Tuesday Poster Session
Category: Biliary/Pancreas
P4312 - Pancreatic Cancer Burden: Racial and Regional Differences in US National Inpatient Sample Data
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MA
Mohammad Alqaisieh, MD
Hamilton Health Care System
Dalton, Georgia
Presenting Author(s)
Bugra Zengin, MD, Jasneet Randhawa, MD, Zaid Zahid, MD, Mohammad Alqaisieh, MD, Maheshkumar Desai, MD
Hamilton Health Care System, Dalton, GA
Introduction: Pancreatic cancer remains the malignancy with the poorest prognosis, evidenced by a 5-year survival rate of only 9%, largely due to late-stage diagnosis. Risk factors include age over 50, smoking, obesity, and genetic predispositions, though no standardized screening guidelines currently exist. This study explores racial disparities, socioeconomic factors, regional variations, and procedural access among pancreatic cancer patients.
Methods: Using the Nationwide Inpatient Sample (NIS) database, patients discharged between 2019 and 2020 with pancreatic cancer were identified through ICD-10 codes and categorized by race. Statistical analyses, performed using STATA, examined racial prevalence, hospital metrics (length of stay, total charges), procedure rates, and comorbidities such as diabetes, obesity, CHF, cirrhosis, CKD, and COPD.
Results: Among 74,584 patients (mean age 68.47 years, 50.96% male), 69.12% were White, 13.30% Black, 8.5% Hispanic, and 8.9% Other. Mortality rates were comparable (p = 0.0069). Paracentesis was performed in 8.3% of cases without racial disparities (p = 0.3577). Cancer-related procedures (pancreatic, gastric, bile duct surgeries) varied significantly, highest in White (24.09%) and lowest in Black (15.78%) (p < 0.001) (see table). White patients had the highest COPD (10.9%) and smoking rates (27.9%), while Black patients had the highest CHF (11.49%), CKD (15.83%), obesity (13.86%), and diabetes (46.52%) (p < 0.001). Cirrhosis was most prevalent in Hispanics (4.06%, p = 0.0306). Black patients had the longest stays (7.8 days), while Hispanic patients had the highest total charges (+$119,733) (p < 0.001). Most White (35.42%), Black (54.59%), and Hispanic (41.64%) patients were hospitalized in the South, while Other groups were mainly in the West (34.95%) (p < 0.001). Pancreatic cancer was more prevalent in low-income Black (47.47%) and Hispanic (35.43%) populations (p < 0.001).
Discussion: Pancreatic cancer outcomes and healthcare experiences show disparities by race, region, and socioeconomic status. Black patients underwent procedures at the lowest rates, and both Black and Hispanic patients experienced more prolonged hospital stays and greater financial burdens. Variations in comorbidities such as diabetes and cirrhosis were also observed. Addressing these disparities requires equitable access to healthcare, targeted screening strategies, and tailored socioeconomic interventions. Further research should explore underlying causes and develop actionable solutions.
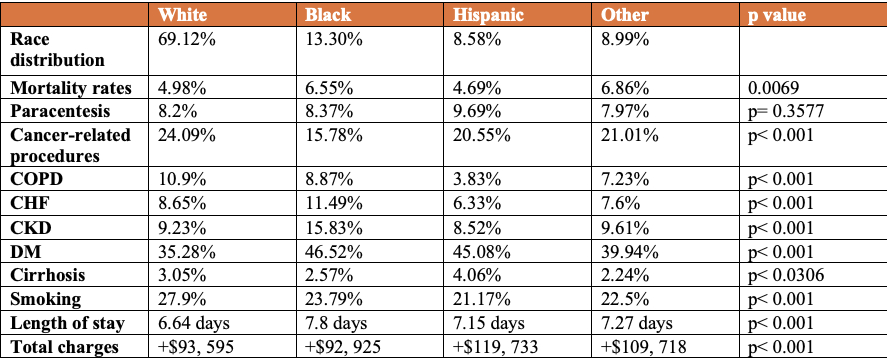
Figure: Racial Disparities in Mortality, Comorbidities, Procedures, and Hospital Metrics
Disclosures:
Bugra Zengin indicated no relevant financial relationships.
Jasneet Randhawa indicated no relevant financial relationships.
Zaid Zahid indicated no relevant financial relationships.
Mohammad Alqaisieh indicated no relevant financial relationships.
Maheshkumar Desai indicated no relevant financial relationships.
