Tuesday Poster Session
Category: Biliary/Pancreas
P4384 - Genetic Clues in Recurrent Idiopathic Pancreatitis: A Case of CFTR 3120+1G>A Mutation
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Vishnu Prasad Chowdary Sudnagunta, MD, MBBS
BronxCare Health System
Bronx, NY
Presenting Author(s)
Vishnu Prasad Chowdary. Sudnagunta, MD, MBBS, Lisbeth Sosa, MD, June Gorriceta, MD, Franklin Sosa, MD, Priscilla Hallal, MD, Harish Patel, MD
BronxCare Health System, Bronx, NY
Introduction: Acute pancreatitis is a common clinical condition characterized by inflammation of the pancreas, requiring hospitalization, severity stratification, fluid resuscitation, and etiologic evaluation. While gallstones and alcohol are the most common causes, congenital and genetic contributors are often underrecognized, particularly in cases of recurrent or idiopathic pancreatitis.
Case Description/
Methods: A 42-year-old female presented to the emergency department with one day of progressive abdominal pain, nausea, and bloating. Her vital signs were notable for a blood pressure of 135/90 mmHg, heart rate of 103 bpm, respiratory rate of 19 breaths/min, and a temperature of 37.1°C. Laboratory testing revealed a lipase level of 282 U/L (Table -1) . A contrast-enhanced CT scan of the abdomen showed findings consistent with acute pancreatitis and hepatic steatosis (Figure-1) . She reported a prior episode of acute pancreatitis and denied alcohol use. Abdominal ultrasound showed no evidence of gallstones. The patient was adopted, and no family history was available. She denied medication use, and magnetic resonance cholangiopancreatography (MRCP) was scheduled for further evaluation.
Of note, in 2016, during a pregnancy, the patient underwent genetic screening and was found to be a heterozygous carrier of the CFTR mutation 3120+1G >A, a known pathogenic variant. She declined prenatal genetic testing at the time. She denied any respiratory symptoms, chronic diarrhea, or a history suggestive of cystic fibrosis. Imaging studies revealed no features of chronic pancreatitis.
Discussion: Recurrent pancreatitis in patients without gallstones or alcohol use warrants evaluation for metabolic, structural, and genetic causes. Among the genetic contributors, CFTR, PRSS1, and SPINK1 mutations are increasingly recognized as causes of pancreatitis in individuals without classic cystic fibrosis. CFTR mutations like 3120+1G >A may impair pancreatic ductal function and contribute to recurrent inflammation, even in the absence of pulmonary or gastrointestinal manifestations of cystic fibrosis. This case highlights the importance of considering genetic testing in idiopathic recurrent pancreatitis and tailoring management accordingly. In addition to standard supportive care, genetic counseling and long-term surveillance are essential to optimize outcomes and prevent complications

