Tuesday Poster Session
Category: Biliary/Pancreas
P4296 - Protein-Energy Malnutrition Fuels Morbidity and Healthcare Burden in Necrotizing Pancreatitis: Insights from a National Cohort
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Angelin Raju, MD (she/her/hers)
Texas Health Resources HEB/ Denton
Bedford, TX
Presenting Author(s)
Angelin Raju, MD1, Anish Jomy, MBBS2, Arthur CHIDI. Igbo, MD, MPH3, Maher Taha, MD4, Aashish Anunaya, MD5
1Texas health, Bedford, TX; 2Methodist Health System, Richardson, TX; 3Texas Health Resources HEB/Denton Internal Medicine Program, Lewisville, TX; 4Texas Health Resources, Irving, TX; 5Texas Health Resources HEB/ Denton, Bedford, TX
Introduction: Protein Energy Malnutrition (PEM) is a known predictor of adverse outcomes in critically ill patients. However, its impact on clinical and resource utilization outcomes in patients with Necrotizing Pancreatitis (NP) remains underexplored.
Methods: We conducted a retrospective cohort study using the National Inpatient Sample (NIS) from 2018-2022, identifying adult hospitalizations with a diagnosis of NP using ICD-10-CM codes. PEM was classified as mild-to-moderate, severe, or unspecified. Survey-weighted analyses were performed to obtain national estimates. Multivariable logistic regression was used to calculate adjusted odds ratios (AOR) for in-hospital outcomes, controlling for age, sex, race, and comorbidity index (Elixhauser).
Results: Among 75,380 weighted hospitalizations for NP, approximately 15,570 (20.6%) had concurrent PEM. Of these, 4565 had mild/moderate PEM, 8030 had severe PEM and 3070 had unspecified PEM. In NP with PEM cohort the mean age was 66 years (-17 years, p< 0.001) with males about 63.6%, and had significantly higher Elixhauser scores (88% vs 67%, p< 0.001). Most common race were White (74%), followed by Black (11%), and Hispanic (9.8%). Overall in-hospital mortality was 2.4 % for NP and it was independently significant in PEM patients (AOR 1.5, p< 0.001) with Mild/moderate PEM (AOR 1.9, p< 0.001), Severe PEM (AOR 2.8, p< 0.001) and Unspecified PEM (AOR 2.2, p< 0.001). PEM patients had significantly higher hospital charges and longer length of stay unadjusted, with maximum for severe PEM. PEM increased the risk of Acute Kidney Injury [AKI] (26.7% vs 19.45%, p< 0.001), VTE (4.9% vs 1.4%, p< 0.001), Sepsis (14.8% vs 5.4%, p< 0.001) and Splanchnic Venous Thrombosis [SVT] (15% vs 10.2%, p< 0.001) in unadjusted model. Risk increases with mild/moderate< unspecified PEM< severe. Higher comorbidity burden (Elixhauser score), and male sex are independent risk factors for AKI, sepsis and SVT. Older age increased the risk of AKI and sepsis.
Discussion: In this large national cohort of patients hospitalized with NP, over 20% had PEM, which was linked to worse outcomes. Increasing PEM severity correlated with higher mortality, longer hospital stays, greater costs, and more complications, including AKI, VTE, sepsis, and SVT. Severe PEM remained an independent predictor of mortality after adjustment. Male sex, older age, and higher comorbidity burden further increased risk. These findings underscore the importance of early nutritional assessment and intervention.
