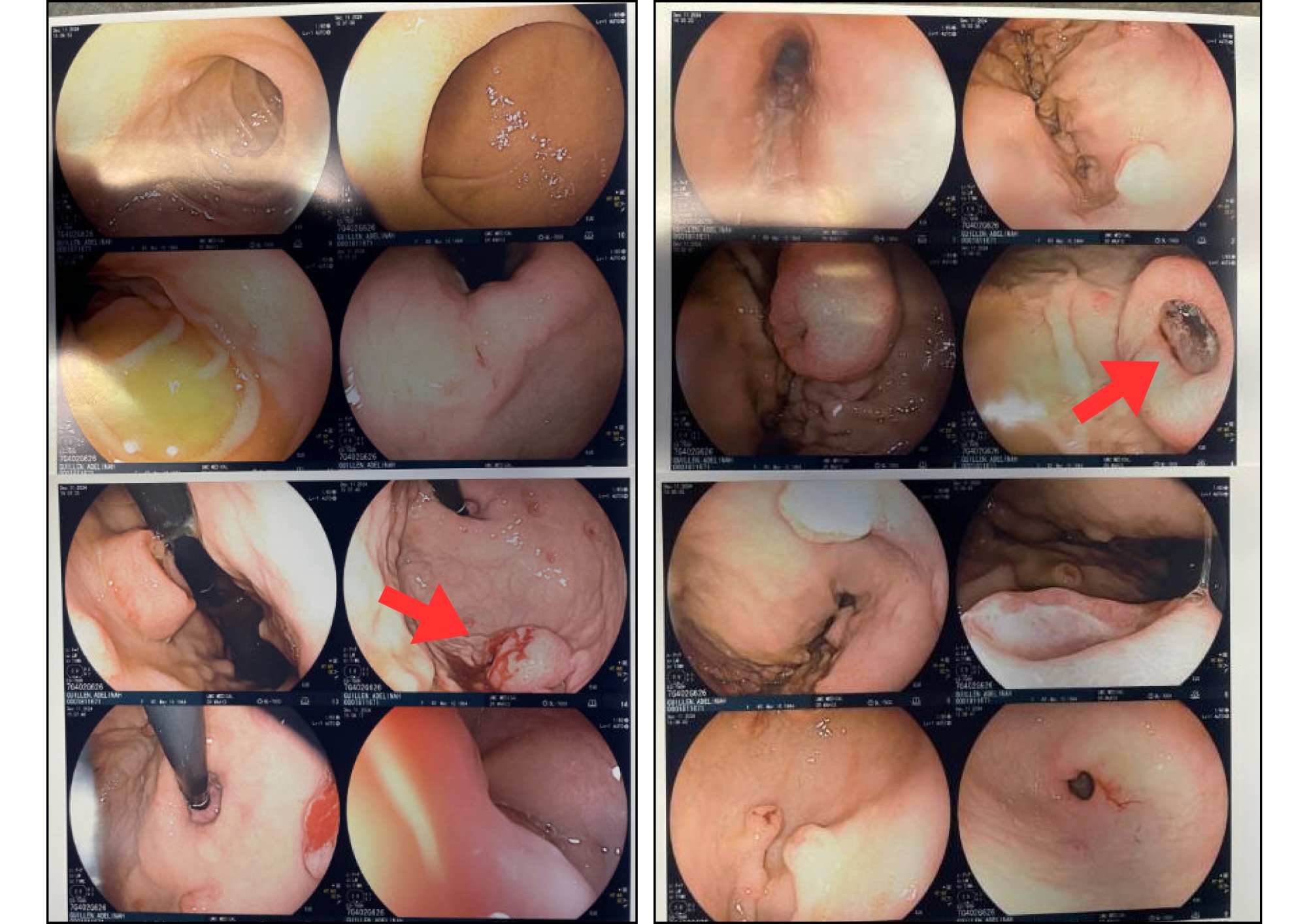
Figure: Esophagogastroduodenoscopy (EGD) revealed multiple ulcerated gastric nodules (red arrows).
These lesions were biopsied and, in conjunction with EUS-guided liver biopsy, were histologically confirmed to be metastatic malignant melanoma.
Disclosures:
Sneh Sonaiya indicated no relevant financial relationships.
Pei Xue indicated no relevant financial relationships.
Rajan Amin indicated no relevant financial relationships.
Vignan Manne indicated no relevant financial relationships.
Sneh Sonaiya, MD, MPH, MBA, Pei Xue, MD, Rajan Amin, MD, Vignan Manne, MD. P4408 - A Rare Case of Metastatic Malignant Melanoma Mimicking Pancreatic Adenocarcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