Bugra Zengin, MD, Jasneet Randhawa, MD, Zaid Zahid, MD, Mohammad Alqaisieh, MD, Maheshkumar Desai, MD. P4312 - Pancreatic Cancer Burden: Racial and Regional Differences in US National Inpatient Sample Data, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Hamilton Health Care System, Dalton, GA
Introduction: Pancreatic cancer remains the malignancy with the poorest prognosis, evidenced by a 5-year survival rate of only 9%, largely due to late-stage diagnosis. Risk factors include age over 50, smoking, obesity, and genetic predispositions, though no standardized screening guidelines currently exist. This study explores racial disparities, socioeconomic factors, regional variations, and procedural access among pancreatic cancer patients.
Methods: Using the Nationwide Inpatient Sample (NIS) database, patients discharged between 2019 and 2020 with pancreatic cancer were identified through ICD-10 codes and categorized by race. Statistical analyses, performed using STATA, examined racial prevalence, hospital metrics (length of stay, total charges), procedure rates, and comorbidities such as diabetes, obesity, CHF, cirrhosis, CKD, and COPD.
Results: Among 74,584 patients (mean age 68.47 years, 50.96% male), 69.12% were White, 13.30% Black, 8.5% Hispanic, and 8.9% Other. Mortality rates were comparable (p = 0.0069). Paracentesis was performed in 8.3% of cases without racial disparities (p = 0.3577). Cancer-related procedures (pancreatic, gastric, bile duct surgeries) varied significantly, highest in White (24.09%) and lowest in Black (15.78%) (p < 0.001) (see table). White patients had the highest COPD (10.9%) and smoking rates (27.9%), while Black patients had the highest CHF (11.49%), CKD (15.83%), obesity (13.86%), and diabetes (46.52%) (p < 0.001). Cirrhosis was most prevalent in Hispanics (4.06%, p = 0.0306). Black patients had the longest stays (7.8 days), while Hispanic patients had the highest total charges (+$119,733) (p < 0.001). Most White (35.42%), Black (54.59%), and Hispanic (41.64%) patients were hospitalized in the South, while Other groups were mainly in the West (34.95%) (p < 0.001). Pancreatic cancer was more prevalent in low-income Black (47.47%) and Hispanic (35.43%) populations (p < 0.001).
Discussion: Pancreatic cancer outcomes and healthcare experiences show disparities by race, region, and socioeconomic status. Black patients underwent procedures at the lowest rates, and both Black and Hispanic patients experienced more prolonged hospital stays and greater financial burdens. Variations in comorbidities such as diabetes and cirrhosis were also observed. Addressing these disparities requires equitable access to healthcare, targeted screening strategies, and tailored socioeconomic interventions. Further research should explore underlying causes and develop actionable solutions.
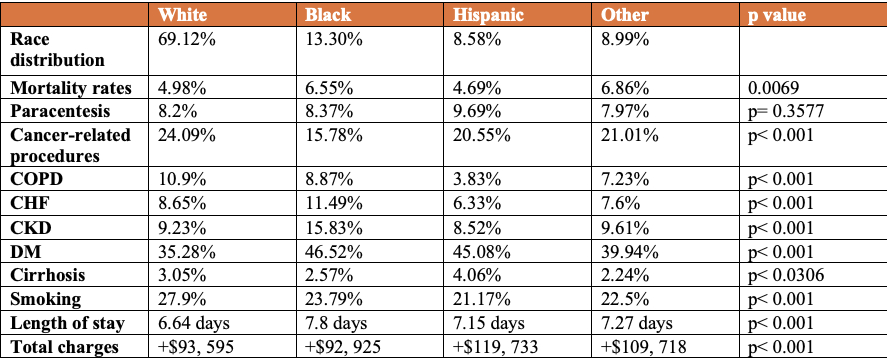
Figure: Racial Disparities in Mortality, Comorbidities, Procedures, and Hospital Metrics
Disclosures:
Bugra Zengin indicated no relevant financial relationships.
Jasneet Randhawa indicated no relevant financial relationships.
Zaid Zahid indicated no relevant financial relationships.
Mohammad Alqaisieh indicated no relevant financial relationships.
Maheshkumar Desai indicated no relevant financial relationships.
Bugra Zengin, MD, Jasneet Randhawa, MD, Zaid Zahid, MD, Mohammad Alqaisieh, MD, Maheshkumar Desai, MD. P4312 - Pancreatic Cancer Burden: Racial and Regional Differences in US National Inpatient Sample Data, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
