Tuesday Poster Session
Category: Biliary/Pancreas
P4364 - Endoscopic Stenting for Pancreatic Duct Strictures in Chronic Pancreatitis: Long-Term Pain Relief Outcomes
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Omar Shamaa, MD
Henry Ford Health
Detroit, MI
Presenting Author(s)
Omar Shamaa, MD1, Maria Chavarria-Viales, 1, Bradley Karmo, MD2, Attisha Tyler, MD3, Faisal Nimri, MD4, Mazen Elatrache, MD1, Tobias Zuchelli, 4
1Henry Ford Health, Detroit, MI; 2Henry Ford Health, West Bloomfield, MI; 3Henry Ford Health System, Detroit, MI; 4Henry Ford Hospital, Detroit, MI
Introduction: Chronic pancreatitis (CP) is a progressive inflammatory disease that can result in chronic debilitating pain and eventual exocrine and endocrine insufficiency. Endoscopic therapies are frequently employed for the management of pancreatic duct (PD) strictures, however data on long-term efficacy for pain control remain limited. Our study aims to evaluate the long-term effectiveness of PD stricture stenting for pain relief in CP.
Methods: This is a single-center retrospective study, that included CP patients who underwent endoscopic retrograde cholangiopancreatography (ERCP), between 7/2014-7/2024. The primary outcome was clinical success following PD stricture stenting, defined as: immediate (pain improvement after 1 session), delayed (pain improvement after ≥2 sessions) and/or sustained (pain improvement for ≥1 year).
Results: Among a total of 123 patients with CP who underwent endoscopic therapy, PD strictures were found in 46% (n=57). All patients with PD strictures underwent PD stenting +/- balloon dilation. Following the initial PD stenting session, 47% reported immediate symptom improvement, while the remainder (53%) needed ≥2 stenting sessions for pain relief. Sustained pain improvement for ≥ 1 year was observed in 44%, and durable symptom relief during last clinical follow up was achieved in 37% of our CP patients with PD strictures. On average, 4 ERCPs with PD stenting were needed to achieve this long-term symptom relief, over a mean follow up period of 36.3 months. The longest stent free interval recorded was 16 months (IQR; 0, 58). Adjunct endoscopic therapies included extracorporeal shock wave lithotripsy (10.5%), spyglass-assisted electrohydraulic lithotripsy (7%), endoscopic ultrasound guided cystgastrostomy (5.3%) and necrosectomy (3.5%). There were no statistically significant associations between these additional endoscopic interventions and clinical success rates.
Discussion: This study highlights the complexity of managing CP pain with endoscopic therapies alone. PD stenting provided long-term symptom relief in only about one-third of patients, primarily after multiple stenting sessions. Those repeat endoscopic therapies can carry increased procedural and anesthesia related adverse events, elevated patient costs and a substantial burden on healthcare systems. Our findings emphasize the need for more effective, tailored interventions to achieve durable pain control in CP while minimizing the cumulative risks and resource demands of current approaches.
