Sunday Poster Session
Category: Small Intestine
P1933 - Five-Year Trends in Hemostasis Following Non-Ampullary Duodenal Endoscopic Mucosal Resection
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- KG
Kanika Garg, MD
Rush University Medical Center
Chicago, IL
Presenting Author(s)
Kanika Garg, MD, Thomas J. Wang, MD, Christopher G. Chapman, MD, Ajaypal Singh, MD, Irving Waxman, MD, FACG, Neal A. Mehta, MD
Rush University Medical Center, Chicago, IL
Introduction: Duodenal adenomas have malignant potential and thus are often treated with endoscopic mucosal resection (EMR). The duodenum's thin wall, increased vascularity, and retroperitoneal position pose technical challenges and elevate procedural risks, particularly bleeding and perforation. Novel hemostatic applications have been developed to mitigate these risks. We evaluated post-resection hemostatic trends in non-ampullary duodenal adenomas over 5 years.
Methods: This is a single-center retrospective cohort study of adults undergoing EMR of non-ampullary duodenal adenomas from 2019 to 2024. Primary outcomes were hemostatic intervention trends and delayed bleeding rates. Enhanced hemostatic strategy was defined as the use of specialized defect closure clips, hemostatic powder/gel, or combination approaches beyond standard clips alone. Secondary analysis compared polyp characteristics between bleeding groups using Mann-Whitney U test.
Results: 46 patients were included (43.5% male, median age 69±9.4 years). Median polyp size was 19mm [7-60mm]; 31 (67.4%) were sessile and 25 (54.3%) were located in the second part of the duodenum. EMR success was 93.5% with 50% en bloc resection. Enhanced hemostatic strategies were employed in 20 cases (43.5%): hemostatic gel (n=7), hemostatic spray (n=9), defect closure clips (n=6), or combination thereof. Standard clips alone were used in 26 cases (56.5%). Intraprocedural bleeding occurred in 25 cases (54.3%) but all were successfully managed during the index procedure. Delayed bleeding occurred in 4 patients (8.7%). Initial hemostasis included: standard clips alone (n=2), standard clips plus hemostatic gel (n=1), and hemostatic spray alone (n=1). Of these, three were managed endoscopically while one required interventional radiology-guided embolization. Polyp size was significantly larger in delayed bleeding cases (median 35mm vs 15.5mm, p< 0.01).
Discussion: Enhanced hemostatic interventions showed increasing adoption over five years, used in 43.5% of duodenal EMRs at our center, potentially contributing to a low delayed bleeding rate. When delayed bleeding occurred, the polyps were among the largest resected and advanced hemostatic interventions were not utilized in 50% of cases. These findings suggest that multimodal hemostatic approaches may improve safety outcomes for duodenal EMR, particularly for larger lesions. Future studies are needed to evaluate whether the combination of multiple hemostatic modalities reduces the risk of delayed bleeding post-EMR.
