Sunday Poster Session
Category: Small Intestine
P1991 - Gastrointestinal Thrombotic Microangiopathy: A Rare and Potentially Fatal Complication of Renal Transplant
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Prakriti Ramamurthy, MBBS, MD (she/her/hers)
University of Massachusetts Chan Medical School - Baystate Health
Springfield, MA
Presenting Author(s)
Prakriti Ramamurthy, MBBS, MD1, Thanisha Santhosh, MBBS2, Shivalinga Shekar, MD, DrNB3, Raj Vigna. Venugopal, MBBS, DNB, DM3, Pranav Ramamurthy, MBBS, MD4, Advaith N. Rao, MBBS2, Rahul Ravindra, MBBS, MD5, Vinayak Bhat, 6
1University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA; 2M S Ramaiah Medical College, Bangalore, Karnataka, India; 3Manipal Hospital, Bangalore, Karnataka, India; 4University of Massachusetts Chan Medical School-Baystate Medical Center, Springfield, MA; 5White River Medical Center, Batesville, AR; 6Henry M. Gunn Senior High School, Palo Alto, CA
Introduction: Thrombotic microangiopathy (TMA) is a debilitating complication following renal transplantation, with an incidence rate reported to be between 0.8% and 14%. Isolated gastrointestinal (GI) involvement is a rarer subset, accounting for a mere 10% of these cases. This is a case of a renal transplant recipient who developed GI-limited TMA, which posed a significant diagnostic and therapeutic challenge.
Case Description/
Methods: A 28-year-old male with end-stage renal disease underwent a live-donor renal transplant in March 2015. 8 months later, he experienced acute antibody-mediated rejection that was managed with plasmapheresis and IV immunoglobulin, maintaining stable graft function for 8 years. In 2023, he presented with intermittent cramping abdominal pain and loose stools for one week. Empirical antibiotics were ineffective and initial infectious workup was negative. Persistent symptoms led to CMV PCR testing, revealing a viral load of 4 million copies. IV ganciclovir led to an initial clinical improvement. However, 2 weeks later, his creatinine increased significantly from baseline and a renal biopsy confirmed acute-on-chronic antibody-mediated rejection. Hemodialysis was initiated with subsequent improvement.
1 week after discharge, he returned with persistent non-bloody diarrhea and cramps. MMF was stopped due to suspected drug-induced colitis, but symptoms persisted. Labs showed anemia, leukopenia, thrombocytopenia, elevated LDH, low haptoglobin and schistocytes, raising suspicion for TMA. Endoscopy revealed duodenal erythema and diffuse colonic congestion and biopsy confirmed GI TMA without CMV inclusions. The patient underwent 9 plasma exchange (PLEX) sessions with marked symptomatic improvement in GI symptoms. A repeat renal biopsy showed chronic rejection without presence of renal TMA. The patient became PLEX-dependent, Eculizumab was considered but not initiated due to financial constraints and the patient ultimately succumbed to multiorgan failure.
Discussion: This case underscores the diagnostic complexity of GI TMA in renal transplant recipients. It often mimics other GI conditions such as infectious or drug-induced colitis, delaying accurate diagnosis. Maintaining a high index of suspicion for GI-limited TMA in transplant recipients presenting with unexplained gastrointestinal symptoms is important, especially in the context of hematologic abnormalities.