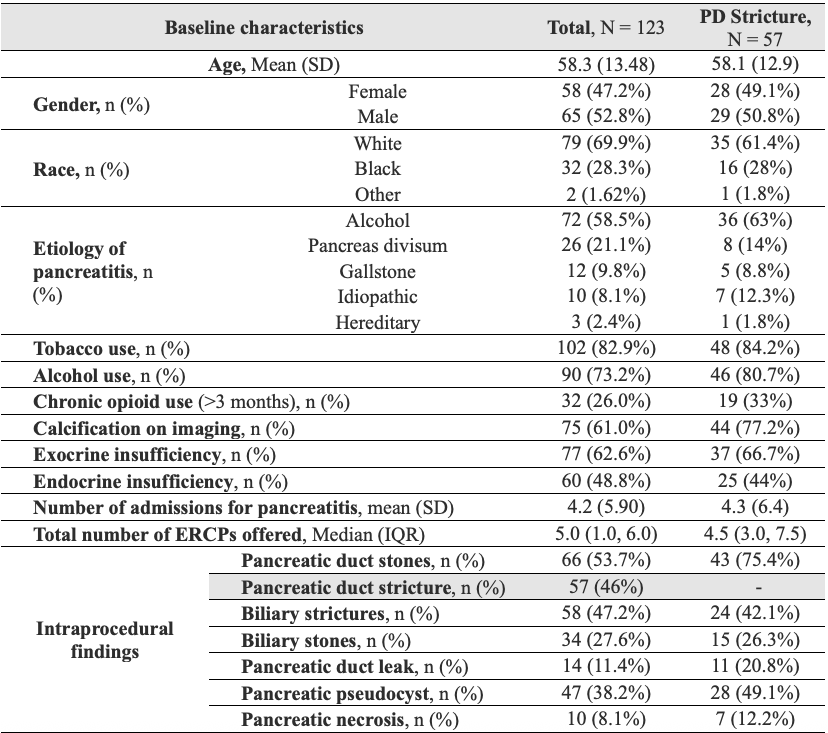
Figure: Table 1. Patient characteristics and intraprocedural details
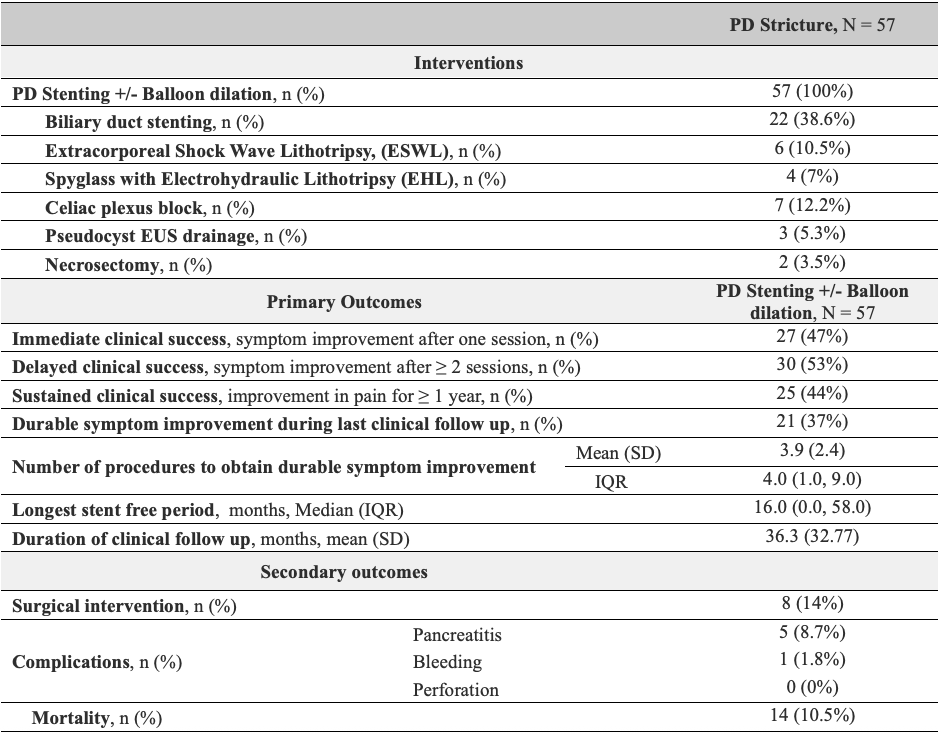
Figure: Table 2. Pancreatic duct stricture Interventions and treatment outcomes
Disclosures:
Omar Shamaa indicated no relevant financial relationships.
Maria Chavarria-Viales indicated no relevant financial relationships.
Bradley Karmo indicated no relevant financial relationships.
Attisha Tyler indicated no relevant financial relationships.
Faisal Nimri indicated no relevant financial relationships.
Mazen Elatrache indicated no relevant financial relationships.
Tobias Zuchelli: Boston Scientific – Consultant.
