Tuesday Poster Session
Category: Biliary/Pancreas
P4330 - Endoscopic Ultrasound-Guided Biopsy of Mural Nodule in Patients With Intraductal Papillary Mucinous Neoplasm: A Viable Strategy to Guide Decision-Making?
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hoe Yan Hor, MBBS (he/him/his)
Mayo Clinic Arizona
Phoenix, AZ
Presenting Author(s)
Hoe Yan Hor, MBBS1, Melody Pi Yin Tu, MBBS2, Po Hong Tan, MBBS2, Richard M. Miller, BS3, Arshia Pessaran, BS2, Douglas Faigel, MD4, Michelle A.. Anderson, MD2, Norio Fukami, MD, FACG2, Michael B. Wallace, MD5, Santhi Swaroop Vege, MD, MACG6, Shounak Majumder, MD6, Chee-chee H. Stucky, MD2, Nabil Wasif, MD, MPH2, Rahul Pannala, MD2, Zhi Ven Fong, MD, MPH, DrPH2
1Mayo Clinic Arizona, Phoenix, AZ; 2Mayo Clinic, Phoenix, AZ; 3Creighton University School of Medicine, Phoenix, AZ; 4Mayo Clinic, Scottsdale, AZ; 5Mayo Clinic, Jacksonville, FL; 6Mayo Clinic, Rochester, MN
Introduction: Intraductal papillary mucinous neoplasm with mural nodules (IPMN-MNs) are associated with a 30% to 50% risk of harboring high-grade dysplasia/adenocarcinoma (HGD/Ca). There are limited data on the accuracy of endoscopic ultrasound guided aspiration/biopsy (EUS-FNA) to identify HGD/Ca and its impact on management. This study evaluated the congruency of EUS-FNA results with surgical pathology.
Methods: In a multi-center retrospective review, we identified patients with IPMN-MNs who underwent EUS-FNA between 2001 and 2024 (Figure 1). Patient demographics, disease characteristics, and treatment modalities were summarized. Univariate analysis was performed to assess factors associated with false-negative EUS-FNA results. Kaplan-Meier analysis was performed to compare survival outcomes in patients with HGD/Ca between treatment groups.
Results: We identified 239 patients; of whom majority (133, 56%) was male, with a median age of 74 (IQR 67-82). The median cyst size was 23 mm (IQR 16-33), and median mural nodule size was 8 mm (IQR 6-10) with a median follow-up of 4.4 years (IQR 1.7-8.5). Majority had branch duct IPMNs (161, 67%), followed by main duct IPMNs (42, 18%), and mixed-type IPMNs (36, 15%). Ninety-two (38%) underwent upfront resection, 30 (13%) underwent resection during surveillance, and 117 (49%) were managed with surveillance only. Among resected patients, the overall incidence of HGD/Ca on surgical pathology was 44%. Among 32 patients with an EUS-FNA result of HGD/Ca, 27 patients had a true-positive result (84% positive predictive value). Among 90 patients with EUS-FNA showing no HGD/Ca, 63 patients had a true-negative result (70% negative predictive value [NPV]). Factors associated with false-negative EUS-FNA results were main or mixed duct involvement, pancreatic ductal dilatation ≥7 mm, and cyst size ≥33 mm on EUS (p< 0.05). EUS-FNA had a sensitivity of 50% (CI: 37%-63%); specificity of 93% (CI: 84%-97%); positive likelihood ratio (LLR) of 6.8 (CI: 2.8-16.5) and negative LLR of 0.54 (CI: 0.4-0.7). Among patients with HGD/Ca on surgical pathology, overall survival was similar between patients managed with surveillance first before eventually undergoing resection and those who underwent upfront resection (p=0.77) (Figure 2).
Discussion: Among patients with IPMN-MN, 56% did not have HGD/Ca. Our study demonstrated that EUS-FNA of the mural nodule had a NPV of 70% and may prove as a reasonable risk-stratifying modality especially in higher-risk patients with competing comorbidities.
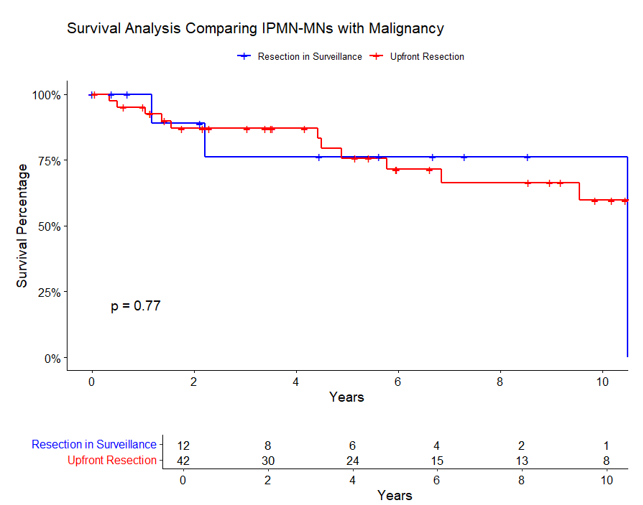
Figure: Figure 1: Endoscopic Ultrasound (EUS) Image of a Confirmed Mural Nodule in an IPMN.