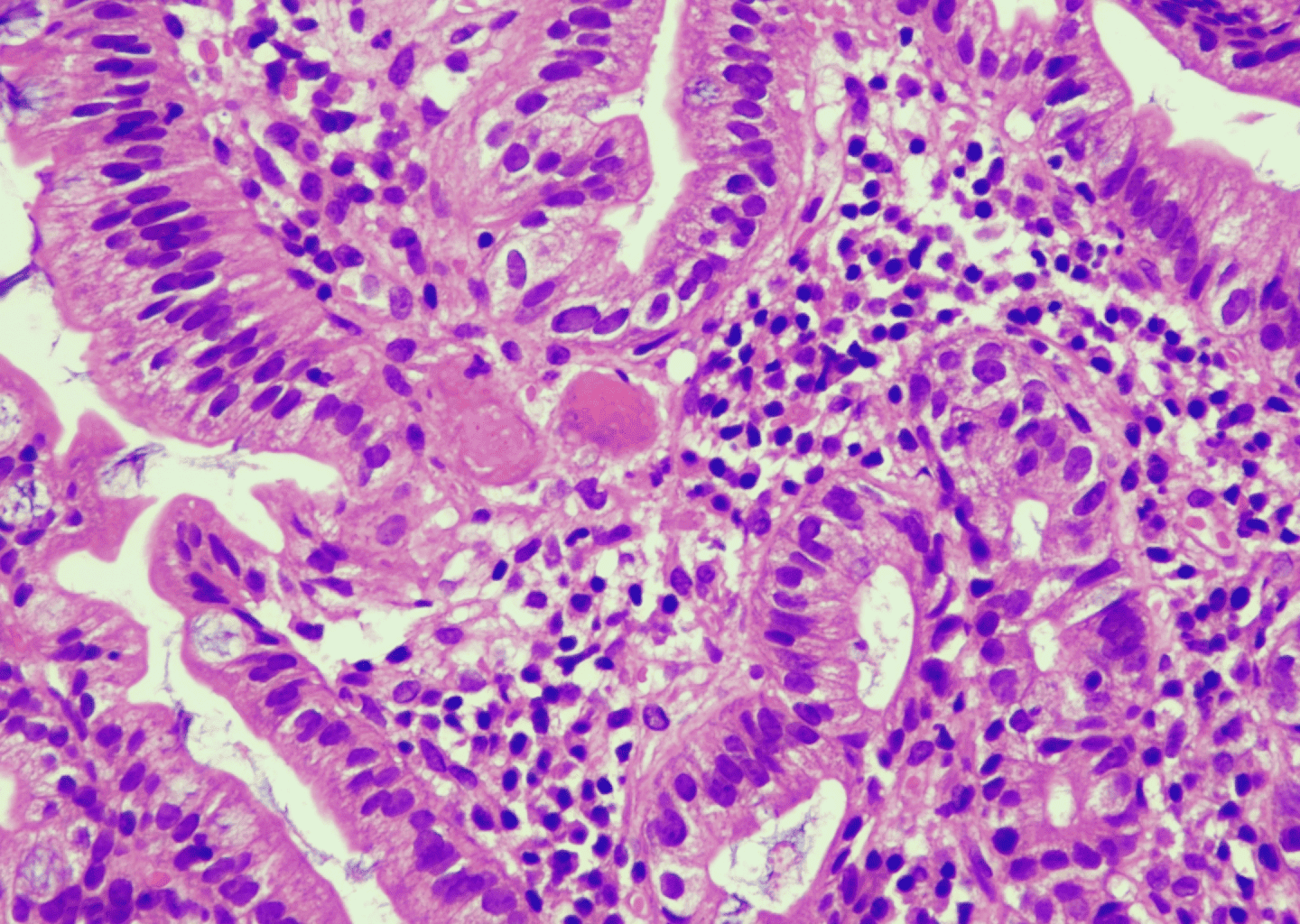
Figure: Duodenal biopsy showing fibrin thrombi obliterating the capillaries. (40x, H&E)
Disclosures:
Prakriti Ramamurthy indicated no relevant financial relationships.
Thanisha Santhosh indicated no relevant financial relationships.
Shivalinga Shekar indicated no relevant financial relationships.
Raj Venugopal indicated no relevant financial relationships.
Pranav Ramamurthy indicated no relevant financial relationships.
Advaith Rao indicated no relevant financial relationships.
Rahul Ravindra indicated no relevant financial relationships.
Vinayak Bhat indicated no relevant financial relationships.
