Tuesday Poster Session
Category: Biliary/Pancreas
P4367 - Comparative Evaluation of Standard Diagnostics, Next-Generation Sequencing, and Deep Learning MRI for Pancreatic Cyst Classification and Risk Assessment
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hidayet Yilmaz, BSc (he/him/his)
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Award: ACG Presidential Poster Award
Hidayet Yilmaz, BSc, Michael B. Wallace, MD
Mayo Clinic, Jacksonville, FL
Introduction: Pancreatic cysts represent a diagnostic challenge due to their variable malignant potential. Classifying cysts as mucinous or non-mucinous and assessing their malignant transformation risk is vital for management. While standard diagnostics include invasive cytology and serial MRI imaging, novel methods such as next-generation sequencing (NGS) and deep-learning AI models have shown promise. This study compares performance of cytology, NGS, traditional MRI, and a deep-learning AI classification model.
Methods: We retrospectively analyzed 175 Mayo Clinic patients with pancreatic cysts. Data on MRI, FNA cytology, pathology and NGS was collected and used to classify cysts as mucinous or non-mucinous and estimate the malignant transformation potential. We evaluated the diagnostic performance of cytology, traditional MRI, NGS, and CEA through pairwise comparisons to pathology, PPC (pathology, NGS, and cytology composite variable), and one another. Once results are obtained, performance of a novel state-of-the-art AI deep-learning model compared to PPC will be analyzed.
Results: Traditional MRI demonstrated high sensitivity (95%) for cyst classification but low specificity (25%) and negative predictive value (44%), underlining its unreliability as a screening modality. NGS performs well against surgical pathology, with sensitivity of 85%, specificity of 75%, and PPV of 94%, in line with previously published results and outperforming current published surgical criteria. Cytology performed relatively poorly, with a sensitivity of 70% underlining its limited value as a standalone diagnostic tool. Compared to NGS, cyst fluid CEA showed sensitivity of 63% and specificity of 68%, reaffirming existing literature questioning its role in cyst classification.
Discussion: NGS demonstrates strong diagnostic accuracy and may be a valuable auxiliary tool in cyst evaluation and guiding treatment decisions. MRI remains sensitive but lacks specificity, while cytology and CEA are unreliable as standalone diagnostic tools. Our findings support a multimodal approach and suggest the addition of NGS into clinical workflows. Integration of a state-of-the-art AI-based MRI model for cyst classification is underway, and subsequent results of a comparison to a compound variable of pathology, NGS and cytology will follow. This study is the first to directly compare traditional diagnostics, NGS, and AI in pancreatic cysts, aiming to improve accuracy while reducing invasiveness.
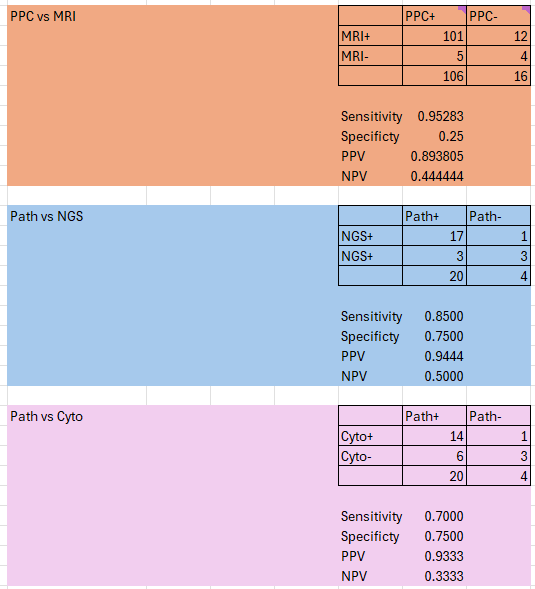
Figure: This table shows the performance of CEA vs Next-generation sequencing for cyst classification (mucinous or non-mucinous) and NGS performance compared to pathology for risk stratification (high-risk or low-risk of malignant transformation).
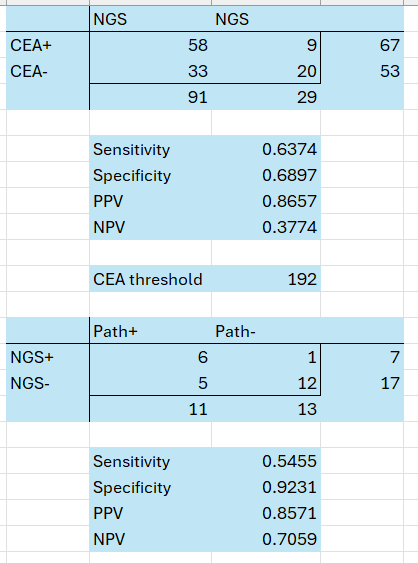
Figure: This table shows the performance in classifying cysts as either mucinous or non-mucinous
PPC = compound variable of pathology, next-generation sequencing and cytology
MRI = traditional MRI (no deep-learning model)
Disclosures:
Hidayet Yilmaz indicated no relevant financial relationships.
Michael Wallace indicated no relevant financial relationships.
