Tuesday Poster Session
Category: Biliary/Pancreas
P4326 - Is ERCP Helpful in Traumatic Bile Leaks?
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Varun Angajala, MS, MD (he/him/his)
Boston University
Boston, MA
Presenting Author(s)
Varun Angajala, MS, MD1, Jacqueline Liu, MD2, Christopher Huang, MD3
1Boston University, Boston, MA; 2Boston Medical Center, Boston, MA; 3Boston University Chobanian & Avedisian School of Medicine, Boston, MA
Introduction: Although endoscopic retrograde cholangiopancreatography (ERCP) is the standard of care for post-surgical bile duct leak (BDL), its role in BDL from hepatic trauma is under-studied. In post-cholecystectomy bile leaks, trans-papillary stenting (TPS) of the bile duct in addition to endoscopic sphincterotomy (ES) improves outcomes compared to ES alone, particularly in patients with major leaks. These endoscopic interventions eliminate the pressure gradient between the bile duct and the duodenum which leads to preferential flow of bile into the duodenum. TPS may have the added benefit of bypassing the cystic duct orifice. However, in traumatic BDL, the small caliber intrahepatic ducts which are disrupted may be less sensitive to the effects of endoscopic therapy. In particular, the role of TPS in traumatic BDL is called into question. We hypothesize that ERCP with ES alone in traumatic BDL is non-inferior to ERCP with ES + TPS.
Methods: In this single-institution retrospective cohort study, patients > 18yo who were diagnosed with BDL from hepatic trauma from 2014 to 2024 were reviewed. The primary outcome was time to perihepatic drain removal after ERCP with ES alone versus ES+TPS. The secondary outcomes were time to perihepatic drain removal after ERCP versus no ERCP and rate of follow-up after TPS placement. Statistical analyses were performed in Microsoft Excel. Paired 2-sided Fischer’s t-tests were used to evaluate primary and secondary outcomes. Multivariate logistic regression was used to account for type of endoscopic intervention, need for angioembolization, and liver injury grade as defined by American Association of Surgery of Trauma.
