Tuesday Poster Session
Category: Biliary/Pancreas
P4313 - GLP1-RA-Based Medications in Patients With Obesity and Chronic Pancreatitis Are Associated With Decreased Cardiac Events Without Increased Risk of Pancreatic Cancer
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Shaina Ailawadi, MD
Case Western Reserve University/University Hospitals
University Heights, OH
Presenting Author(s)
Shaina Ailawadi, MD1, Abbinaya Elangovan, MD2, Apoorva K. Chandar, MBBS, MPH3, Raj Shah, MD4
1Case Western Reserve University/University Hospitals, University Heights, OH; 2Carilion Clinic, Roanoke, VA; 3Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 4The Ohio State University Wexner Medical Center, Columbus, OH
Introduction: Glucagon-like peptide-1 agonist-based medication (GLP-1RA) use has risen by 600% among Americans with obesity over the last six years. Prior studies have shown that GLP1-RA use decreases the incidence of major adverse cardiac events (MACE) in patients with obesity. However, given the association of GLP1-RA use with pancreatitis and the theoretical concern for pancreatic cancer, their use in patients with chronic pancreatitis (CP) remains unclear. We investigated the association of GLP1-RA use and CP incidence as well as the risk of pancreatic cancer and MACE in those with CP and obesity.
Methods: We performed a retrospective cohort study using ICD.10 codes using the TriNetX, a healthcare database with over 119 million patients in the United States. In the first analysis, among obese patients with pre-existing CP, we compared the 5-year incidence of MACE (acute myocardial infarction, stroke, acute heart failure, unstable angina) and pancreatic cancer between GLP1-RA (tirzepatide, liraglutide, dulaglutide, or semaglutide) users and non-users (Table 1A). Both groups had exclusions of history of prior pancreatic cancer. In the next analysis, we compared the 5-year incidence of CP between patients with obesity with and without GLP1-RA use (Table 1B). Patients with prior CP or pancreatic cancer were excluded. In both analyses, cohorts were propensity score matched (PSM) on age, sex, tobacco use, alcohol use, hypertension, diabetes mellitus, hyperlipidemia, and obesity. P-values < 0.05 were statistically significant.
Results: Among 18,352,024 patients with obesity in the database, there were 48,956 patients with obesity and CP, and of those, 3,739 patients who were prescribed a GLP-1RA in this study. After PSM, patients with obesity, CP, and GLP1-RA use had a lower incidence of MACE (6.59% vs. 11.33%, OR 0.55 [0.46, 0.66]) (Table 2A) and pancreatic cancer (0.45% vs. 3.25%, OR 0.14 [0.08, 0.23]) (Table 2B) compared to those without GLP-1RA use. Further, patients with obesity and GLP1-RA use had decreased risk of developing CP (0.12% vs. 0.33%, OR 0.36 [0.34, 0.39]) compared to those without GLP1-RA use (Table 2C).
Discussion: Our findings indicate that among patients with obesity and chronic pancreatitis, GLP1-RA use is associated with a significantly decreased risk of both MACE and pancreatic cancer. Among patients with obesity, GLP1-RA use did not result in increased incidence of developing CP. These results support the continued use of GLP1-RA in obese patients with chronic pancreatitis.