Prakriti Ramamurthy, MBBS, MD1, Thanisha Santhosh, MBBS2, Shivalinga Shekar, MD, DrNB3, Raj Vigna. Venugopal, MBBS, DNB, DM3, Pranav Ramamurthy, MBBS, MD4, Advaith N. Rao, MBBS2, Rahul Ravindra, MBBS, MD5, Vinayak Bhat, 6. P1991 - Gastrointestinal Thrombotic Microangiopathy: A Rare and Potentially Fatal Complication of Renal Transplant, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA; 2M S Ramaiah Medical College, Bangalore, Karnataka, India; 3Manipal Hospital, Bangalore, Karnataka, India; 4University of Massachusetts Chan Medical School-Baystate Medical Center, Springfield, MA; 5White River Medical Center, Batesville, AR; 6Henry M. Gunn Senior High School, Palo Alto, CA
Introduction: Thrombotic microangiopathy (TMA) is a debilitating complication following renal transplantation, with an incidence rate reported to be between 0.8% and 14%. Isolated gastrointestinal (GI) involvement is a rarer subset, accounting for a mere 10% of these cases. This is a case of a renal transplant recipient who developed GI-limited TMA, which posed a significant diagnostic and therapeutic challenge.
Case Description/
Methods: A 28-year-old male with end-stage renal disease underwent a live-donor renal transplant in March 2015. 8 months later, he experienced acute antibody-mediated rejection that was managed with plasmapheresis and IV immunoglobulin, maintaining stable graft function for 8 years. In 2023, he presented with intermittent cramping abdominal pain and loose stools for one week. Empirical antibiotics were ineffective and initial infectious workup was negative. Persistent symptoms led to CMV PCR testing, revealing a viral load of 4 million copies. IV ganciclovir led to an initial clinical improvement. However, 2 weeks later, his creatinine increased significantly from baseline and a renal biopsy confirmed acute-on-chronic antibody-mediated rejection. Hemodialysis was initiated with subsequent improvement.
1 week after discharge, he returned with persistent non-bloody diarrhea and cramps. MMF was stopped due to suspected drug-induced colitis, but symptoms persisted. Labs showed anemia, leukopenia, thrombocytopenia, elevated LDH, low haptoglobin and schistocytes, raising suspicion for TMA. Endoscopy revealed duodenal erythema and diffuse colonic congestion and biopsy confirmed GI TMA without CMV inclusions. The patient underwent 9 plasma exchange (PLEX) sessions with marked symptomatic improvement in GI symptoms. A repeat renal biopsy showed chronic rejection without presence of renal TMA. The patient became PLEX-dependent, Eculizumab was considered but not initiated due to financial constraints and the patient ultimately succumbed to multiorgan failure.
Discussion: This case underscores the diagnostic complexity of GI TMA in renal transplant recipients. It often mimics other GI conditions such as infectious or drug-induced colitis, delaying accurate diagnosis. Maintaining a high index of suspicion for GI-limited TMA in transplant recipients presenting with unexplained gastrointestinal symptoms is important, especially in the context of hematologic abnormalities.