Figure: Figure 1. CT Abdomen and Pelvis with Intravenous Contrast
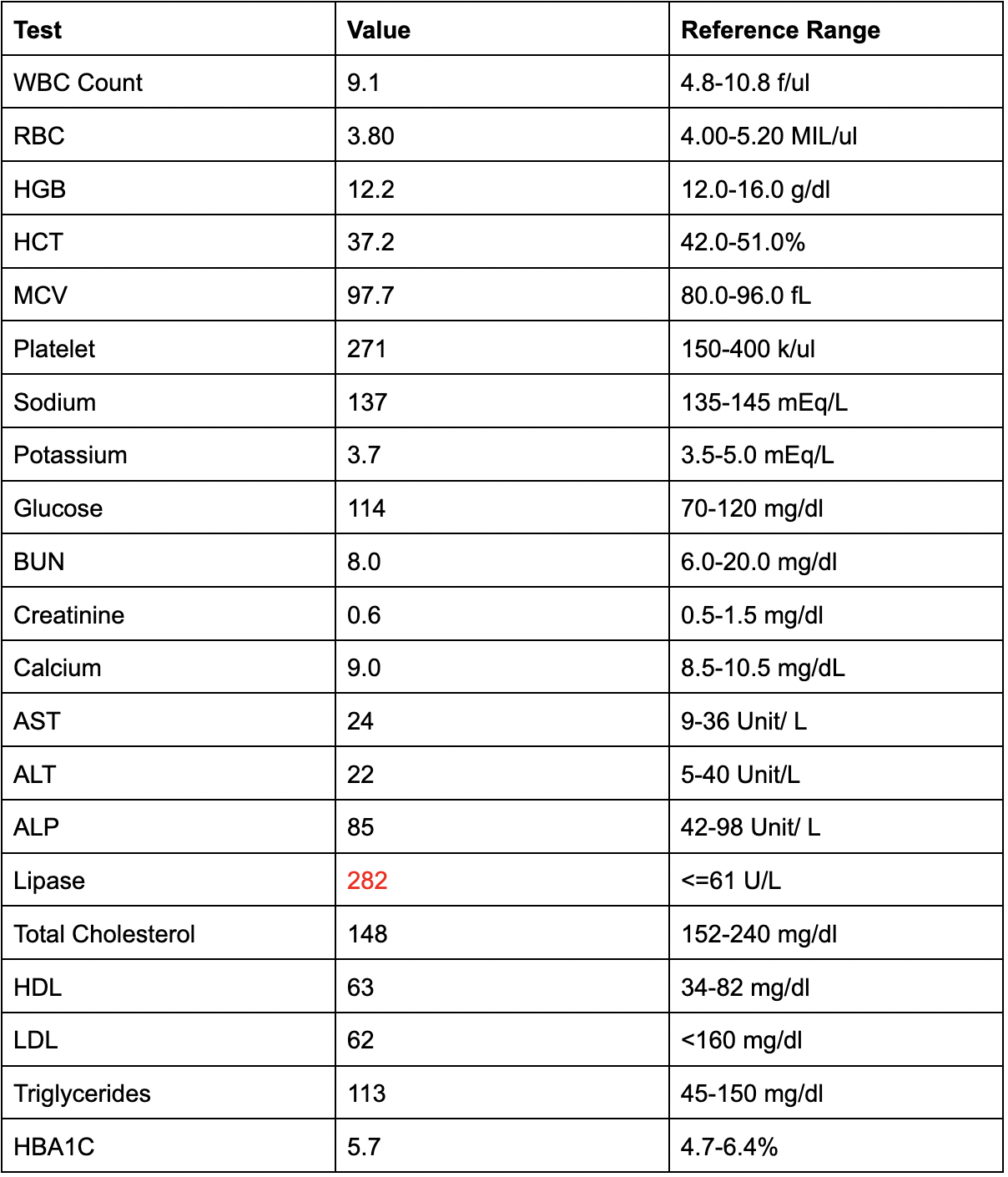
Figure: Table -1: Laboratory Values at the Time of Presentation
Disclosures:
Vishnu Sudnagunta indicated no relevant financial relationships.
Lisbeth Sosa indicated no relevant financial relationships.
June Gorriceta indicated no relevant financial relationships.
Franklin Sosa indicated no relevant financial relationships.
Priscilla Hallal indicated no relevant financial relationships.
Harish Patel indicated no relevant financial relationships.
Vishnu Prasad Chowdary. Sudnagunta, MD, MBBS, Lisbeth Sosa, MD, June Gorriceta, MD, Franklin Sosa, MD, Priscilla Hallal, MD, Harish Patel, MD. P4384 - Genetic Clues in Recurrent Idiopathic Pancreatitis: A Case of CFTR 3120+1G>A Mutation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
BronxCare Health System, Bronx, NY
Introduction: Acute pancreatitis is a common clinical condition characterized by inflammation of the pancreas, requiring hospitalization, severity stratification, fluid resuscitation, and etiologic evaluation. While gallstones and alcohol are the most common causes, congenital and genetic contributors are often underrecognized, particularly in cases of recurrent or idiopathic pancreatitis.
Case Description/
Methods: A 42-year-old female presented to the emergency department with one day of progressive abdominal pain, nausea, and bloating. Her vital signs were notable for a blood pressure of 135/90 mmHg, heart rate of 103 bpm, respiratory rate of 19 breaths/min, and a temperature of 37.1°C. Laboratory testing revealed a lipase level of 282 U/L (Table -1) . A contrast-enhanced CT scan of the abdomen showed findings consistent with acute pancreatitis and hepatic steatosis (Figure-1) . She reported a prior episode of acute pancreatitis and denied alcohol use. Abdominal ultrasound showed no evidence of gallstones. The patient was adopted, and no family history was available. She denied medication use, and magnetic resonance cholangiopancreatography (MRCP) was scheduled for further evaluation.
Of note, in 2016, during a pregnancy, the patient underwent genetic screening and was found to be a heterozygous carrier of the CFTR mutation 3120+1G >A, a known pathogenic variant. She declined prenatal genetic testing at the time. She denied any respiratory symptoms, chronic diarrhea, or a history suggestive of cystic fibrosis. Imaging studies revealed no features of chronic pancreatitis.