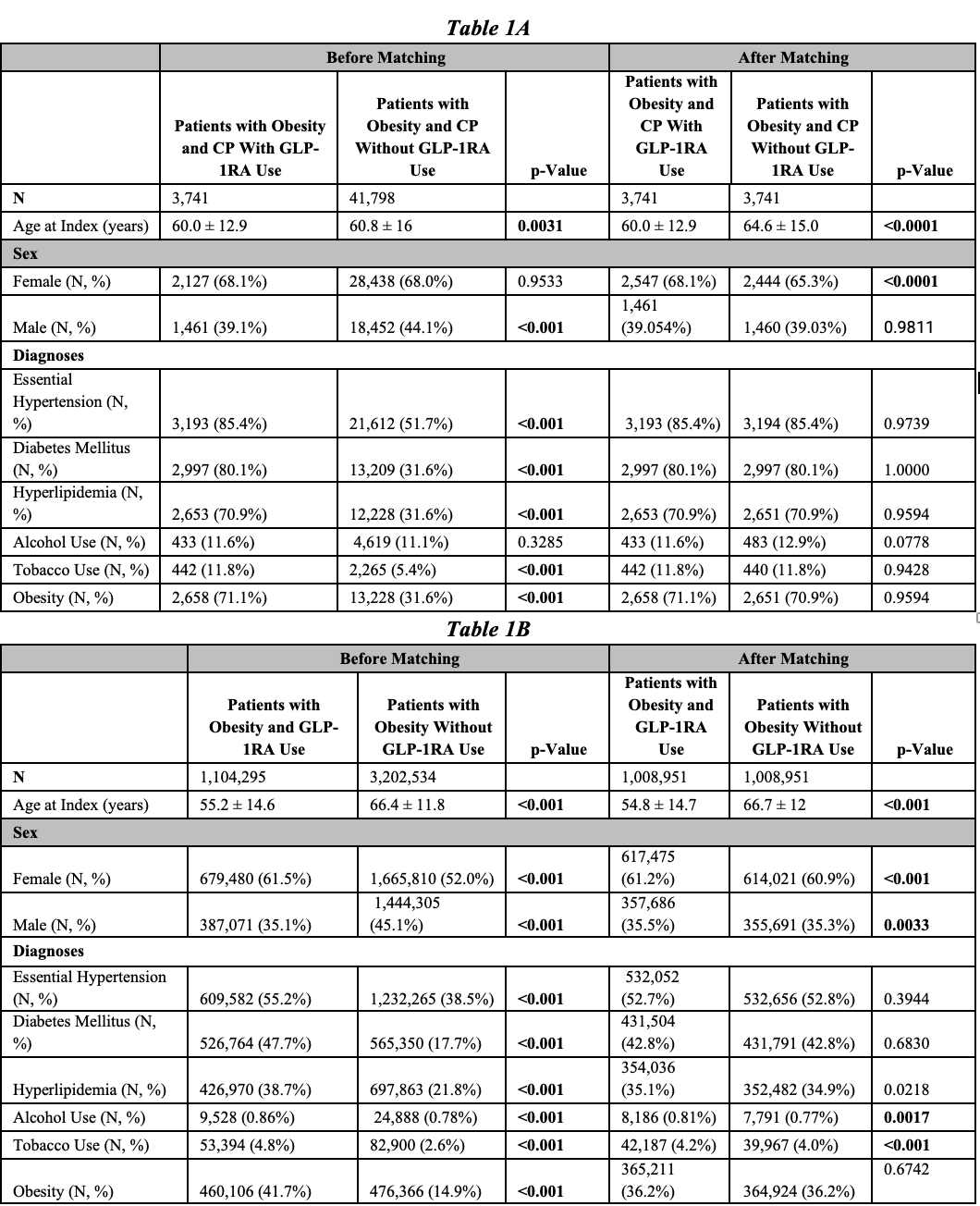
Figure: Table 1A. Baseline characteristics and comorbidities for patients with obesity and chronic pancreatitis with GLP-1RA use compared to those patients with obesity and chronic pancreatitis without GLP-1RA use before and after propensity score matching.
Table 1B. Baseline characteristics and comorbidities for patients with obesity and GLP-1RA use compared to those patients with obesity without GLP-1RA use before and after propensity score matching.
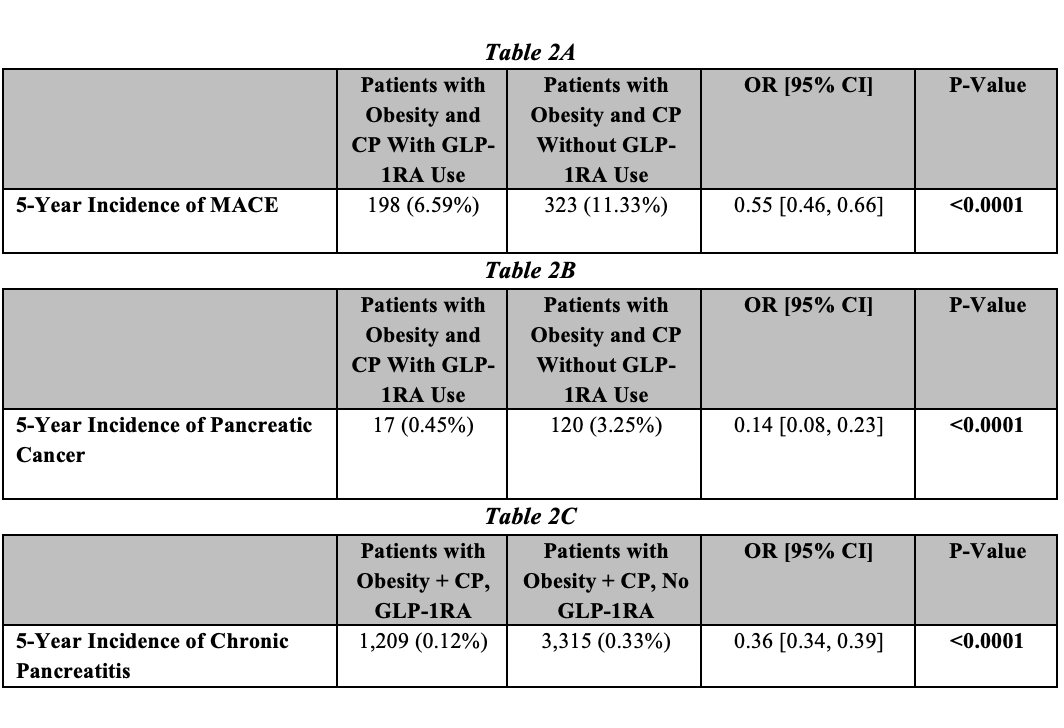
Figure: Table 2A. 5-year incidence of MACE in patients with obesity and chronic pancreatitis with GLP-1RA use compared to patients with obesity and chronic pancreatitis without GLP-1RA use after propensity score matching, with odds ratios and 95% confidence intervals.
Table 2B. 5-year incidence of pancreatic cancer in patients with obesity and chronic pancreatitis with GLP-1RA use compared to patients with obesity and chronic pancreatitis without GLP-1RA use after propensity score matching, with odds ratios and 95% confidence intervals.
Table 2C. 5-year incidence of chronic pancreatitis in patients with obesity and GLP-1RA use compared to patients with obesity without GLP-1RA use after propensity score matching, with odds ratios and 95% confidence intervals.
Disclosures:
Shaina Ailawadi indicated no relevant financial relationships.
Abbinaya Elangovan indicated no relevant financial relationships.
Apoorva Chandar indicated no relevant financial relationships.
Raj Shah indicated no relevant financial relationships.
