Tuesday Poster Session
Category: Biliary/Pancreas
P4368 - Age ≥60 Years Predicts Higher In-Hospital Mortality in Acute Pancreatitis: A 2022 Central Pennsylvania Retrospective Cohort Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Angsupat Pornchai, MD (she/her/hers)
University of Pittsburgh Medical Center
Harrisburg, PA
Presenting Author(s)
Angsupat Pornchai, MD, Lovette Oji, MD, Evelyn Calderon, MD, Oyindamola Amosu, MD, Christina Tache, MD, Eshan Nanda, MD, Anas Atrash, MD, Raul Cantu, MD, Hajra Khan, MD
University of Pittsburgh Medical Center, Harrisburg, PA
Introduction: Acute pancreatitis (AP) is an acute inflammatory disorder of the pancreas and a major contributor to gastrointestinal-related hospitalizations globally, with substantial clinical and economic consequences. While the majority of cases resolve with mild disease, up to 20% progress to severe AP, marked by increased morbidity, mortality, and resource use, particularly in high-risk subgroups. As the population ages, older patients are experiencing a rising incidence of AP and disproportionately suffer severe complications and death. However, the influence of advanced age on in-hospital outcomes including in-hospital mortality, need for intensive care, and length of stay has not been clearly defined, and prior reports lack consistent, age-stratified data. Recognizing the unique vulnerabilities of elderly patients, our study aims to fill this gap by rigorously analyzing the relationship between age and in-hospital outcomes in AP.
Methods: We retrospectively reviewed 287 consecutive adults (≥18 years) admitted with serologically and radiographically confirmed acute pancreatitis to a Central Pennsylvania hospital in 2022. Exclusion criteria included age < 18 years, acute-on-chronic pancreatitis, incomplete demographic data, or absence of confirmatory laboratory or imaging studies. Patients were stratified into elderly (≥60 years; n = 105) and non-elderly (< 60 years; n = 182) cohorts. The primary endpoint was in-hospital mortality; secondary endpoints were intensive care unit admission and hospital length of stay (LOS). Continuous variables were assessed for normality using the Shapiro–Wilk test: normally distributed data are reported as mean ± SD (range), and non-normal data as median (interquartile range). Between-group comparisons used Student’s t-test or the Mann–Whitney U test for continuous variables, and chi-square or Fisher’s exact test for categorical variables. A two-sided P < 0.05 was considered statistically significant. All analyses were performed with SAS 9.4.
Results: Elderly patients had higher in-hospital mortality than non-elderly patients (12.4% vs 2.2%; p = 0.0004). ICU admission rates were similar (8.6% vs 6.1%; p = 0.43). Median LOS was 3 days (IQR 2–5) in elderly and 3 days (IQR 2–4) in non-elderly patients (p = 0.09).
Discussion: Elderly AP patients exhibit distinct demographic characteristics, including greater White race representation, higher partnership rates, and increased inpatient care, underscoring the need to tailor outreach and support interventions by age.
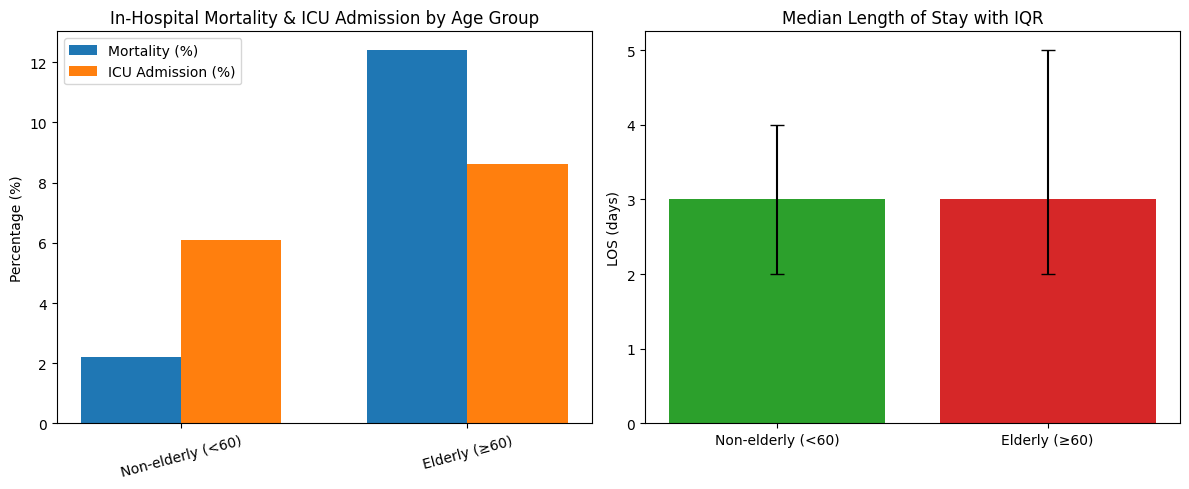
Figure: Panel 1: Bar chart showing in-hospital mortality and ICU admission rates (%)
Panel 2: Bar chart of median length-of-stay (days) with IQR error bars
Disclosures:
Angsupat Pornchai indicated no relevant financial relationships.
Lovette Oji indicated no relevant financial relationships.
Evelyn Calderon indicated no relevant financial relationships.
Oyindamola Amosu indicated no relevant financial relationships.
Christina Tache indicated no relevant financial relationships.
Eshan Nanda indicated no relevant financial relationships.
Anas Atrash indicated no relevant financial relationships.
Raul Cantu indicated no relevant financial relationships.
Hajra Khan indicated no relevant financial relationships.
