Sunday Poster Session
Category: Small Intestine
P1983 - Benign Bumps, Big Impacts: Exploring Hamartomas in the Gastrointestinal Tract
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Rachel Patel, DO
Lehigh Valley Health Network
Coopersburg, PA
Presenting Author(s)
Rachel Patel, DO1, Salman Ahmed, DO2, Tyler Wark, DO2, Tinsa Varughese, DO2, Corey Savard, MD2, Shashin Shah, MD2
1Lehigh Valley Health Network, Coopersburg, PA; 2Lehigh Valley Health Network, Allentown, PA
Introduction: Hamartomas are benign lesions consistent of disorganized tissue native to the anatomical location. Though typically benign, they can undergo malignant transformation. Common sites of hamartomas include lungs, hypothalamus, and breast. They may cause morbidity by various mechanisms such as infection, infarction, pressure/obstruction, hemorrhage, and neoplastic transformation. Here, we highlight a rare case of Brunner’s gland hamartoma in the gastric antrum of the gastrointestinal tract.
Case Description/
Methods: A 43-year-old obese male with a past medical history of seasonal allergies and prior transverse duodenal mass presented for a follow-up. Three years prior, an endoscopy revealed a mass in the duodenal bulb covering a quarter of the circumference. Partial removal via cold forceps yielded inconclusive biopsies. A recent CT abdomen and pelvis failed to detect the mass. Therefore, the patient underwent a repeat EGD which revealed a large multi-lobulated polyp with a smooth surface and a thick stalk arising from the edge of the pyloric channel. A solution of Everlift and epinephrine was injected to define the stalk and a 20 mm hot snare was used for a complete resection. Purastat solution was applied to the mucosal defect to aid in healing, and one Boston Scientific ultra-clip was placed to prevent bleeding. Pathology confirmed a Brunner’s gland hamartoma.