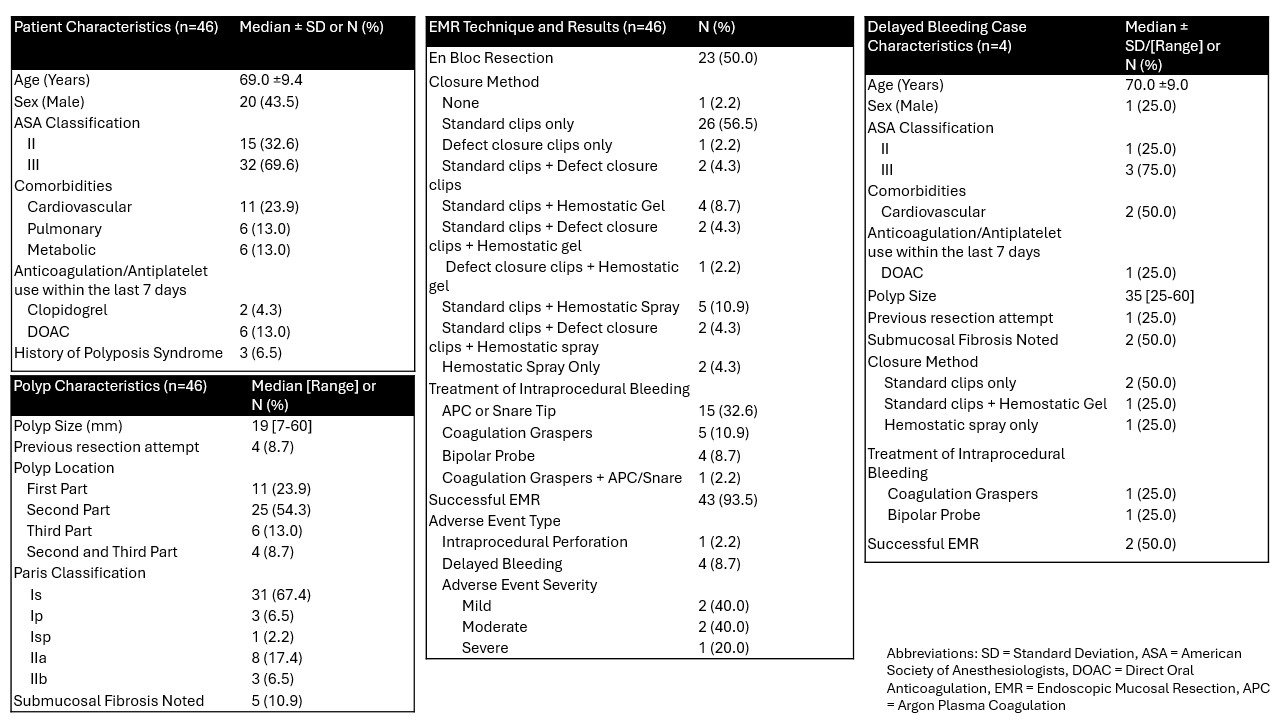
Figure: Figure 1. Summary of patient, polyp, and procedural factors and their association with outcomes following duodenal polyp endoscopic mucosal resection.
Disclosures:
Kanika Garg indicated no relevant financial relationships.
Thomas Wang indicated no relevant financial relationships.
Christopher Chapman: Boston Scientific – Consultant. Olympus – Consultant. Phathom Pharmaceuticals – Consultant.
Ajaypal Singh: Boston Scientific – Consultant. Creo – Consultant. Olympus – Consultant.
Irving Waxman: Boston Scientific – Consultant. Cook Medical – Consultant. Medtronic – Consultant.
Neal Mehta: Boston Scientific – Consultant. Castle Biosciences – Consultant. ConMed – Consultant. Medtronic – Consultant. Olympus – Consultant.
Kanika Garg, MD, Thomas J. Wang, MD, Christopher G. Chapman, MD, Ajaypal Singh, MD, Irving Waxman, MD, FACG, Neal A. Mehta, MD. P1933 - Five-Year Trends in Hemostasis Following Non-Ampullary Duodenal Endoscopic Mucosal Resection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Rush University Medical Center, Chicago, IL
Introduction: Duodenal adenomas have malignant potential and thus are often treated with endoscopic mucosal resection (EMR). The duodenum's thin wall, increased vascularity, and retroperitoneal position pose technical challenges and elevate procedural risks, particularly bleeding and perforation. Novel hemostatic applications have been developed to mitigate these risks. We evaluated post-resection hemostatic trends in non-ampullary duodenal adenomas over 5 years.
Methods: This is a single-center retrospective cohort study of adults undergoing EMR of non-ampullary duodenal adenomas from 2019 to 2024. Primary outcomes were hemostatic intervention trends and delayed bleeding rates. Enhanced hemostatic strategy was defined as the use of specialized defect closure clips, hemostatic powder/gel, or combination approaches beyond standard clips alone. Secondary analysis compared polyp characteristics between bleeding groups using Mann-Whitney U test.
Results: 46 patients were included (43.5% male, median age 69±9.4 years). Median polyp size was 19mm [7-60mm]; 31 (67.4%) were sessile and 25 (54.3%) were located in the second part of the duodenum. EMR success was 93.5% with 50% en bloc resection. Enhanced hemostatic strategies were employed in 20 cases (43.5%): hemostatic gel (n=7), hemostatic spray (n=9), defect closure clips (n=6), or combination thereof. Standard clips alone were used in 26 cases (56.5%). Intraprocedural bleeding occurred in 25 cases (54.3%) but all were successfully managed during the index procedure. Delayed bleeding occurred in 4 patients (8.7%). Initial hemostasis included: standard clips alone (n=2), standard clips plus hemostatic gel (n=1), and hemostatic spray alone (n=1). Of these, three were managed endoscopically while one required interventional radiology-guided embolization. Polyp size was significantly larger in delayed bleeding cases (median 35mm vs 15.5mm, p< 0.01).
