Tuesday Poster Session
Category: Biliary/Pancreas
P4338 - AI-Based Survival Prediction in Primary Biliary Cirrhosis Using Random Survival Forest and Longitudinal Clinical Features
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sri Harsha Boppana, MBBS, MD
Nassau University Medical Center
Hicksville, NY
Presenting Author(s)
Sri Harsha Boppana, MBBS, MD1, Manaswitha Thota, MD2, Gautam Maddineni, MD3, Sachin Sravan Kumar Komati, 4, Sarath Chandra Ponnada, 5, Sai Lakshmi Prasanna Komati, MBBS6, C. David Mintz, MD, PhD7
1Nassau University Medical Center, East Meadow, NY; 2Virginia Commonwealth University, Richmond, VA; 3Florida State University, Cape Coral, FL; 4Florida International University, Florida, FL; 5Great Eastern Medical School and Hospital, Srikakulam, Srikakulam, Andhra Pradesh, India; 6Government Medical College, Ongole, Ongole, Andhra Pradesh, India; 7Johns Hopkins University School of Medicine, Baltimore, MD
Introduction: Primary biliary cirrhosis progresses unpredictably and challenges timely intervention. We developed and validated a random survival forest model to predict transplant-free survival and to identify key prognostic markers in a cohort of 418 patients.
Methods: We curated a cohort of 418 patients with primary biliary cirrhosis and collected longitudinal data on bilirubin, albumin, copper, prothrombin time, and 13 additional clinical variables. Missing continuous values received mean imputation; missing categorical values received mode imputation. We standardized continuous features to a mean of zero with unit variance and converted categorical variables into binary indicators. Outcomes were defined as death, liver transplantation, or censoring. We randomly allocated 80 percent of the data to a training set and 20 percent to a test set. We then trained a Random Survival Forest with 1,000 decision trees and assessed discrimination via the concordance index (C-index). To identify key prognostic markers, we performed permutation-based feature importance analysis.
Results: The Random Survival Forest achieved a training C-index of 0.94 and a testing C-index of 0.88. Permutation analysis highlighted baseline bilirubin and albumin as the most influential predictors, followed by prothrombin time and copper. We generated individualized risk scores and stratified patients into low- (n = 82), moderate- (n = 134), and high-risk (n = 202) groups. Mean risk scores measured 20.1 in the low-risk group, 31.8 in the moderate-risk group, and 93.9 in the high-risk group. Kaplan–Meier curves demonstrated clear separation across all three strata, confirming robust prognostic stratification. (Figure 1,2,3)
Discussion: The model demonstrated high discrimination and successfully stratified patients into distinct risk groups, with bilirubin and albumin emerging as dominant predictors. These results highlight the potential of machine-learning–based risk tools to inform personalized management and warrant external validation for broader clinical application.
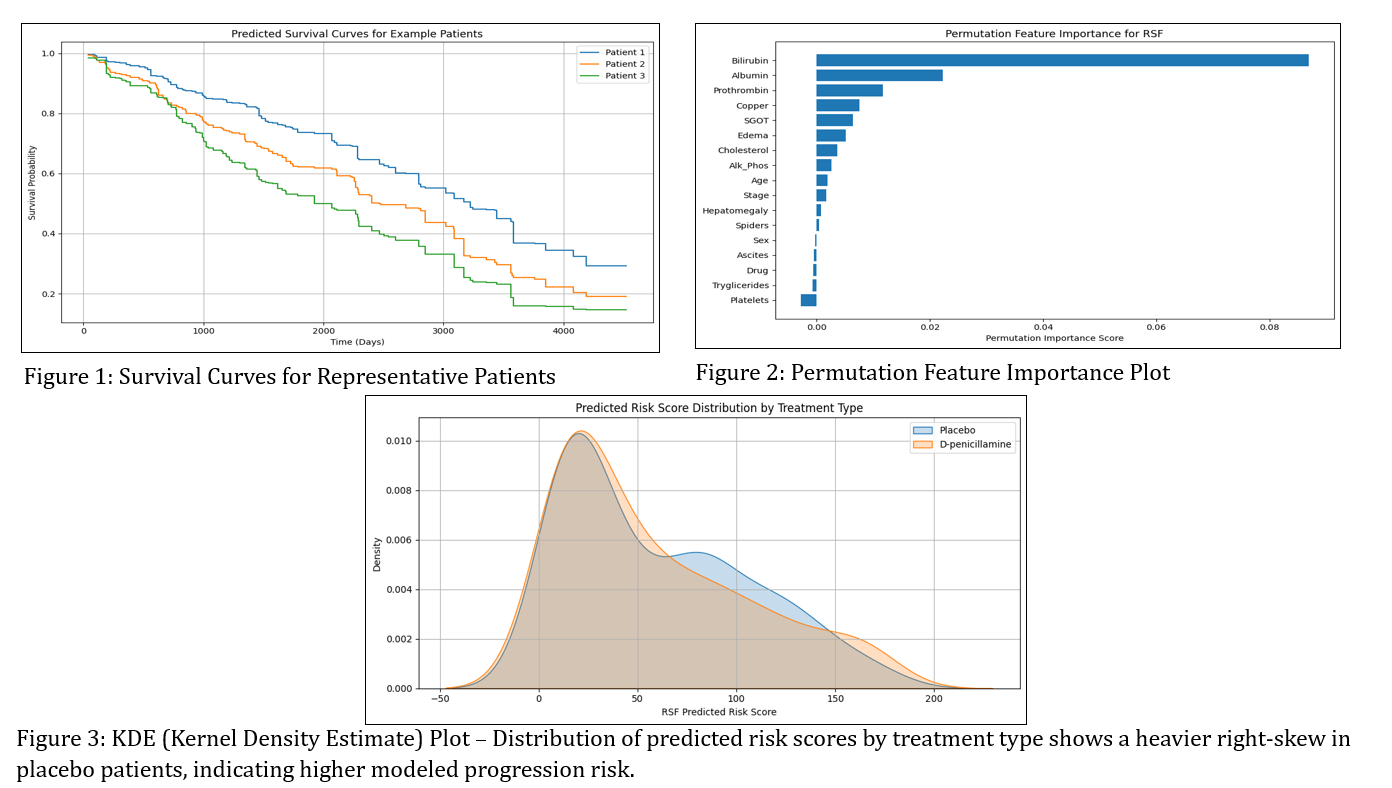
Figure: Figure 1,2,3
Disclosures:
Sri Harsha Boppana indicated no relevant financial relationships.