Figure: Figure 2: Survival Curve of Patients with IPMN with mural nodule with HGD/Cancer — Upfront Resection at Mural Nodule Detection vs Resection During Surveillance.
Disclosures:
Hoe Yan Hor indicated no relevant financial relationships.
Melody Pi Yin Tu indicated no relevant financial relationships.
Po Hong Tan indicated no relevant financial relationships.
Richard Miller indicated no relevant financial relationships.
Arshia Pessaran indicated no relevant financial relationships.
Douglas Faigel indicated no relevant financial relationships.
Michelle Anderson: Boston Scientific – Consultant.
Norio Fukami: Boston Scientific – Consultant. Creo Medical – Consultant.
Michael Wallace indicated no relevant financial relationships.
Santhi Swaroop Vege: Barnes Jewish in Saint Louis – Consultant. Beth Israel Hospital Boston – Consultant. Department of Defense – Grant/Research Support. Houston Methodist – Consultant. NIDDK – Grant/Research Support. Orlando Health – Consultant. Up-to-Date – Royalties.
Shounak Majumder indicated no relevant financial relationships.
Chee-chee H. Stucky indicated no relevant financial relationships.
Nabil Wasif indicated no relevant financial relationships.
Rahul Pannala: HCL Technologies – Consultant. Nestlé Health Science – Consultant.
Zhi Ven Fong indicated no relevant financial relationships.
Hoe Yan Hor, MBBS1, Melody Pi Yin Tu, MBBS2, Po Hong Tan, MBBS2, Richard M. Miller, BS3, Arshia Pessaran, BS2, Douglas Faigel, MD4, Michelle A.. Anderson, MD2, Norio Fukami, MD, FACG2, Michael B. Wallace, MD5, Santhi Swaroop Vege, MD, MACG6, Shounak Majumder, MD6, Chee-chee H. Stucky, MD2, Nabil Wasif, MD, MPH2, Rahul Pannala, MD2, Zhi Ven Fong, MD, MPH, DrPH2. P4330 - Endoscopic Ultrasound-Guided Biopsy of Mural Nodule in Patients With Intraductal Papillary Mucinous Neoplasm: A Viable Strategy to Guide Decision-Making?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic Arizona, Phoenix, AZ; 2Mayo Clinic, Phoenix, AZ; 3Creighton University School of Medicine, Phoenix, AZ; 4Mayo Clinic, Scottsdale, AZ; 5Mayo Clinic, Jacksonville, FL; 6Mayo Clinic, Rochester, MN
Introduction: Intraductal papillary mucinous neoplasm with mural nodules (IPMN-MNs) are associated with a 30% to 50% risk of harboring high-grade dysplasia/adenocarcinoma (HGD/Ca). There are limited data on the accuracy of endoscopic ultrasound guided aspiration/biopsy (EUS-FNA) to identify HGD/Ca and its impact on management. This study evaluated the congruency of EUS-FNA results with surgical pathology.
Methods: In a multi-center retrospective review, we identified patients with IPMN-MNs who underwent EUS-FNA between 2001 and 2024 (Figure 1). Patient demographics, disease characteristics, and treatment modalities were summarized. Univariate analysis was performed to assess factors associated with false-negative EUS-FNA results. Kaplan-Meier analysis was performed to compare survival outcomes in patients with HGD/Ca between treatment groups.