Omar Shamaa, MD1, Maria Chavarria-Viales, 1, Bradley Karmo, MD2, Attisha Tyler, MD3, Faisal Nimri, MD4, Mazen Elatrache, MD1, Tobias Zuchelli, 4. P4364 - Endoscopic Stenting for Pancreatic Duct Strictures in Chronic Pancreatitis: Long-Term Pain Relief Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Henry Ford Health, Detroit, MI; 2Henry Ford Health, West Bloomfield, MI; 3Henry Ford Health System, Detroit, MI; 4Henry Ford Hospital, Detroit, MI
Introduction: Chronic pancreatitis (CP) is a progressive inflammatory disease that can result in chronic debilitating pain and eventual exocrine and endocrine insufficiency. Endoscopic therapies are frequently employed for the management of pancreatic duct (PD) strictures, however data on long-term efficacy for pain control remain limited. Our study aims to evaluate the long-term effectiveness of PD stricture stenting for pain relief in CP.
Methods: This is a single-center retrospective study, that included CP patients who underwent endoscopic retrograde cholangiopancreatography (ERCP), between 7/2014-7/2024. The primary outcome was clinical success following PD stricture stenting, defined as: immediate (pain improvement after 1 session), delayed (pain improvement after ≥2 sessions) and/or sustained (pain improvement for ≥1 year).
Results: Among a total of 123 patients with CP who underwent endoscopic therapy, PD strictures were found in 46% (n=57). All patients with PD strictures underwent PD stenting +/- balloon dilation. Following the initial PD stenting session, 47% reported immediate symptom improvement, while the remainder (53%) needed ≥2 stenting sessions for pain relief. Sustained pain improvement for ≥ 1 year was observed in 44%, and durable symptom relief during last clinical follow up was achieved in 37% of our CP patients with PD strictures. On average, 4 ERCPs with PD stenting were needed to achieve this long-term symptom relief, over a mean follow up period of 36.3 months. The longest