Manaswitha Thota indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Sachin Sravan Kumar Komati indicated no relevant financial relationships.
Sarath Chandra Ponnada indicated no relevant financial relationships.
Sai Lakshmi Prasanna Komati indicated no relevant financial relationships.
C. David Mintz indicated no relevant financial relationships.
Sri Harsha Boppana, MBBS, MD1, Manaswitha Thota, MD2, Gautam Maddineni, MD3, Sachin Sravan Kumar Komati, 4, Sarath Chandra Ponnada, 5, Sai Lakshmi Prasanna Komati, MBBS6, C. David Mintz, MD, PhD7. P4338 - AI-Based Survival Prediction in Primary Biliary Cirrhosis Using Random Survival Forest and Longitudinal Clinical Features, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Nassau University Medical Center, East Meadow, NY; 2Virginia Commonwealth University, Richmond, VA; 3Florida State University, Cape Coral, FL; 4Florida International University, Florida, FL; 5Great Eastern Medical School and Hospital, Srikakulam, Srikakulam, Andhra Pradesh, India; 6Government Medical College, Ongole, Ongole, Andhra Pradesh, India; 7Johns Hopkins University School of Medicine, Baltimore, MD
Introduction: Primary biliary cirrhosis progresses unpredictably and challenges timely intervention. We developed and validated a random survival forest model to predict transplant-free survival and to identify key prognostic markers in a cohort of 418 patients.
Methods: We curated a cohort of 418 patients with primary biliary cirrhosis and collected longitudinal data on bilirubin, albumin, copper, prothrombin time, and 13 additional clinical variables. Missing continuous values received mean imputation; missing categorical values received mode imputation. We standardized continuous features to a mean of zero with unit variance and converted categorical variables into binary indicators. Outcomes were defined as death, liver transplantation, or censoring. We randomly allocated 80 percent of the data to a training set and 20 percent to a test set. We then trained a Random Survival Forest with 1,000 decision trees and assessed discrimination via the concordance index (C-index). To identify key prognostic markers, we performed permutation-based feature importance analysis.
Results: The Random Survival Forest achieved a training C-index of 0.94 and a testing C-index of 0.88. Permutation analysis highlighted baseline bilirubin and albumin as the most influential predictors, followed by prothrombin time and copper. We generated individualized risk scores and stratified patients into low- (n = 82), moderate- (n = 134), and high-risk (n = 202) groups. Mean risk scores measured 20.1 in the low-risk group, 31.8 in the moderate-risk group, and 93.9 in the high-risk group. Kaplan–Meier curves demonstrated clear separation across all three strata, confirming robust prognostic stratification. (Figure 1,2,3)
Discussion: The model demonstrated high discrimination and successfully stratified patients into distinct risk groups, with bilirubin and albumin emerging as dominant predictors. These results highlight the potential of machine-learning–based risk tools to inform personalized management and warrant external validation for broader clinical application.