Results: Among 25 patients in the study cohort, 14 underwent ERCP with ES-only, 5 underwent ERCP with ES+TPS, and 6 did not undergo ERCP. One patient died within 48 hours of presentation and was excluded.
Mean time to drain removal was 11.4 days in the ES-only group vs. 28.8 days in the ES+TPS group (P = 0.017). In a multivariate logistic regression model, angioembolization (P = 0.032) and TPS placement (P=0.009) were associated with increased time to drain removal. Among patients who underwent TPS placement, 1 out of 5 was unable to follow up for stent removal due to difficulties with health insurance.
Discussion: In BDL from hepatic trauma, ERCP with ES alone may be non-inferior to ES+TPS and avoids the risk of loss of follow-up for TPS removal. Further study is needed to determine whether ERCP is truly beneficial in treating BDL from hepatic trauma.
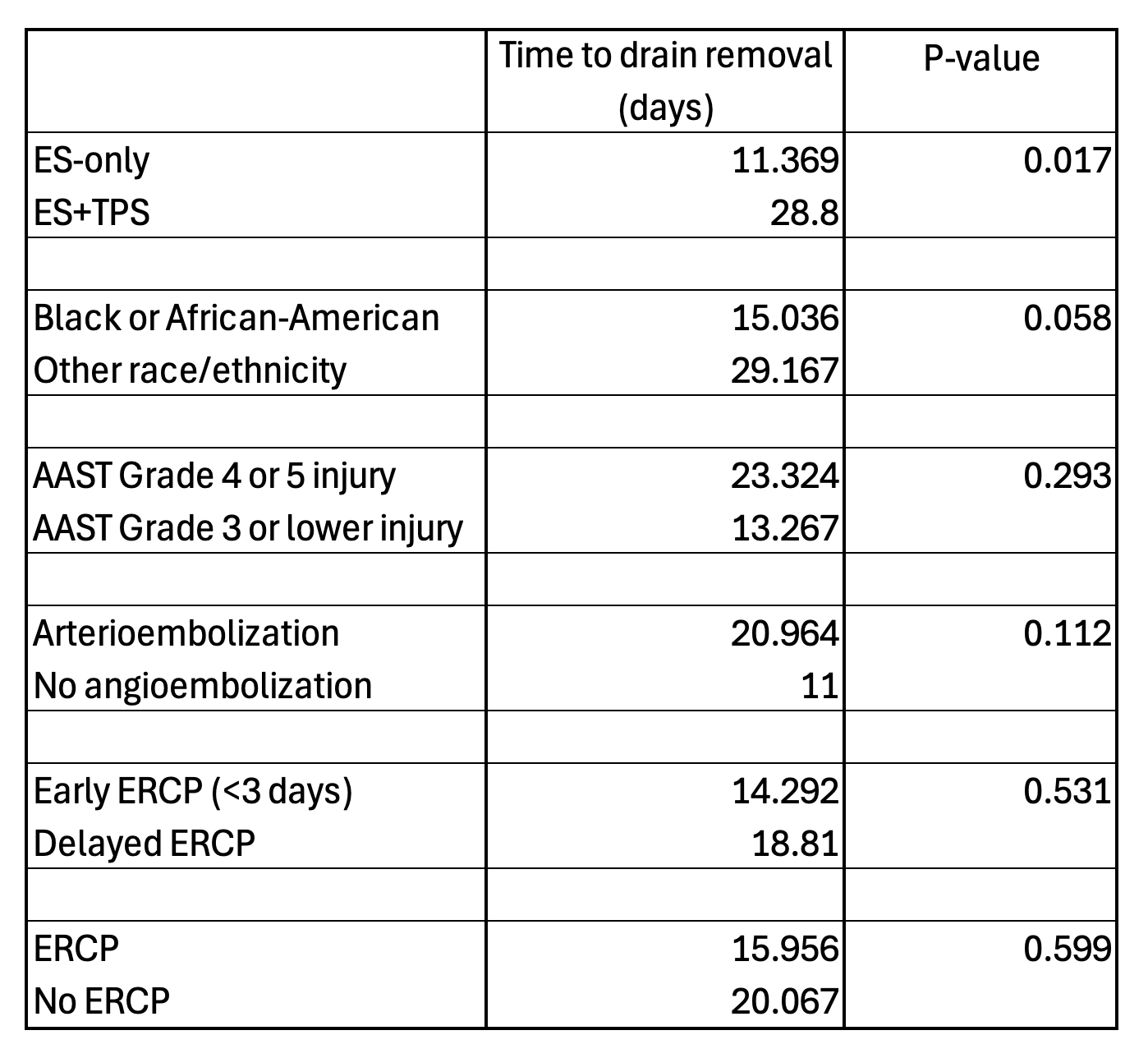
Figure: Table 1. Average time to drain removal and P-values of paired 2-sided t-tests, comparing the following elements: type of endoscopic intervention performed, race, liver injury grade as measured by American Association of Trauma Surgery (AAST) Liver Injury Scale, need for angioembolization, early vs. delayed ERCP, and ERCP vs. conservative management.
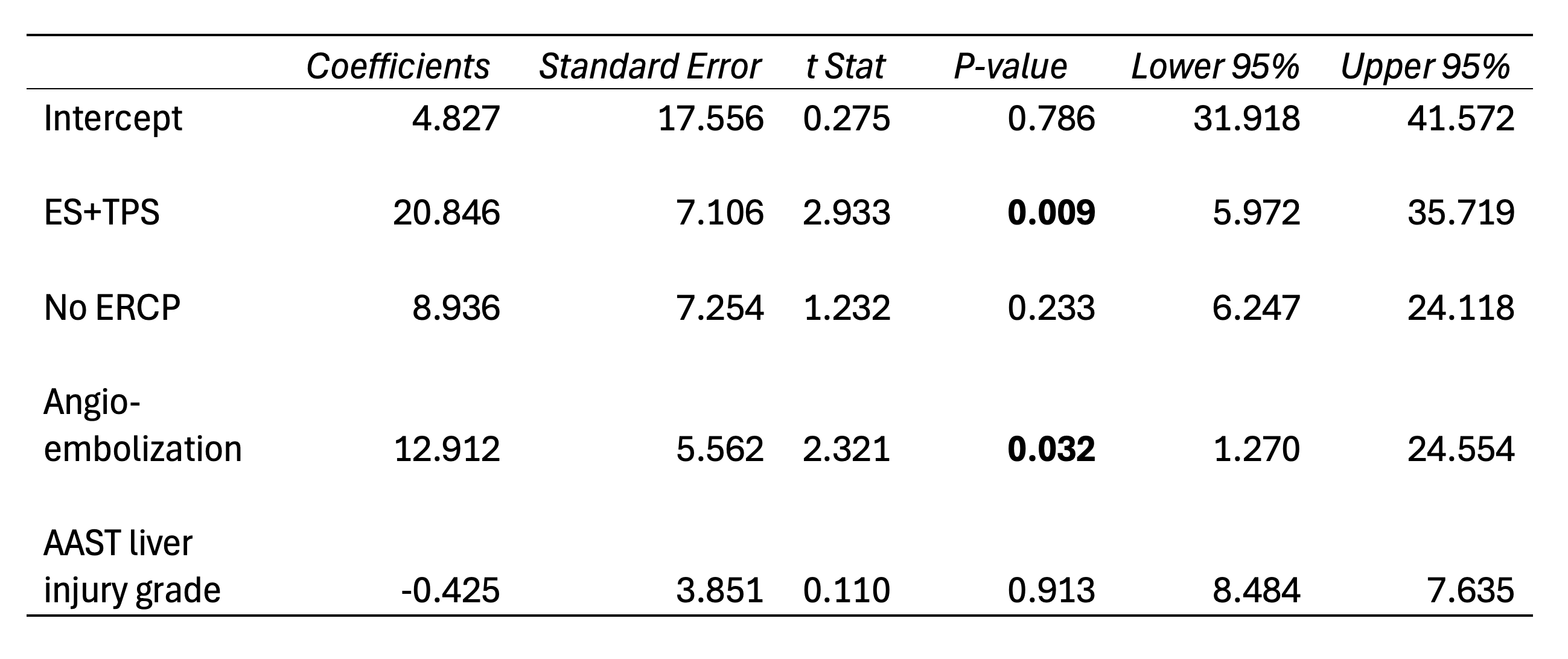
Figure: Table 2. Results of multivariate logistic regression model accounting for the following elements: type of endoscopic intervention performed, whether or not ERCP was performed, need for angioembolization, and liver injury grade as measured by American Association of Trauma Surgery (AAST) Livery Injury Scale.
Disclosures:
Varun Angajala indicated no relevant financial relationships.
Jacqueline Liu indicated no relevant financial relationships.
Christopher Huang: Olympus – Consultant.