Discussion: Brunner’s gland hamartomas are rare, benign duodenal tumors, compromising less than 1% of primary gastrointestinal tumors. Their clinical manifestations are often nonspecific, and the exact etiology remains unclear, but may be linked to high gastric acid section, H. pylori infection, chronic pancreatitis, inflammatory stimulation, and mucosal injury. Endoscopic biopsies are frequently negative, given that the mass is often covered by intact mucosa, and their submucosal location makes standard biopsies insufficient for accurate diagnosis. When biopsies are obtained, evaluation for malignant transformation through histology and immunochemistry is essential, especially if the lesion increases in size or exhibits morphological changes. This case highlights the importance of early detection and complete excision of gastrointestinal hamartomas. Addressing the underlying cause remains the cornerstone of effective management.
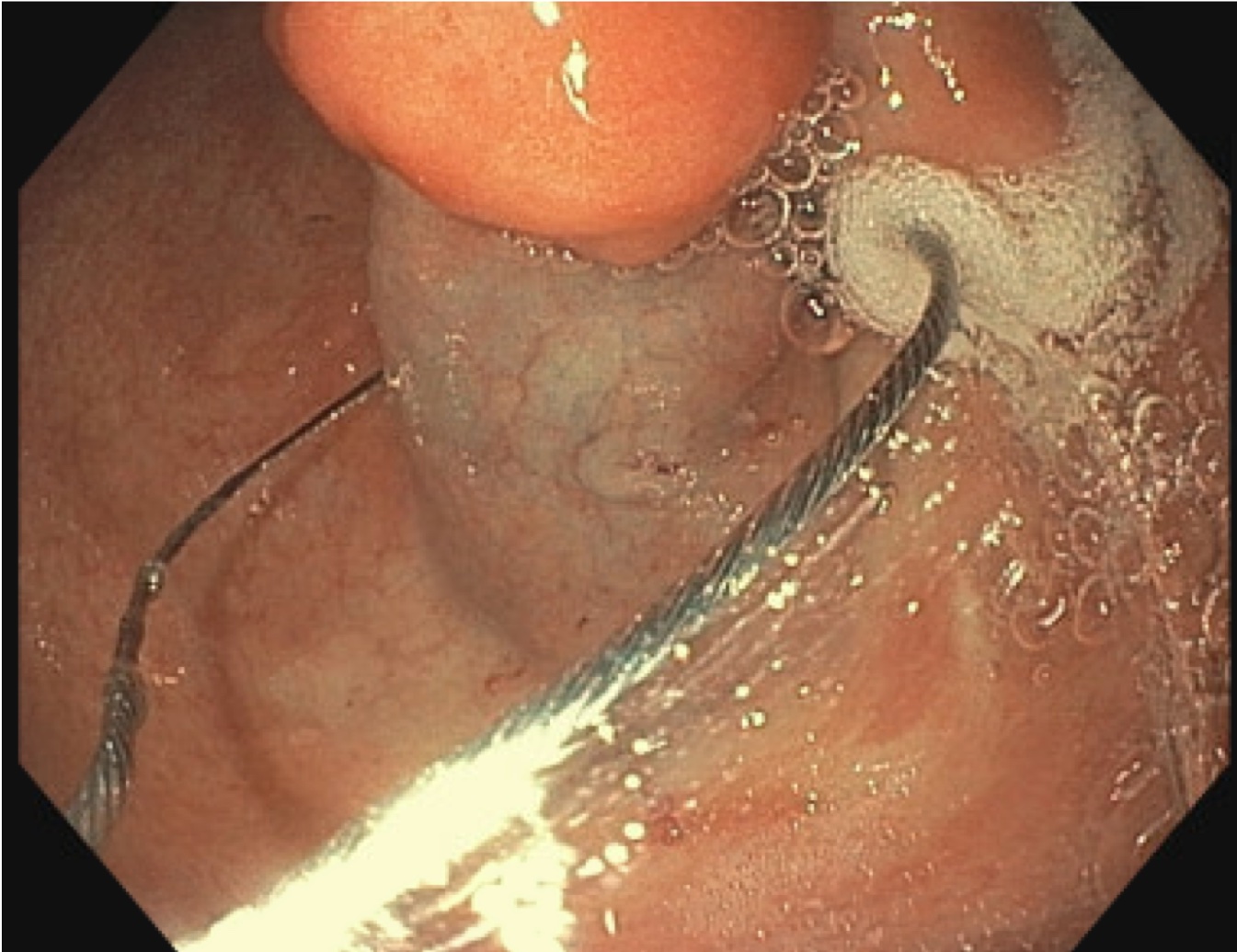
Figure: The antrum of the stomach wall showing a large multi-lobulated polyp with a thick stalk arising from the edge of the pyloric channel. A solution made of 9 parts Everlift and 1 part 1:1000 epinephrine solution was injected into the stalk to define it.
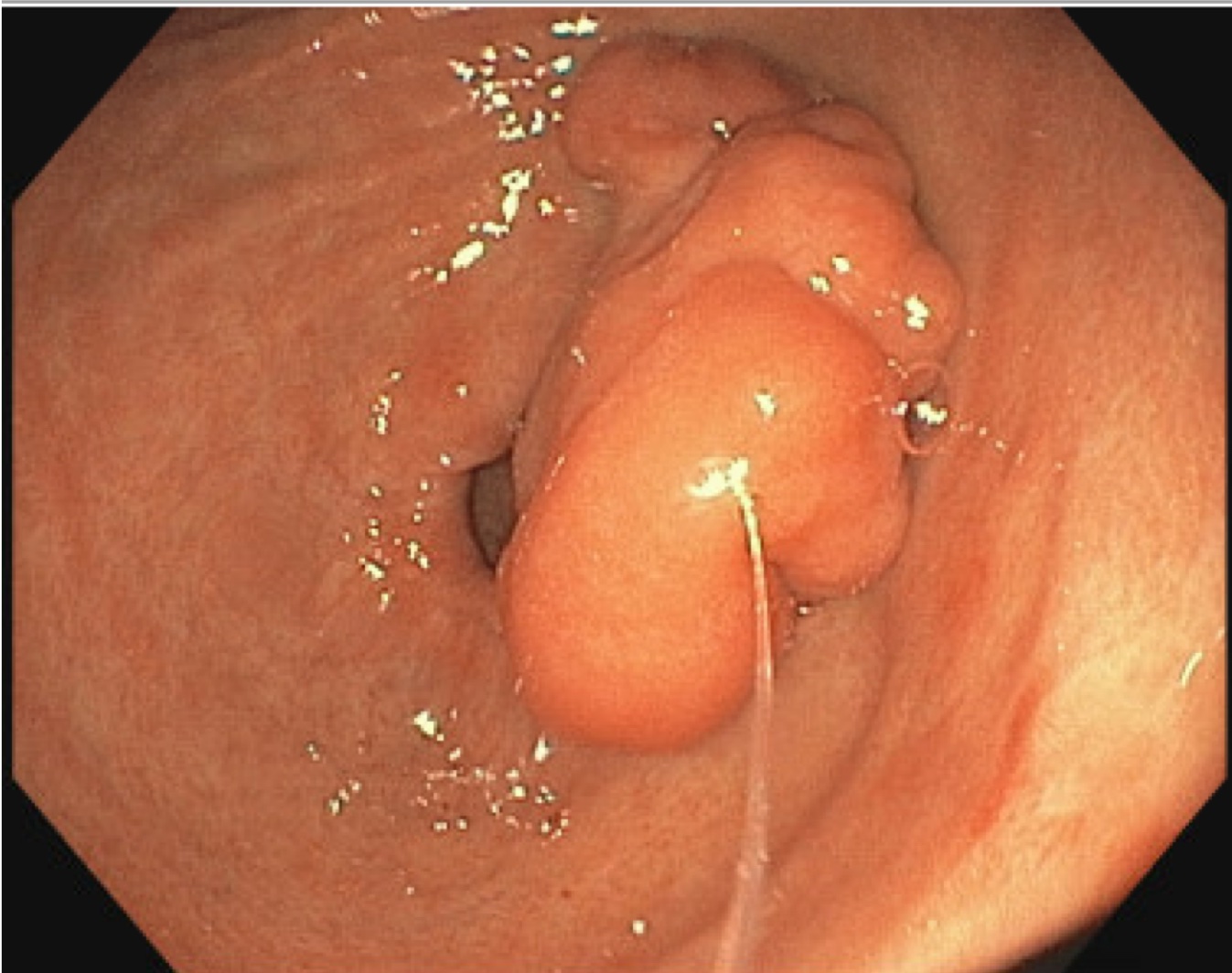
Figure: A 20 mm hot snare was looped around the polyp allowing resection in 1 piece. About 5 mL of Purasat solution was applied to the mucosal defect and a Ultra clip was placed for closure and to prevent bleeding.
Disclosures:
Rachel Patel indicated no relevant financial relationships.
Salman Ahmed indicated no relevant financial relationships.
Tyler Wark indicated no relevant financial relationships.
Tinsa Varughese indicated no relevant financial relationships.
Corey Savard indicated no relevant financial relationships.
Shashin Shah indicated no relevant financial relationships.
Rachel Patel, DO1, Salman Ahmed, DO2, Tyler Wark, DO2, Tinsa Varughese, DO2, Corey Savard, MD2, Shashin Shah, MD2. P1983 - Benign Bumps, Big Impacts: Exploring Hamartomas in the Gastrointestinal Tract, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Lehigh Valley Health Network, Coopersburg, PA; 2Lehigh Valley Health Network, Allentown, PA