stent free interval recorded was 16 months (IQR; 0, 58). Adjunct endoscopic therapies included extracorporeal shock wave lithotripsy (10.5%), spyglass-assisted electrohydraulic lithotripsy (7%), endoscopic ultrasound guided cystgastrostomy (5.3%) and necrosectomy (3.5%). There were no statistically significant associations between these additional endoscopic interventions and clinical success rates.
Discussion: This study highlights the complexity of managing CP pain with endoscopic therapies alone. PD stenting provided long-term symptom relief in only about one-third of patients, primarily after multiple stenting sessions. Those repeat endoscopic therapies can carry increased procedural and anesthesia related adverse events, elevated patient costs and a substantial burden on healthcare systems. Our findings emphasize the need for more effective, tailored interventions to achieve durable pain control in CP while minimizing the cumulative risks and resource demands of current approaches.
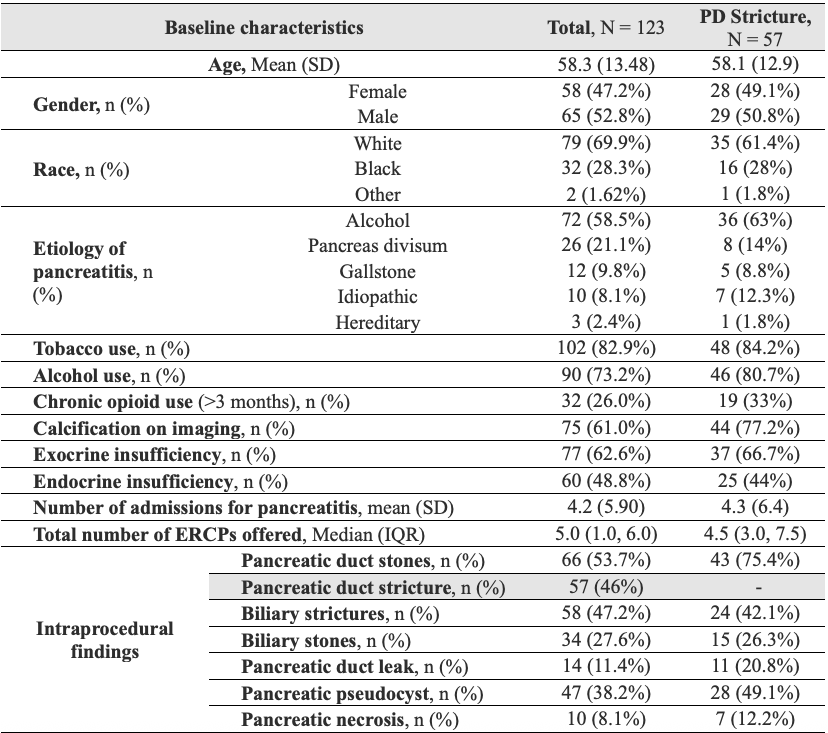
Figure: Table 1. Patient characteristics and intraprocedural details
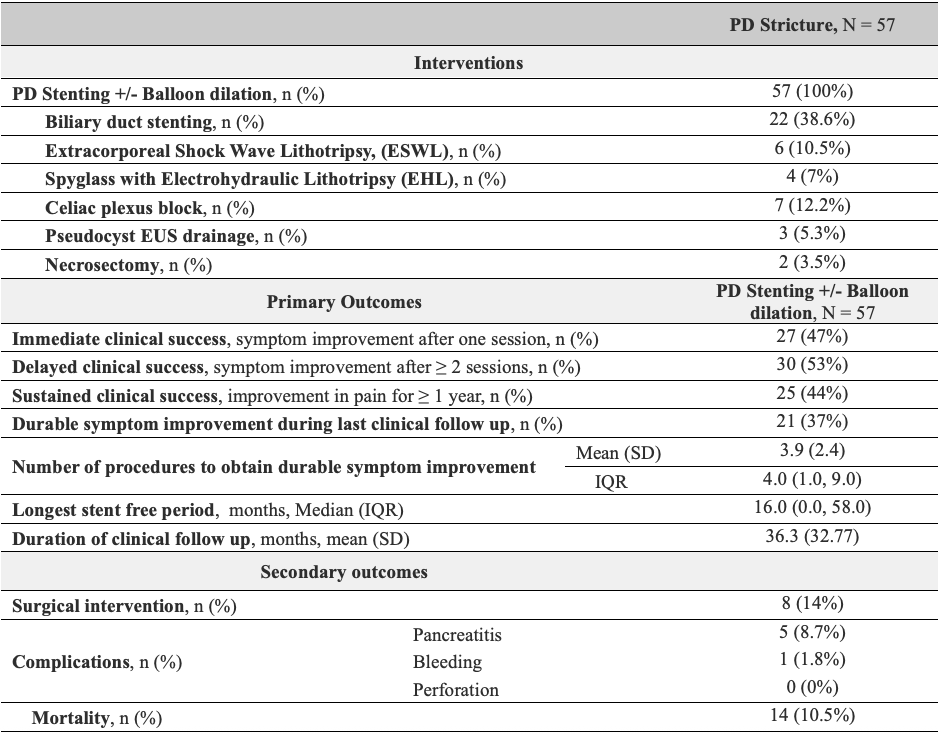
Figure: Table 2. Pancreatic duct stricture Interventions and treatment outcomes
Disclosures:
Omar Shamaa indicated no relevant financial relationships.
Maria Chavarria-Viales indicated no relevant financial relationships.
Bradley Karmo indicated no relevant financial relationships.
Attisha Tyler indicated no relevant financial relationships.
Faisal Nimri indicated no relevant financial relationships.
Mazen Elatrache indicated no relevant financial relationships.
Tobias Zuchelli: Boston Scientific – Consultant.
Omar Shamaa, MD1, Maria Chavarria-Viales, 1, Bradley Karmo, MD2, Attisha Tyler, MD3, Faisal Nimri, MD4, Mazen Elatrache, MD1, Tobias Zuchelli, 4. P4364 - Endoscopic Stenting for Pancreatic Duct Strictures in Chronic Pancreatitis: Long-Term Pain Relief Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