Varun Angajala, MS, MD1, Jacqueline Liu, MD2, Christopher Huang, MD3. P4326 - Is ERCP Helpful in Traumatic Bile Leaks?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Boston University, Boston, MA; 2Boston Medical Center, Boston, MA; 3Boston University Chobanian & Avedisian School of Medicine, Boston, MA
Introduction: Although endoscopic retrograde cholangiopancreatography (ERCP) is the standard of care for post-surgical bile duct leak (BDL), its role in BDL from hepatic trauma is under-studied. In post-cholecystectomy bile leaks, trans-papillary stenting (TPS) of the bile duct in addition to endoscopic sphincterotomy (ES) improves outcomes compared to ES alone, particularly in patients with major leaks. These endoscopic interventions eliminate the pressure gradient between the bile duct and the duodenum which leads to preferential flow of bile into the duodenum. TPS may have the added benefit of bypassing the cystic duct orifice. However, in traumatic BDL, the small caliber intrahepatic ducts which are disrupted may be less sensitive to the effects of endoscopic therapy. In particular, the role of TPS in traumatic BDL is called into question. We hypothesize that ERCP with ES alone in traumatic BDL is non-inferior to ERCP with ES + TPS.
Methods: In this single-institution retrospective cohort study, patients > 18yo who were diagnosed with BDL from hepatic trauma from 2014 to 2024 were reviewed. The primary outcome was time to perihepatic drain removal after ERCP with ES alone versus ES+TPS. The secondary outcomes were time to perihepatic drain removal after ERCP versus no ERCP and rate of follow-up after TPS placement. Statistical analyses were performed in Microsoft Excel. Paired 2-sided Fischer’s t-tests were used to evaluate primary and secondary outcomes. Multivariate logistic regression was used to account for type of endoscopic intervention, need for angioembolization, and liver injury grade as defined by American Association of Surgery of Trauma.
Results: Among 25 patients in the study cohort, 14 underwent ERCP with ES-only, 5 underwent ERCP with ES+TPS, and 6 did not undergo ERCP. One patient died within 48 hours of presentation and was excluded.