Introduction: Hamartomas are benign lesions consistent of disorganized tissue native to the anatomical location. Though typically benign, they can undergo malignant transformation. Common sites of hamartomas include lungs, hypothalamus, and breast. They may cause morbidity by various mechanisms such as infection, infarction, pressure/obstruction, hemorrhage, and neoplastic transformation. Here, we highlight a rare case of Brunner’s gland hamartoma in the gastric antrum of the gastrointestinal tract.
Case Description/
Methods: A 43-year-old obese male with a past medical history of seasonal allergies and prior transverse duodenal mass presented for a follow-up. Three years prior, an endoscopy revealed a mass in the duodenal bulb covering a quarter of the circumference. Partial removal via cold forceps yielded inconclusive biopsies. A recent CT abdomen and pelvis failed to detect the mass. Therefore, the patient underwent a repeat EGD which revealed a large multi-lobulated polyp with a smooth surface and a thick stalk arising from the edge of the pyloric channel. A solution of Everlift and epinephrine was injected to define the stalk and a 20 mm hot snare was used for a complete resection. Purastat solution was applied to the mucosal defect to aid in healing, and one Boston Scientific ultra-clip was placed to prevent bleeding. Pathology confirmed a Brunner’s gland hamartoma.
Discussion: Brunner’s gland hamartomas are rare, benign duodenal tumors, compromising less than 1% of primary gastrointestinal tumors. Their clinical manifestations are often nonspecific, and the exact etiology remains unclear, but may be linked to high gastric acid section, H. pylori infection, chronic pancreatitis, inflammatory stimulation, and mucosal injury. Endoscopic biopsies are frequently negative, given that the mass is often covered by intact mucosa, and their submucosal location makes standard biopsies insufficient for accurate diagnosis. When biopsies are obtained, evaluation for malignant transformation through histology and immunochemistry is essential, especially if the lesion increases in size or exhibits morphological changes. This case highlights the importance of early detection and complete excision of gastrointestinal hamartomas. Addressing the underlying cause remains the cornerstone of effective management.