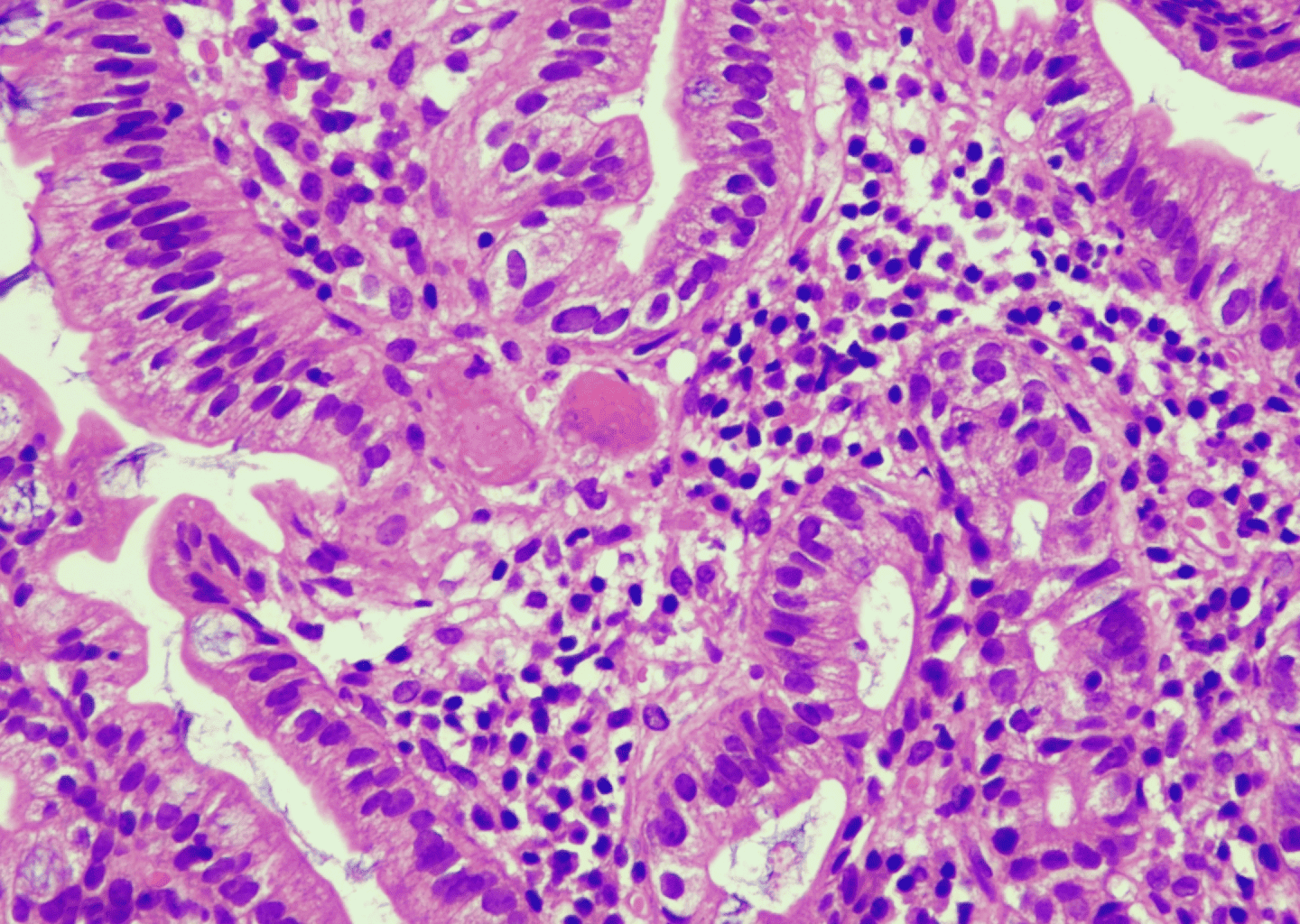
Figure: Duodenal biopsy showing fibrin thrombi obliterating the capillaries. (40x, H&E)
Disclosures:
Prakriti Ramamurthy indicated no relevant financial relationships.
Thanisha Santhosh indicated no relevant financial relationships.
Shivalinga Shekar indicated no relevant financial relationships.
Raj Venugopal indicated no relevant financial relationships.
Pranav Ramamurthy indicated no relevant financial relationships.
Advaith Rao indicated no relevant financial relationships.
Rahul Ravindra indicated no relevant financial relationships.
Vinayak Bhat indicated no relevant financial relationships.
Prakriti Ramamurthy, MBBS, MD1, Thanisha Santhosh, MBBS2, Shivalinga Shekar, MD, DrNB3, Raj Vigna. Venugopal, MBBS, DNB, DM3, Pranav Ramamurthy, MBBS, MD4, Advaith N. Rao, MBBS2, Rahul Ravindra, MBBS, MD5, Vinayak Bhat, 6. P1991 - Gastrointestinal Thrombotic Microangiopathy: A Rare and Potentially Fatal Complication of Renal Transplant, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