Mean time to drain removal was 11.4 days in the ES-only group vs. 28.8 days in the ES+TPS group (P = 0.017). In a multivariate logistic regression model, angioembolization (P = 0.032) and TPS placement (P=0.009) were associated with increased time to drain removal. Among patients who underwent TPS placement, 1 out of 5 was unable to follow up for stent removal due to difficulties with health insurance.
Discussion: In BDL from hepatic trauma, ERCP with ES alone may be non-inferior to ES+TPS and avoids the risk of loss of follow-up for TPS removal. Further study is needed to determine whether ERCP is truly beneficial in treating BDL from hepatic trauma.
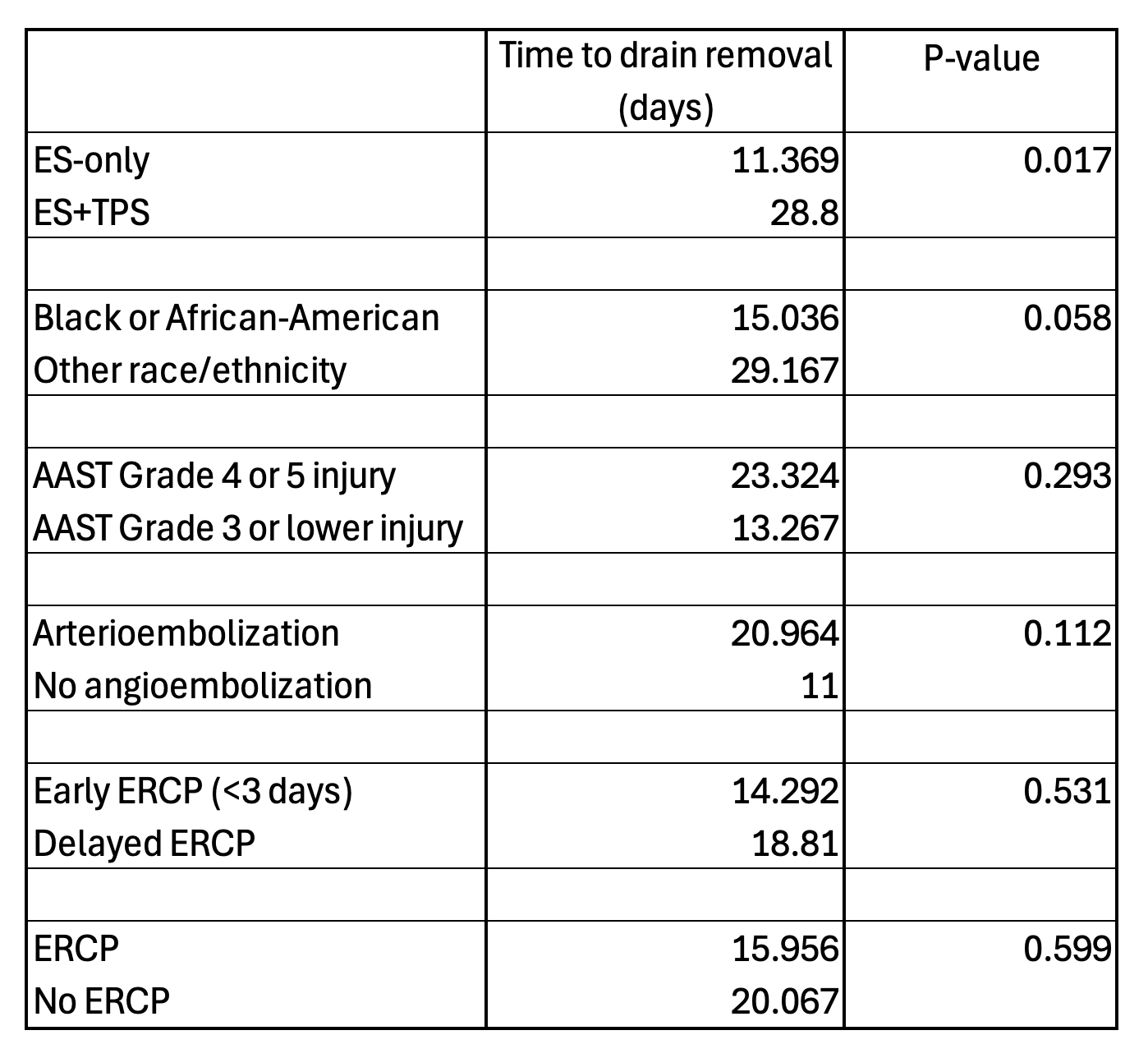
Figure: Table 1. Average time to drain removal and P-values of paired 2-sided t-tests, comparing the following elements: type of endoscopic intervention performed, race, liver injury grade as measured by American Association of Trauma Surgery (AAST) Liver Injury Scale, need for angioembolization, early vs. delayed ERCP, and ERCP vs. conservative management.