Angsupat Pornchai, MD, Lovette Oji, MD, Evelyn Calderon, MD, Oyindamola Amosu, MD, Christina Tache, MD, Eshan Nanda, MD, Anas Atrash, MD, Raul Cantu, MD, Hajra Khan, MD. P4368 - Age ≥60 Years Predicts Higher In-Hospital Mortality in Acute Pancreatitis: A 2022 Central Pennsylvania Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Pittsburgh Medical Center, Harrisburg, PA
Introduction: Acute pancreatitis (AP) is an acute inflammatory disorder of the pancreas and a major contributor to gastrointestinal-related hospitalizations globally, with substantial clinical and economic consequences. While the majority of cases resolve with mild disease, up to 20% progress to severe AP, marked by increased morbidity, mortality, and resource use, particularly in high-risk subgroups. As the population ages, older patients are experiencing a rising incidence of AP and disproportionately suffer severe complications and death. However, the influence of advanced age on in-hospital outcomes including in-hospital mortality, need for intensive care, and length of stay has not been clearly defined, and prior reports lack consistent, age-stratified data. Recognizing the unique vulnerabilities of elderly patients, our study aims to fill this gap by rigorously analyzing the relationship between age and in-hospital outcomes in AP.
Methods: We retrospectively reviewed 287 consecutive adults (≥18 years) admitted with serologically and radiographically confirmed acute pancreatitis to a Central Pennsylvania hospital in 2022. Exclusion criteria included age < 18 years, acute-on-chronic pancreatitis, incomplete demographic data, or absence of confirmatory laboratory or imaging studies. Patients were stratified into elderly (≥60 years; n = 105) and non-elderly (< 60 years; n = 182) cohorts. The primary endpoint was in-hospital mortality; secondary endpoints were intensive care unit admission and hospital length of stay (LOS). Continuous variables were assessed for normality using the Shapiro–Wilk test: normally distributed data are reported as mean ± SD (range), and non-normal data as median (interquartile range). Between-group comparisons used Student’s t-test or the Mann–Whitney U test for continuous variables, and chi-square or Fisher’s exact test for categorical variables. A two-sided P < 0.05 was considered statistically significant. All analyses were performed with SAS 9.4.
Results: Elderly patients had higher in-hospital mortality than non-elderly patients (12.4% vs 2.2%; p = 0.0004). ICU admission rates were similar (8.6% vs 6.1%; p = 0.43). Median LOS was 3 days (IQR 2–5) in elderly and 3 days (IQR 2–4) in non-elderly patients (p = 0.09).
Discussion: Elderly AP patients exhibit distinct demographic characteristics, including greater White race representation, higher partnership rates, and increased inpatient care, underscoring the need to tailor outreach and support interventions by age.
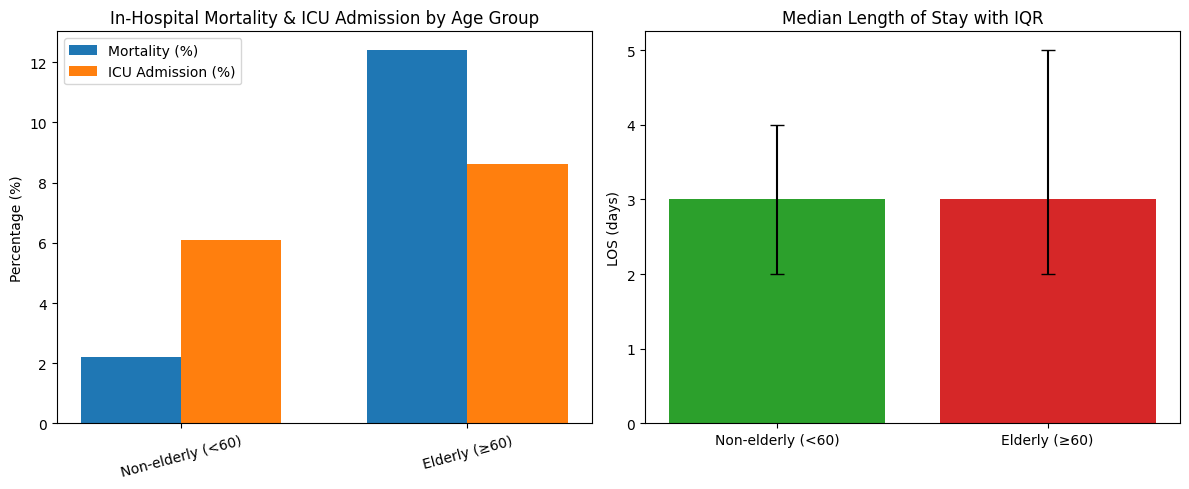
Figure: Panel 1: Bar chart showing in-hospital mortality and ICU admission rates (%)
Panel 2: Bar chart of median length-of-stay (days) with IQR error bars
Disclosures:
Angsupat Pornchai indicated no relevant financial relationships.
Lovette Oji indicated no relevant financial relationships.
Evelyn Calderon indicated no relevant financial relationships.
Oyindamola Amosu indicated no relevant financial relationships.
Christina Tache indicated no relevant financial relationships.
Eshan Nanda indicated no relevant financial relationships.
Anas Atrash indicated no relevant financial relationships.
Raul Cantu indicated no relevant financial relationships.
Hajra Khan indicated no relevant financial relationships.
Angsupat Pornchai, MD, Lovette Oji, MD, Evelyn Calderon, MD, Oyindamola Amosu, MD, Christina Tache, MD, Eshan Nanda, MD, Anas Atrash, MD, Raul Cantu, MD, Hajra Khan, MD. P4368 - Age ≥60 Years Predicts Higher In-Hospital Mortality in Acute Pancreatitis: A 2022 Central Pennsylvania Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