Discussion: Enhanced hemostatic interventions showed increasing adoption over five years, used in 43.5% of duodenal EMRs at our center, potentially contributing to a low delayed bleeding rate. When delayed bleeding occurred, the polyps were among the largest resected and advanced hemostatic interventions were not utilized in 50% of cases. These findings suggest that multimodal hemostatic approaches may improve safety outcomes for duodenal EMR, particularly for larger lesions. Future studies are needed to evaluate whether the combination of multiple hemostatic modalities reduces the risk of delayed bleeding post-EMR.
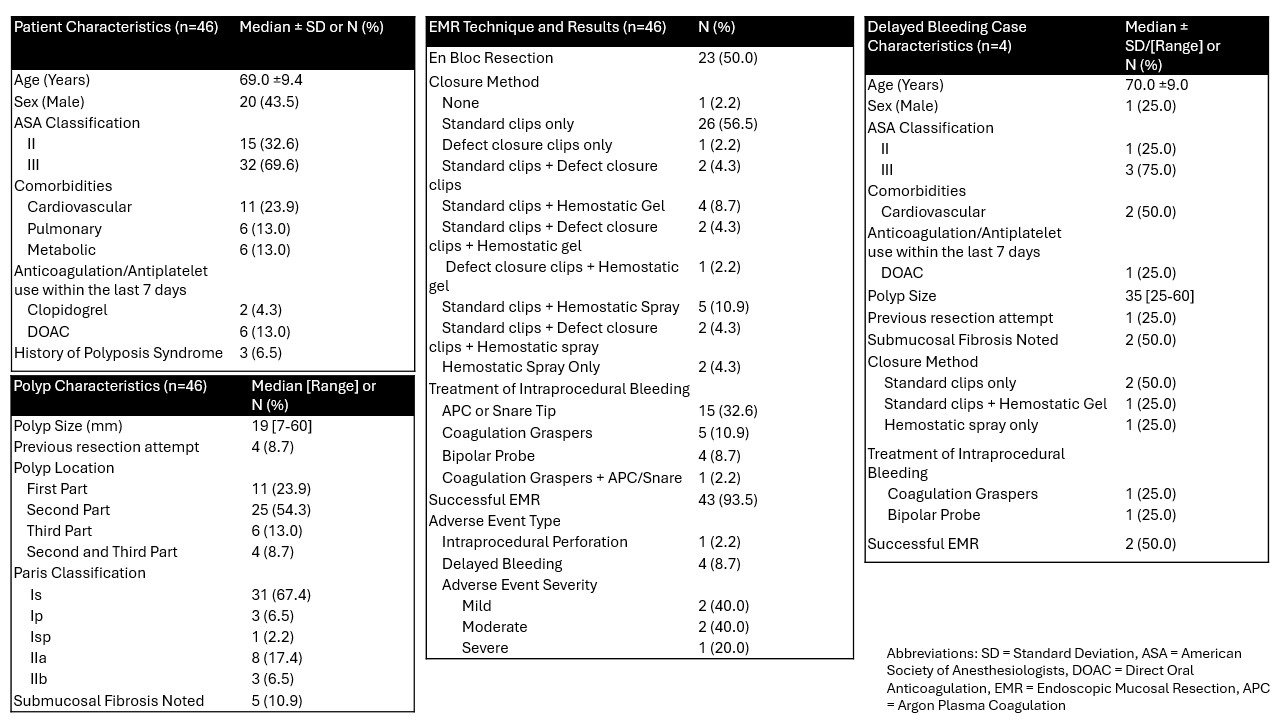
Figure: Figure 1. Summary of patient, polyp, and procedural factors and their association with outcomes following duodenal polyp endoscopic mucosal resection.
Disclosures:
Kanika Garg indicated no relevant financial relationships.
Thomas Wang indicated no relevant financial relationships.
Christopher Chapman: Boston Scientific – Consultant. Olympus – Consultant. Phathom Pharmaceuticals – Consultant.
Ajaypal Singh: Boston Scientific – Consultant. Creo – Consultant. Olympus – Consultant.
Irving Waxman: Boston Scientific – Consultant. Cook Medical – Consultant. Medtronic – Consultant.
Neal Mehta: Boston Scientific – Consultant. Castle Biosciences – Consultant. ConMed – Consultant. Medtronic – Consultant. Olympus – Consultant.
Kanika Garg, MD, Thomas J. Wang, MD, Christopher G. Chapman, MD, Ajaypal Singh, MD, Irving Waxman, MD, FACG, Neal A. Mehta, MD. P1933 - Five-Year Trends in Hemostasis Following Non-Ampullary Duodenal Endoscopic Mucosal Resection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