Shaina Ailawadi, MD1, Abbinaya Elangovan, MD2, Apoorva K. Chandar, MBBS, MPH3, Raj Shah, MD4. P4313 - GLP1-RA-Based Medications in Patients With Obesity and Chronic Pancreatitis Are Associated With Decreased Cardiac Events Without Increased Risk of Pancreatic Cancer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Case Western Reserve University/University Hospitals, University Heights, OH; 2Carilion Clinic, Roanoke, VA; 3Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 4The Ohio State University Wexner Medical Center, Columbus, OH
Introduction: Glucagon-like peptide-1 agonist-based medication (GLP-1RA) use has risen by 600% among Americans with obesity over the last six years. Prior studies have shown that GLP1-RA use decreases the incidence of major adverse cardiac events (MACE) in patients with obesity. However, given the association of GLP1-RA use with pancreatitis and the theoretical concern for pancreatic cancer, their use in patients with chronic pancreatitis (CP) remains unclear. We investigated the association of GLP1-RA use and CP incidence as well as the risk of pancreatic cancer and MACE in those with CP and obesity.
Methods: We performed a retrospective cohort study using ICD.10 codes using the TriNetX, a healthcare database with over 119 million patients in the United States. In the first analysis, among obese patients with pre-existing CP, we compared the 5-year incidence of MACE (acute myocardial infarction, stroke, acute heart failure, unstable angina) and pancreatic cancer between GLP1-RA (tirzepatide, liraglutide, dulaglutide, or semaglutide) users and non-users (Table 1A). Both groups had exclusions of history of prior pancreatic cancer. In the next analysis, we compared the 5-year incidence of CP between patients with obesity with and without GLP1-RA use (Table 1B). Patients with prior CP or pancreatic cancer were excluded. In both analyses, cohorts were propensity score matched (PSM) on age, sex, tobacco use, alcohol use, hypertension, diabetes mellitus, hyperlipidemia, and obesity. P-values < 0.05 were statistically significant.