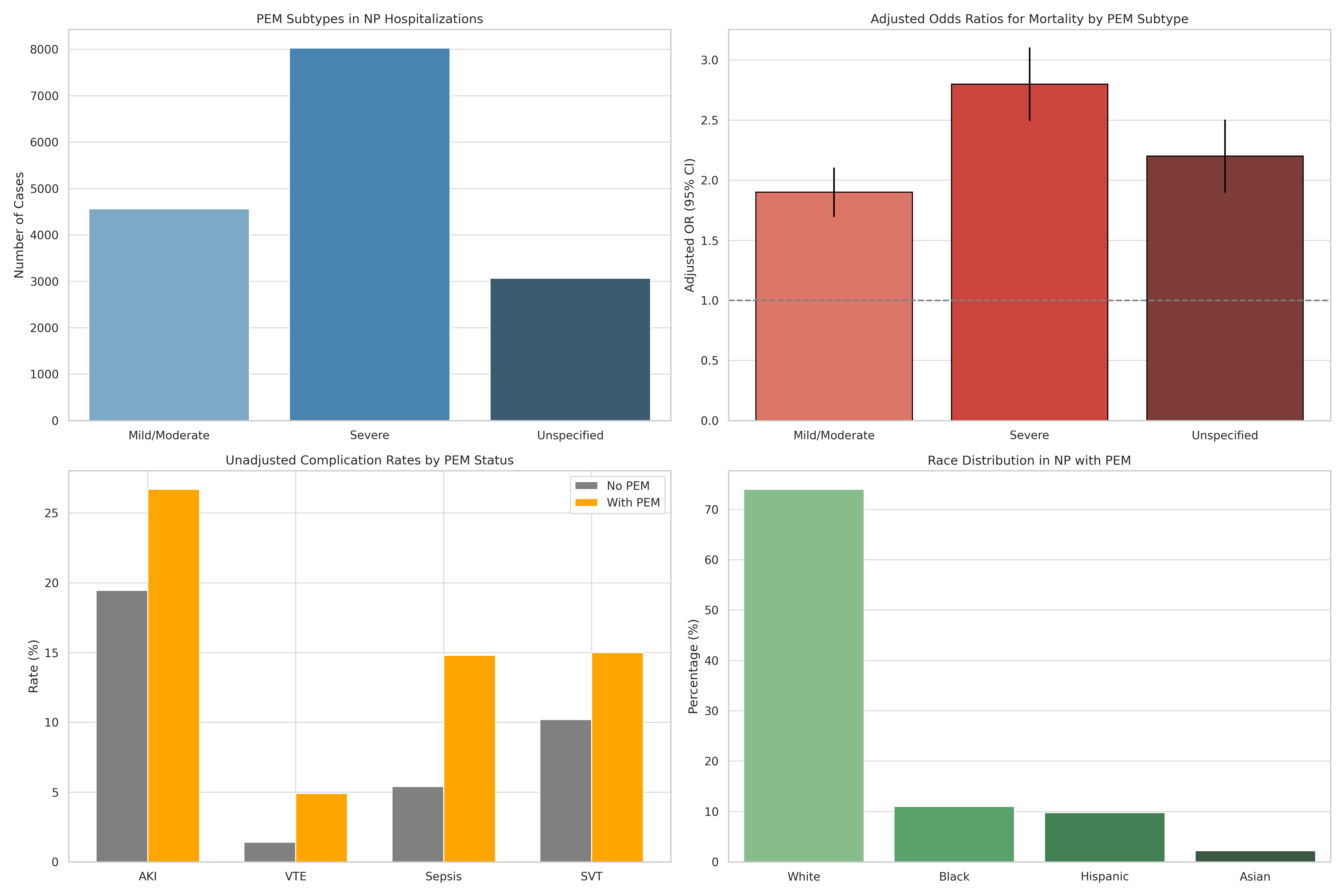
Figure: Graphical representation of significant findings in NP with PEM
Disclosures:
Angelin Raju indicated no relevant financial relationships.
Anish Jomy indicated no relevant financial relationships.
Arthur Igbo indicated no relevant financial relationships.
Maher Taha indicated no relevant financial relationships.
Aashish Anunaya indicated no relevant financial relationships.
Angelin Raju, MD1, Anish Jomy, MBBS2, Arthur CHIDI. Igbo, MD, MPH3, Maher Taha, MD4, Aashish Anunaya, MD5. P4296 - Protein-Energy Malnutrition Fuels Morbidity and Healthcare Burden in Necrotizing Pancreatitis: Insights from a National Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Texas health, Bedford, TX; 2Methodist Health System, Richardson, TX; 3Texas Health Resources HEB/Denton Internal Medicine Program, Lewisville, TX; 4Texas Health Resources, Irving, TX; 5Texas Health Resources HEB/ Denton, Bedford, TX
Introduction: Protein Energy Malnutrition (PEM) is a known predictor of adverse outcomes in critically ill patients. However, its impact on clinical and resource utilization outcomes in patients with Necrotizing Pancreatitis (NP) remains underexplored.
Methods: We conducted a retrospective cohort study using the National Inpatient Sample (NIS) from 2018-2022, identifying adult hospitalizations with a diagnosis of NP using ICD-10-CM codes. PEM was classified as mild-to-moderate, severe, or unspecified. Survey-weighted analyses were performed to obtain national estimates. Multivariable logistic regression was used to calculate adjusted odds ratios (AOR) for in-hospital outcomes, controlling for age, sex, race, and comorbidity index (Elixhauser).
Results: Among 75,380 weighted hospitalizations for NP, approximately 15,570 (20.6%) had concurrent PEM. Of these, 4565 had mild/moderate PEM, 8030 had severe PEM and 3070 had unspecified PEM. In NP with PEM cohort the mean age was 66 years (-17 years, p< 0.001) with males about 63.6%, and had significantly higher Elixhauser scores (88% vs 67%, p< 0.001). Most common race were White (74%), followed by Black (11%), and Hispanic (9.8%). Overall in-hospital mortality was 2.4 % for NP and it was independently significant in PEM patients (AOR 1.5, p< 0.001) with Mild/moderate PEM (AOR 1.9, p< 0.001), Severe PEM (AOR 2.8, p< 0.001) and Unspecified PEM (AOR 2.2, p< 0.001). PEM patients had significantly higher hospital charges and longer length of stay unadjusted, with maximum for severe PEM. PEM increased the risk of Acute Kidney Injury [AKI] (26.7% vs 19.45%, p< 0.001), VTE (4.9% vs 1.4%, p< 0.001), Sepsis (14.8% vs 5.4%, p< 0.001) and Splanchnic Venous Thrombosis [SVT] (15% vs 10.2%, p< 0.001) in unadjusted model. Risk increases with mild/moderate< unspecified PEM< severe. Higher comorbidity burden (Elixhauser score), and male sex are independent risk factors for AKI, sepsis and SVT. Older age increased the risk of AKI and sepsis.