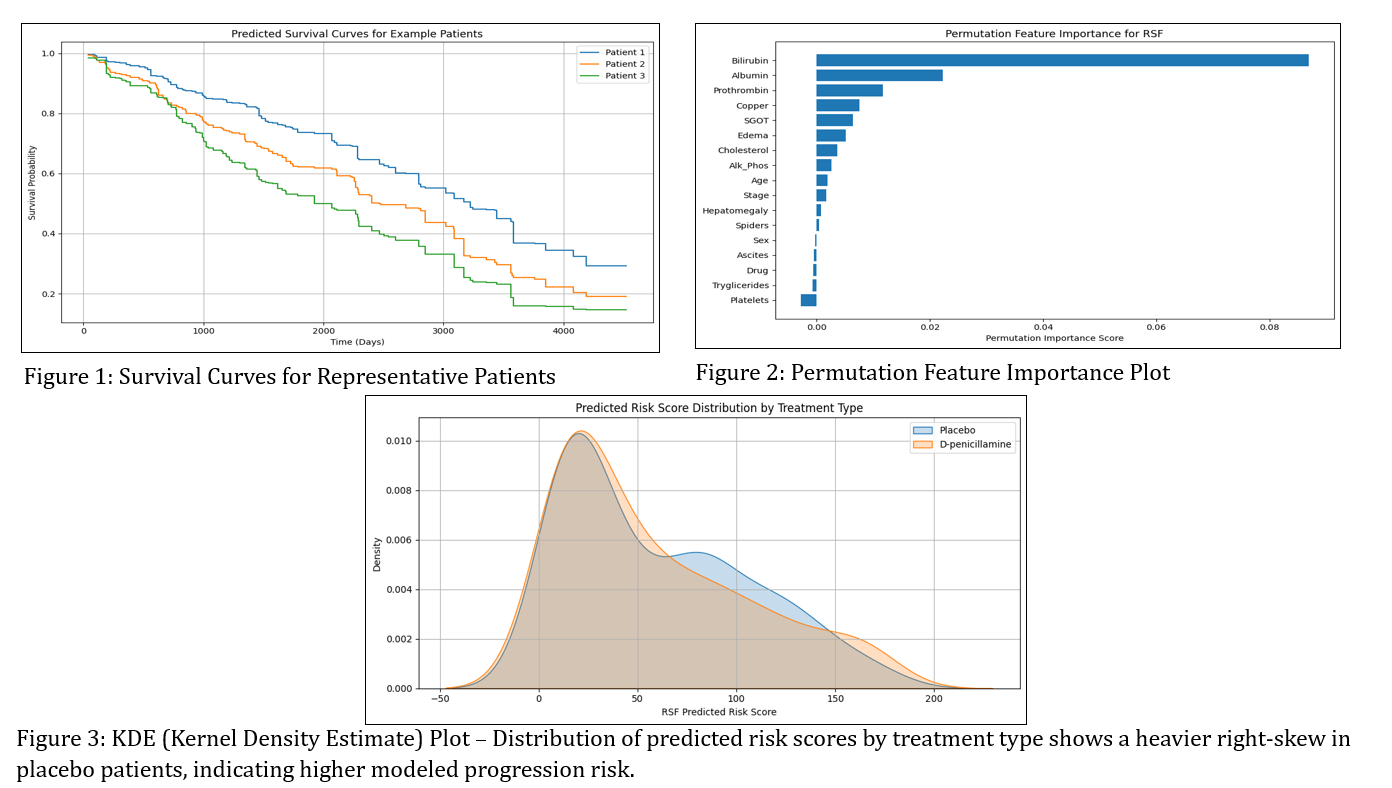
Figure: Figure 1,2,3
Disclosures:
Sri Harsha Boppana indicated no relevant financial relationships.
Manaswitha Thota indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Sachin Sravan Kumar Komati indicated no relevant financial relationships.
Sarath Chandra Ponnada indicated no relevant financial relationships.
Sai Lakshmi Prasanna Komati indicated no relevant financial relationships.
C. David Mintz indicated no relevant financial relationships.
Sri Harsha Boppana, MBBS, MD1, Manaswitha Thota, MD2, Gautam Maddineni, MD3, Sachin Sravan Kumar Komati, 4, Sarath Chandra Ponnada, 5, Sai Lakshmi Prasanna Komati, MBBS6, C. David Mintz, MD, PhD7. P4338 - AI-Based Survival Prediction in Primary Biliary Cirrhosis Using Random Survival Forest and Longitudinal Clinical Features, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