Discussion: Recurrent pancreatitis in patients without gallstones or alcohol use warrants evaluation for metabolic, structural, and genetic causes. Among the genetic contributors, CFTR, PRSS1, and SPINK1 mutations are increasingly recognized as causes of pancreatitis in individuals without classic cystic fibrosis. CFTR mutations like 3120+1G >A may impair pancreatic ductal function and contribute to recurrent inflammation, even in the absence of pulmonary or gastrointestinal manifestations of cystic fibrosis. This case highlights the importance of considering genetic testing in idiopathic recurrent pancreatitis and tailoring management accordingly. In addition to standard supportive care, genetic counseling and long-term surveillance are essential to optimize outcomes and prevent complications

Figure: Figure 1. CT Abdomen and Pelvis with Intravenous Contrast
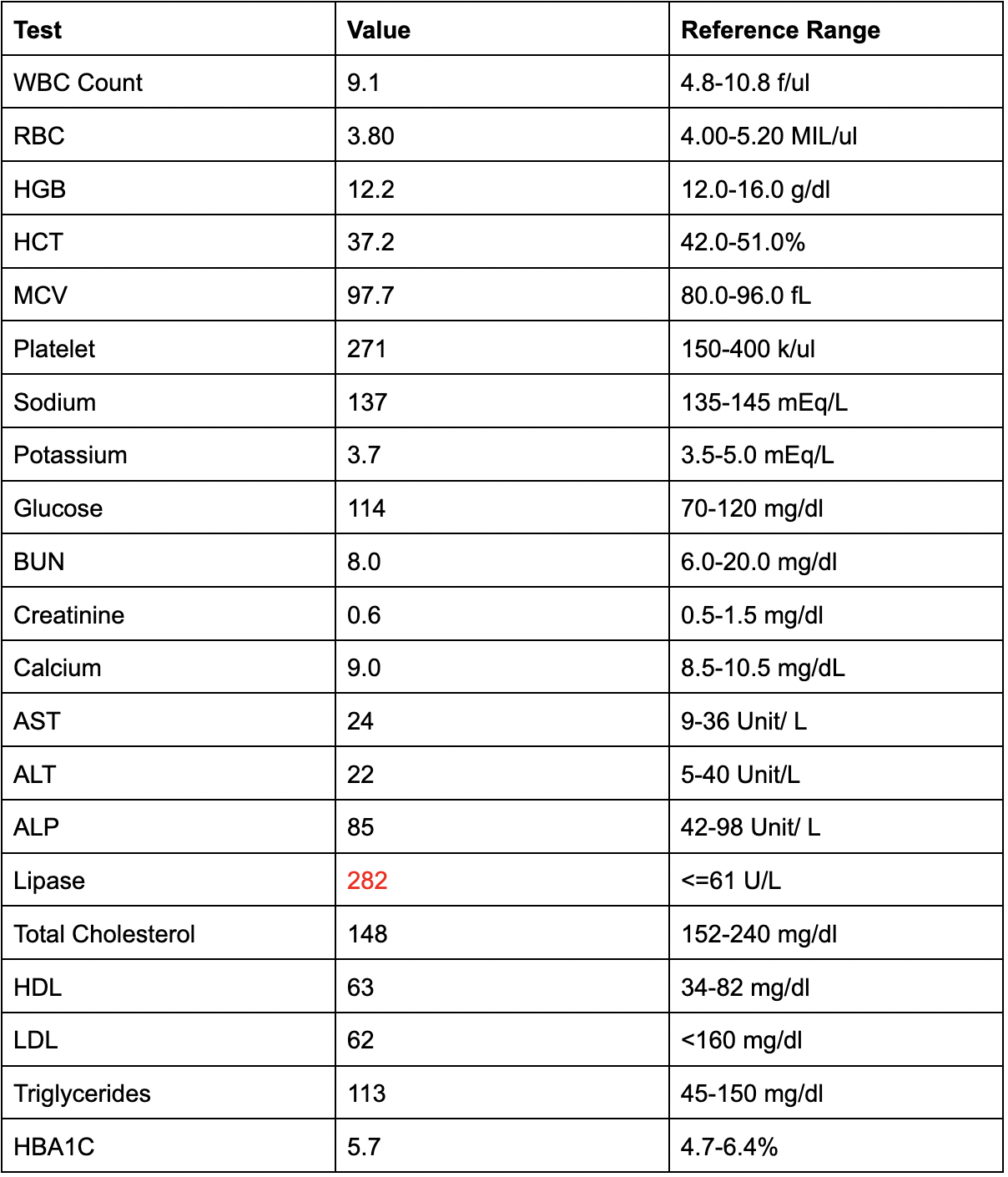
Figure: Table -1: Laboratory Values at the Time of Presentation
Disclosures:
Vishnu Sudnagunta indicated no relevant financial relationships.
Lisbeth Sosa indicated no relevant financial relationships.
June Gorriceta indicated no relevant financial relationships.
Franklin Sosa indicated no relevant financial relationships.
Priscilla Hallal indicated no relevant financial relationships.
Harish Patel indicated no relevant financial relationships.
Vishnu Prasad Chowdary. Sudnagunta, MD, MBBS, Lisbeth Sosa, MD, June Gorriceta, MD, Franklin Sosa, MD, Priscilla Hallal, MD, Harish Patel, MD. P4384 - Genetic Clues in Recurrent Idiopathic Pancreatitis: A Case of CFTR 3120+1G>A Mutation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