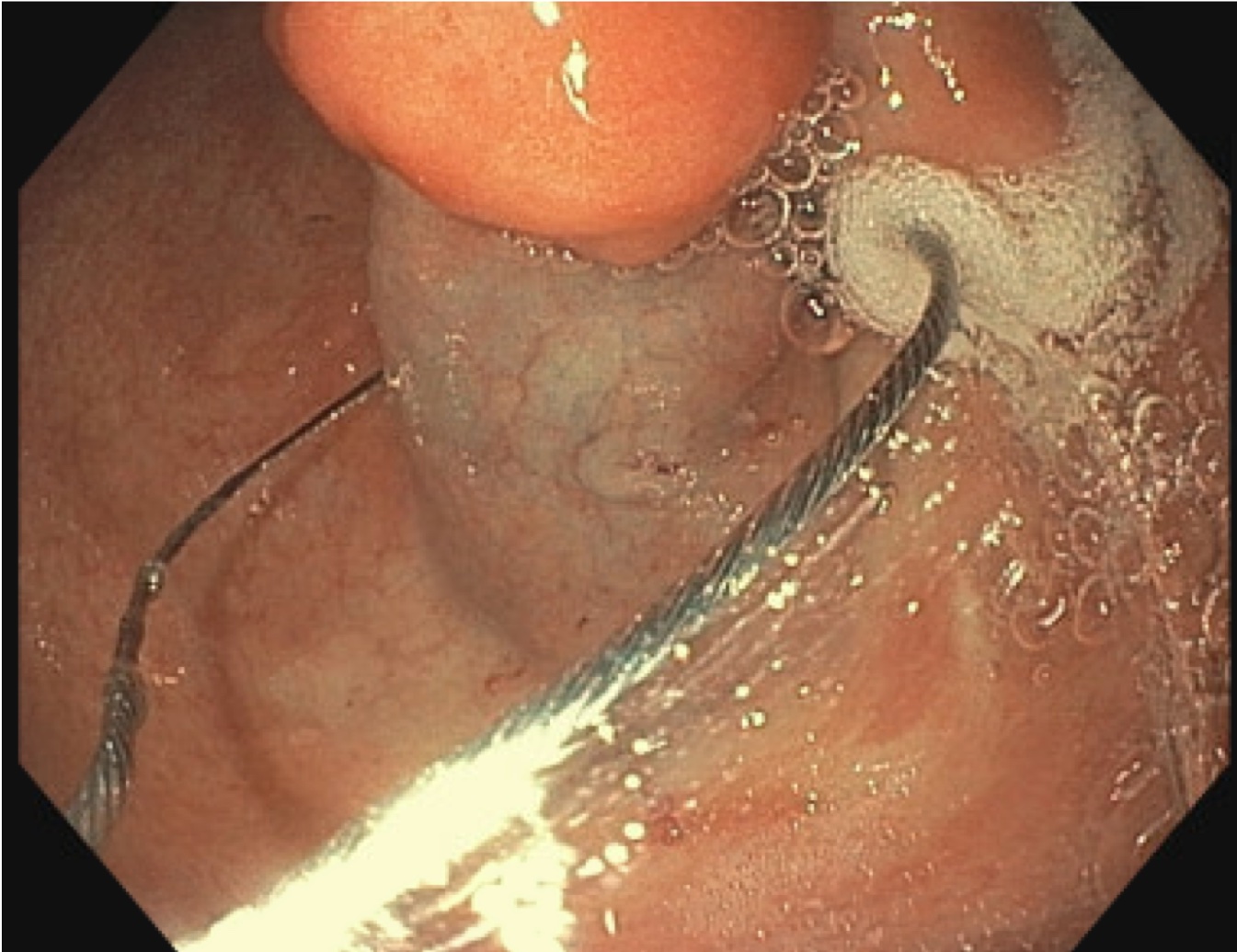
Figure: The antrum of the stomach wall showing a large multi-lobulated polyp with a thick stalk arising from the edge of the pyloric channel. A solution made of 9 parts Everlift and 1 part 1:1000 epinephrine solution was injected into the stalk to define it.