Discussion: In this large national cohort of patients hospitalized with NP, over 20% had PEM, which was linked to worse outcomes. Increasing PEM severity correlated with higher mortality, longer hospital stays, greater costs, and more complications, including AKI, VTE, sepsis, and SVT. Severe PEM remained an independent predictor of mortality after adjustment. Male sex, older age, and higher comorbidity burden further increased risk. These findings underscore the importance of early nutritional assessment and intervention.
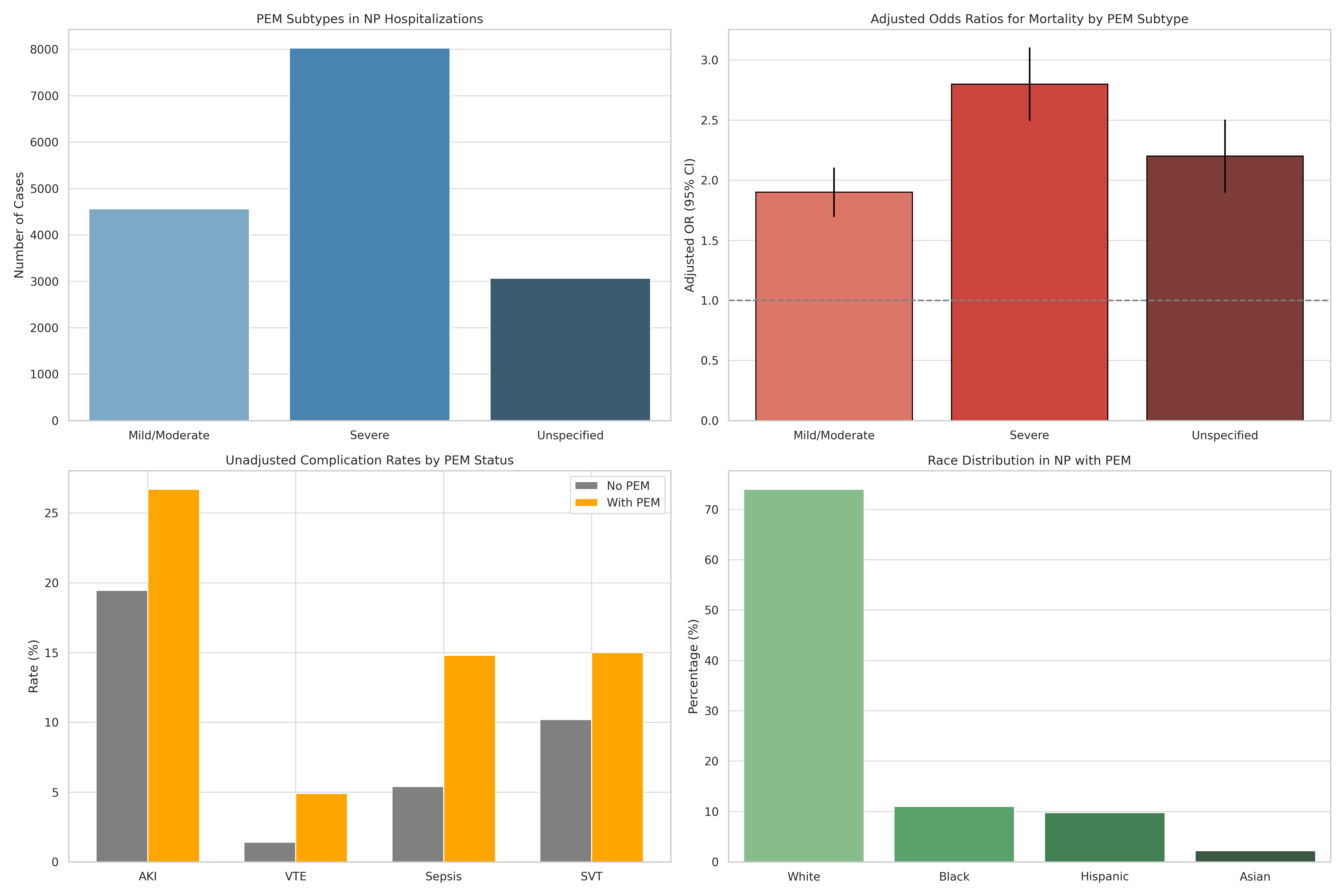
Figure: Graphical representation of significant findings in NP with PEM
Disclosures:
Angelin Raju indicated no relevant financial relationships.
Anish Jomy indicated no relevant financial relationships.
Arthur Igbo indicated no relevant financial relationships.
Maher Taha indicated no relevant financial relationships.
Aashish Anunaya indicated no relevant financial relationships.
Angelin Raju, MD1, Anish Jomy, MBBS2, Arthur CHIDI. Igbo, MD, MPH3, Maher Taha, MD4, Aashish Anunaya, MD5. P4296 - Protein-Energy Malnutrition Fuels Morbidity and Healthcare Burden in Necrotizing Pancreatitis: Insights from a National Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