Hidayet Yilmaz, BSc, Michael B. Wallace, MD. P4367 - Comparative Evaluation of Standard Diagnostics, Next-Generation Sequencing, and Deep Learning MRI for Pancreatic Cyst Classification and Risk Assessment, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Hidayet Yilmaz, BSc, Michael B. Wallace, MD
Mayo Clinic, Jacksonville, FL
Introduction: Pancreatic cysts represent a diagnostic challenge due to their variable malignant potential. Classifying cysts as mucinous or non-mucinous and assessing their malignant transformation risk is vital for management. While standard diagnostics include invasive cytology and serial MRI imaging, novel methods such as next-generation sequencing (NGS) and deep-learning AI models have shown promise. This study compares performance of cytology, NGS, traditional MRI, and a deep-learning AI classification model.
Methods: We retrospectively analyzed 175 Mayo Clinic patients with pancreatic cysts. Data on MRI, FNA cytology, pathology and NGS was collected and used to classify cysts as mucinous or non-mucinous and estimate the malignant transformation potential. We evaluated the diagnostic performance of cytology, traditional MRI, NGS, and CEA through pairwise comparisons to pathology, PPC (pathology, NGS, and cytology composite variable), and one another. Once results are obtained, performance of a novel state-of-the-art AI deep-learning model compared to PPC will be analyzed.
Results: Traditional MRI demonstrated high sensitivity (95%) for cyst classification but low specificity (25%) and negative predictive value (44%), underlining its unreliability as a screening modality. NGS performs well against surgical pathology, with sensitivity of 85%, specificity of 75%, and PPV of 94%, in line with previously published results and outperforming current published surgical criteria. Cytology performed relatively poorly, with a sensitivity of 70% underlining its limited value as a standalone diagnostic tool. Compared to NGS, cyst fluid CEA showed sensitivity of 63% and specificity of 68%, reaffirming existing literature questioning its role in cyst classification.
Discussion: NGS demonstrates strong diagnostic accuracy and may be a valuable auxiliary tool in cyst evaluation and guiding treatment decisions. MRI remains sensitive but lacks specificity, while cytology and CEA are unreliable as standalone diagnostic tools. Our findings support a multimodal approach and suggest the addition of NGS into clinical workflows. Integration of a state-of-the-art AI-based MRI model for cyst classification is underway, and subsequent results of a comparison to a compound variable of pathology, NGS and cytology will follow. This study is the first to directly compare traditional diagnostics, NGS, and AI in pancreatic cysts, aiming to improve accuracy while reducing invasiveness.
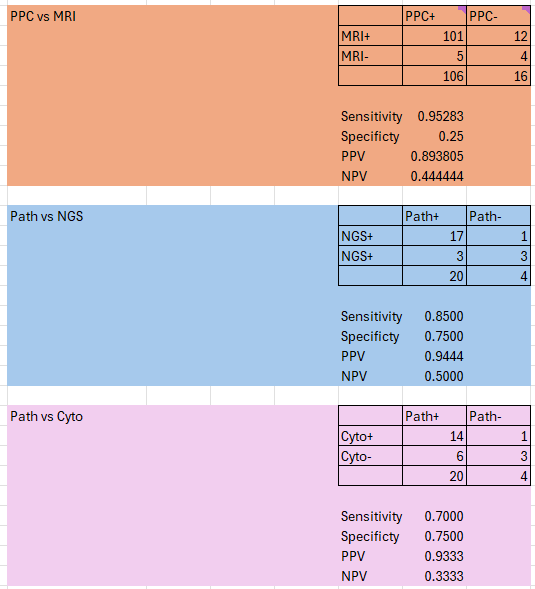
Figure: This table shows the performance of CEA vs Next-generation sequencing for cyst classification (mucinous or non-mucinous) and NGS performance compared to pathology for risk stratification (high-risk or low-risk of malignant transformation).
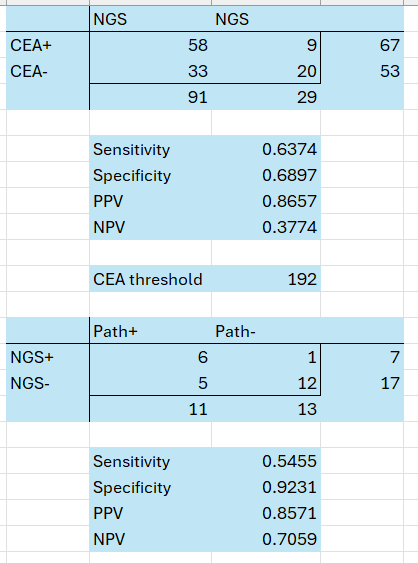
Figure: This table shows the performance in classifying cysts as either mucinous or non-mucinous
PPC = compound variable of pathology, next-generation sequencing and cytology
MRI = traditional MRI (no deep-learning model)
Disclosures:
Hidayet Yilmaz indicated no relevant financial relationships.
Michael Wallace indicated no relevant financial relationships.
Hidayet Yilmaz, BSc, Michael B. Wallace, MD. P4367 - Comparative Evaluation of Standard Diagnostics, Next-Generation Sequencing, and Deep Learning MRI for Pancreatic Cyst Classification and Risk Assessment, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