Results: We identified 239 patients; of whom majority (133, 56%) was male, with a median age of 74 (IQR 67-82). The median cyst size was 23 mm (IQR 16-33), and median mural nodule size was 8 mm (IQR 6-10) with a median follow-up of 4.4 years (IQR 1.7-8.5). Majority had branch duct IPMNs (161, 67%), followed by main duct IPMNs (42, 18%), and mixed-type IPMNs (36, 15%). Ninety-two (38%) underwent upfront resection, 30 (13%) underwent resection during surveillance, and 117 (49%) were managed with surveillance only. Among resected patients, the overall incidence of HGD/Ca on surgical pathology was 44%. Among 32 patients with an EUS-FNA result of HGD/Ca, 27 patients had a true-positive result (84% positive predictive value). Among 90 patients with EUS-FNA showing no HGD/Ca, 63 patients had a true-negative result (70% negative predictive value [NPV]). Factors associated with false-negative EUS-FNA results were main or mixed duct involvement, pancreatic ductal dilatation ≥7 mm, and cyst size ≥33 mm on EUS (p< 0.05). EUS-FNA had a sensitivity of 50% (CI: 37%-63%); specificity of 93% (CI: 84%-97%); positive likelihood ratio (LLR) of 6.8 (CI: 2.8-16.5) and negative LLR of 0.54 (CI: 0.4-0.7). Among patients with HGD/Ca on surgical pathology, overall survival was similar between patients managed with surveillance first before eventually undergoing resection and those who underwent upfront resection (p=0.77) (Figure 2).
Discussion: Among patients with IPMN-MN, 56% did not have HGD/Ca. Our study demonstrated that EUS-FNA of the mural nodule had a NPV of 70% and may prove as a reasonable risk-stratifying modality especially in higher-risk patients with competing comorbidities.
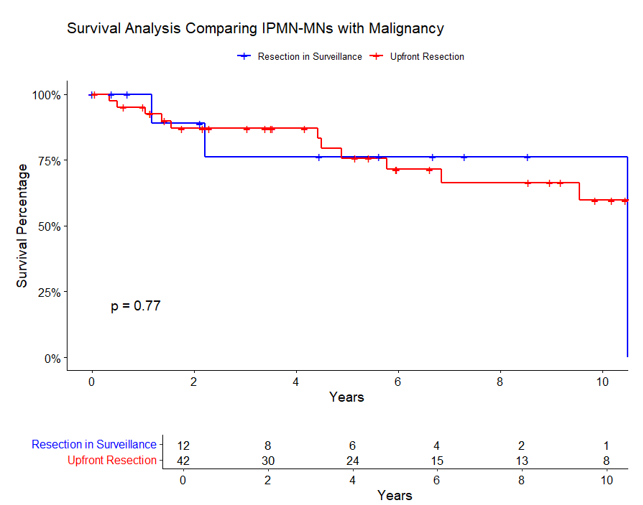
Figure: Figure 1: Endoscopic Ultrasound (EUS) Image of a Confirmed Mural Nodule in an IPMN.

Figure: Figure 2: Survival Curve of Patients with IPMN with mural nodule with HGD/Cancer — Upfront Resection at Mural Nodule Detection vs Resection During Surveillance.
Disclosures:
Hoe Yan Hor indicated no relevant financial relationships.
Melody Pi Yin Tu indicated no relevant financial relationships.
Po Hong Tan indicated no relevant financial relationships.
Richard Miller indicated no relevant financial relationships.
Arshia Pessaran indicated no relevant financial relationships.
Douglas Faigel indicated no relevant financial relationships.
Michelle Anderson: Boston Scientific – Consultant.
Norio Fukami: Boston Scientific – Consultant. Creo Medical – Consultant.
Michael Wallace indicated no relevant financial relationships.
Santhi Swaroop Vege: Barnes Jewish in Saint Louis – Consultant. Beth Israel Hospital Boston – Consultant. Department of Defense – Grant/Research Support. Houston Methodist – Consultant. NIDDK – Grant/Research Support. Orlando Health – Consultant. Up-to-Date – Royalties.
Shounak Majumder indicated no relevant financial relationships.
Chee-chee H. Stucky indicated no relevant financial relationships.
Nabil Wasif indicated no relevant financial relationships.
Rahul Pannala: HCL Technologies – Consultant. Nestlé Health Science – Consultant.
Zhi Ven Fong indicated no relevant financial relationships.
Hoe Yan Hor, MBBS1, Melody Pi Yin Tu, MBBS2, Po Hong Tan, MBBS2, Richard M. Miller, BS3, Arshia Pessaran, BS2, Douglas Faigel, MD4, Michelle A.. Anderson, MD2, Norio Fukami, MD, FACG2, Michael B. Wallace, MD5, Santhi Swaroop Vege, MD, MACG6, Shounak Majumder, MD6, Chee-chee H. Stucky, MD2, Nabil Wasif, MD, MPH2, Rahul Pannala, MD2, Zhi Ven Fong, MD, MPH, DrPH2. P4330 - Endoscopic Ultrasound-Guided Biopsy of Mural Nodule in Patients With Intraductal Papillary Mucinous Neoplasm: A Viable Strategy to Guide Decision-Making?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