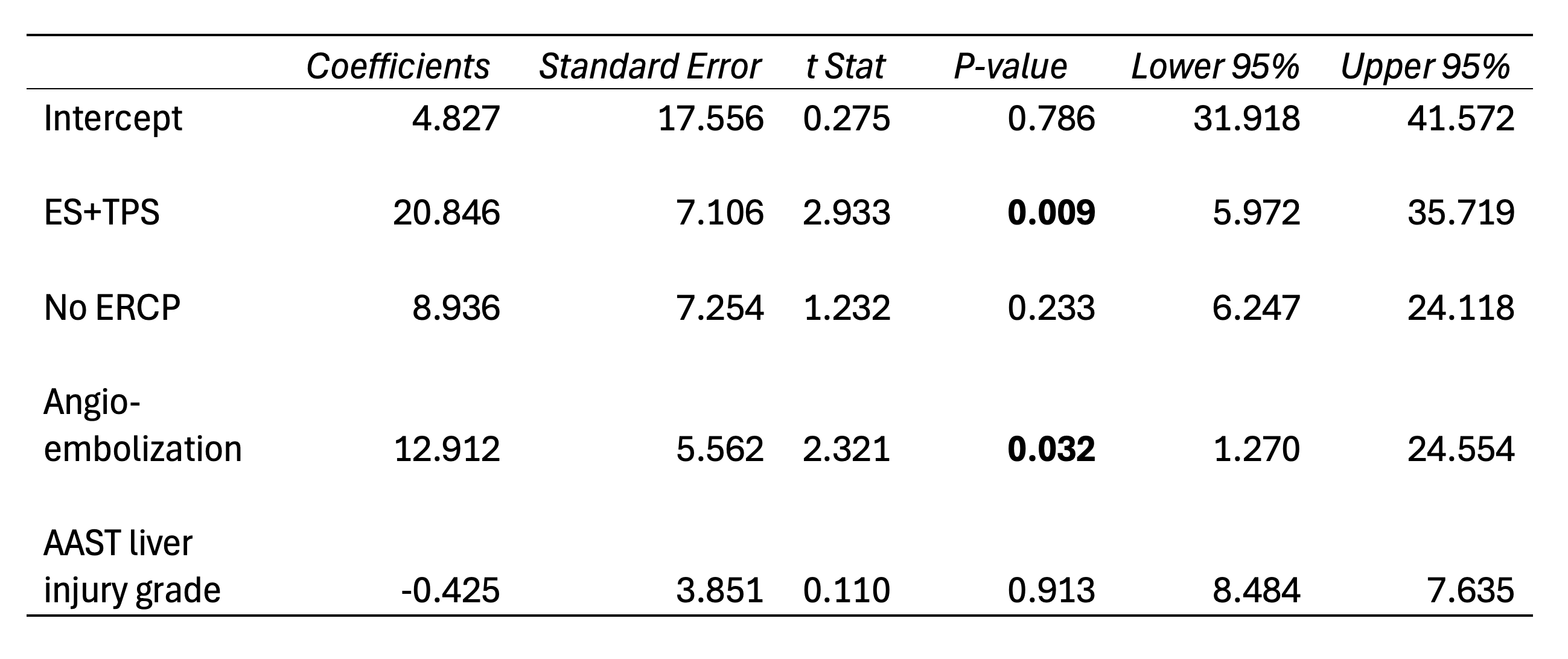
Figure: Table 2. Results of multivariate logistic regression model accounting for the following elements: type of endoscopic intervention performed, whether or not ERCP was performed, need for angioembolization, and liver injury grade as measured by American Association of Trauma Surgery (AAST) Livery Injury Scale.
Disclosures:
Varun Angajala indicated no relevant financial relationships.
Jacqueline Liu indicated no relevant financial relationships.
Christopher Huang: Olympus – Consultant.
Varun Angajala, MS, MD1, Jacqueline Liu, MD2, Christopher Huang, MD3. P4326 - Is ERCP Helpful in Traumatic Bile Leaks?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