Results: Among 18,352,024 patients with obesity in the database, there were 48,956 patients with obesity and CP, and of those, 3,739 patients who were prescribed a GLP-1RA in this study. After PSM, patients with obesity, CP, and GLP1-RA use had a lower incidence of MACE (6.59% vs. 11.33%, OR 0.55 [0.46, 0.66]) (Table 2A) and pancreatic cancer (0.45% vs. 3.25%, OR 0.14 [0.08, 0.23]) (Table 2B) compared to those without GLP-1RA use. Further, patients with obesity and GLP1-RA use had decreased risk of developing CP (0.12% vs. 0.33%, OR 0.36 [0.34, 0.39]) compared to those without GLP1-RA use (Table 2C).
Discussion: Our findings indicate that among patients with obesity and chronic pancreatitis, GLP1-RA use is associated with a significantly decreased risk of both MACE and pancreatic cancer. Among patients with obesity, GLP1-RA use did not result in increased incidence of developing CP. These results support the continued use of GLP1-RA in obese patients with chronic pancreatitis.
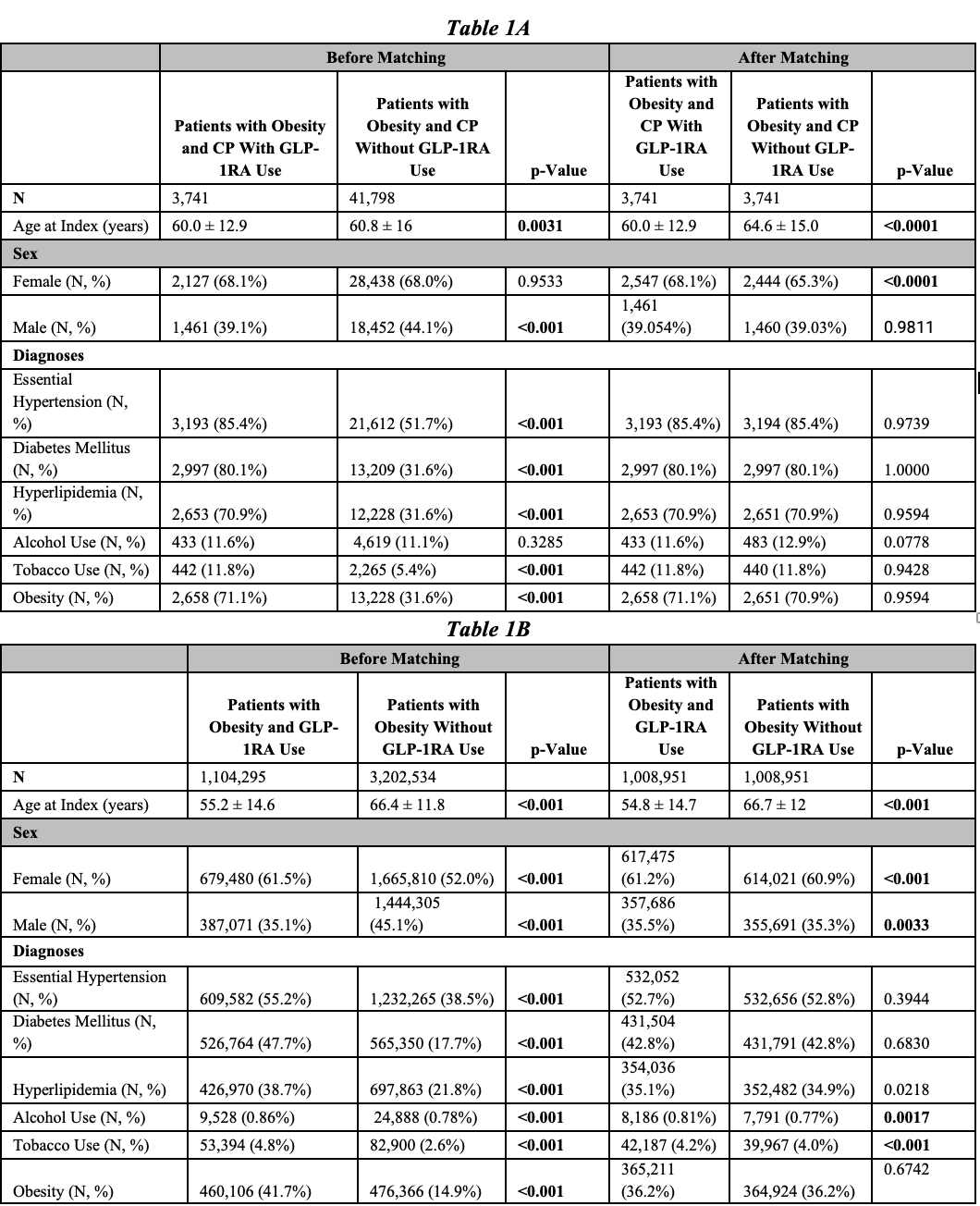
Figure: Table 1A. Baseline characteristics and comorbidities for patients with obesity and chronic pancreatitis with GLP-1RA use compared to those patients with obesity and chronic pancreatitis without GLP-1RA use before and after propensity score matching.