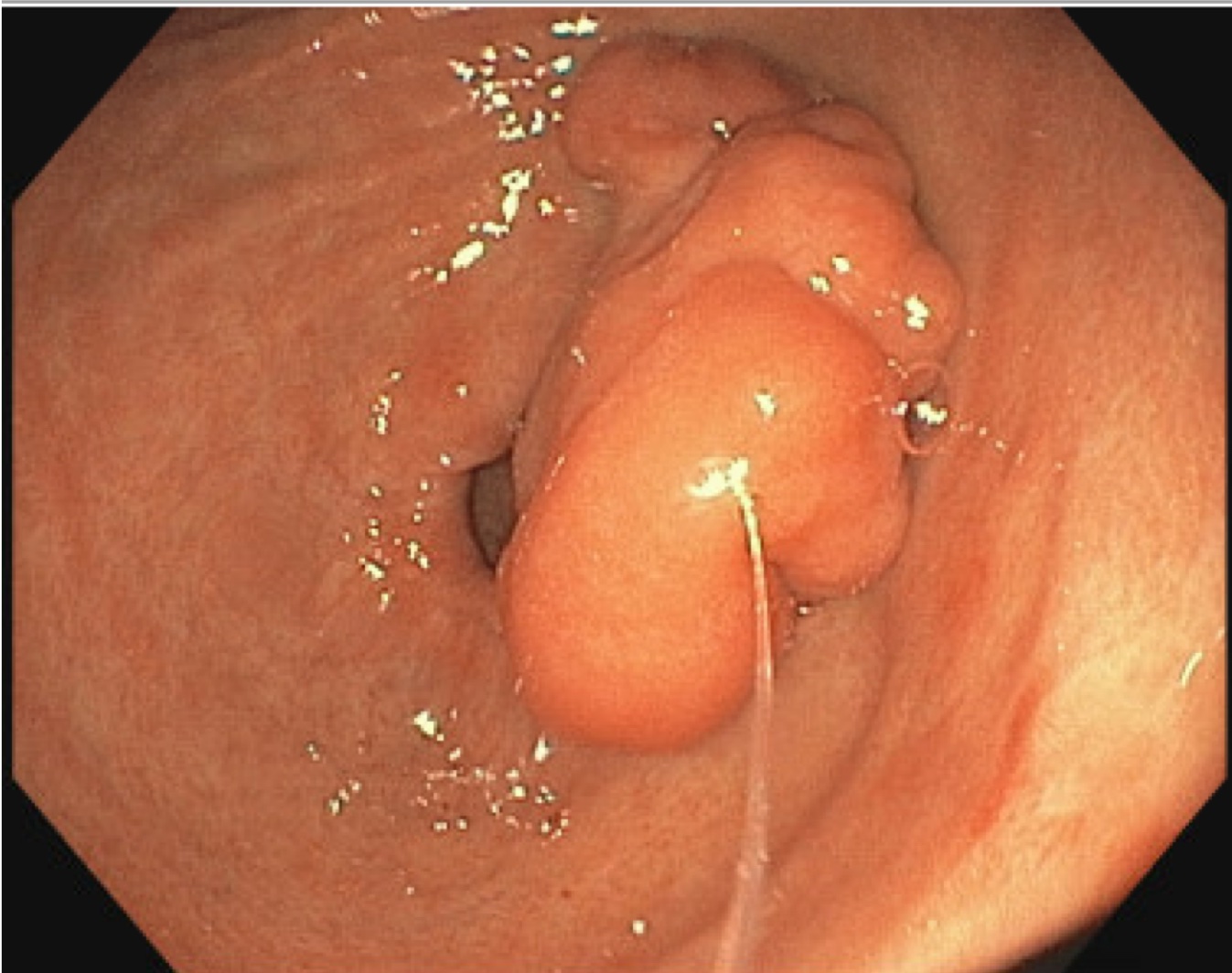
Figure: A 20 mm hot snare was looped around the polyp allowing resection in 1 piece. About 5 mL of Purasat solution was applied to the mucosal defect and a Ultra clip was placed for closure and to prevent bleeding.
Disclosures:
Rachel Patel indicated no relevant financial relationships.
Salman Ahmed indicated no relevant financial relationships.
Tyler Wark indicated no relevant financial relationships.
Tinsa Varughese indicated no relevant financial relationships.
Corey Savard indicated no relevant financial relationships.
Shashin Shah indicated no relevant financial relationships.
Rachel Patel, DO1, Salman Ahmed, DO2, Tyler Wark, DO2, Tinsa Varughese, DO2, Corey Savard, MD2, Shashin Shah, MD2. P1983 - Benign Bumps, Big Impacts: Exploring Hamartomas in the Gastrointestinal Tract, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