Table 1B. Baseline characteristics and comorbidities for patients with obesity and GLP-1RA use compared to those patients with obesity without GLP-1RA use before and after propensity score matching.
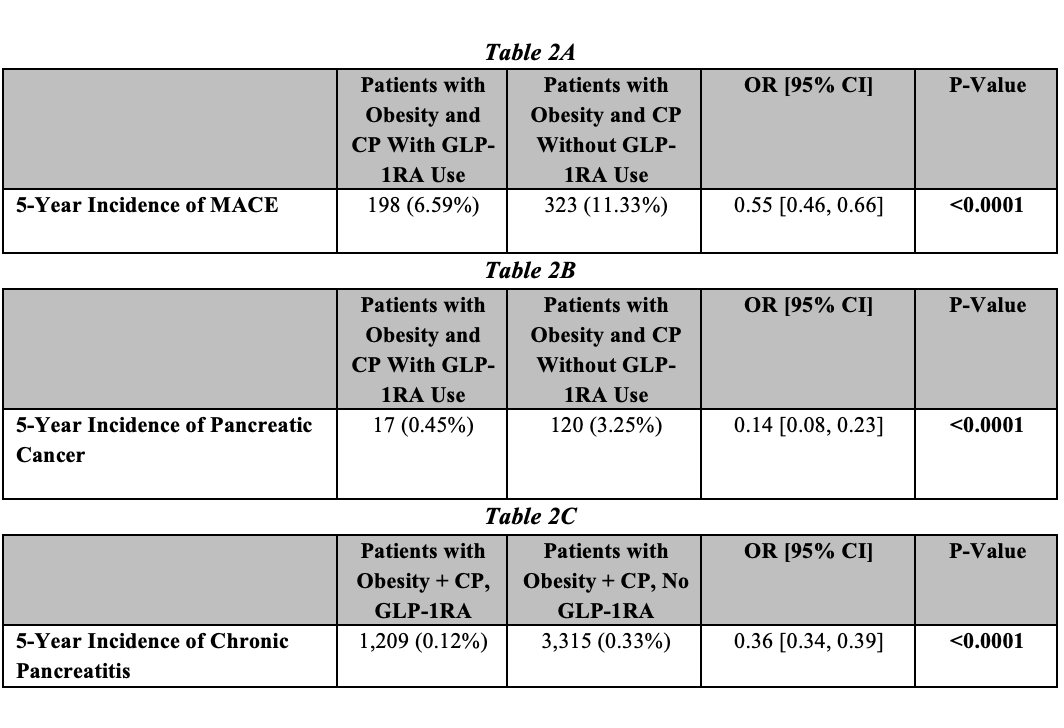
Figure: Table 2A. 5-year incidence of MACE in patients with obesity and chronic pancreatitis with GLP-1RA use compared to patients with obesity and chronic pancreatitis without GLP-1RA use after propensity score matching, with odds ratios and 95% confidence intervals.
Table 2B. 5-year incidence of pancreatic cancer in patients with obesity and chronic pancreatitis with GLP-1RA use compared to patients with obesity and chronic pancreatitis without GLP-1RA use after propensity score matching, with odds ratios and 95% confidence intervals.
Table 2C. 5-year incidence of chronic pancreatitis in patients with obesity and GLP-1RA use compared to patients with obesity without GLP-1RA use after propensity score matching, with odds ratios and 95% confidence intervals.
Disclosures:
Shaina Ailawadi indicated no relevant financial relationships.
Abbinaya Elangovan indicated no relevant financial relationships.
Apoorva Chandar indicated no relevant financial relationships.
Raj Shah indicated no relevant financial relationships.
Shaina Ailawadi, MD1, Abbinaya Elangovan, MD2, Apoorva K. Chandar, MBBS, MPH3, Raj Shah, MD4. P4313 - GLP1-RA-Based Medications in Patients With Obesity and Chronic Pancreatitis Are Associated With Decreased Cardiac Events Without Increased Risk of Pancreatic Cancer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

