Sunday Poster Session
Category: Practice Management
P1930 - Virtual Multidisciplinary GI Clinic Improves Outcomes in Medicare-Aged Patients With Gastrointestinal Conditions
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- SB
Sameer Berry, MD
NYU Langone Health
New York, NY
Presenting Author(s)
Sameer Berry, MD1, Sanskriti Varma, MD2, Chamara Basnayake, MBBS3, Jeffrey Berinstein, MD, MS4, Walter Chan, MD, MPH, FACG5, John Allen, MD, MBA4, William Chey, MD, FACG4
1NYU Langone Health, New York, NY; 2Massachusetts General Hospital, Somerville, MA; 3St Vincent’s Hospital Melbourne – Department of Gastroenterology, Melbourne, Victoria, Australia; 4University of Michigan Health, Ann Arbor, MI; 5Brigham and Women's Hospital, Boston, MA
Introduction: Gastrointestinal (GI) disorders are highly prevalent in adults aged 65 and older, affecting more than half of the Medicare population and contributing to significant healthcare costs. This population faces unique care challenges, including increased symptom burden, higher complication rates, and frequent reliance on emergency services and advanced diagnostics. We evaluated the impact of a virtual multidisciplinary GI clinic on patient engagement and clinical outcomes in Medicare-aged adults.
Methods: In this prospective observational study, adults aged ≥65 years and insured by a national commercial health plan were enrolled in a virtual GI clinic between March 2021 and May 2025. Patients receiving ≥1 year of care were included in descriptive analyses of clinical engagement. All patients completed ≥4 clinical visits and provided self-reported outcomes at baseline and after the most recent visit, including symptom severity (of any GI-related symptom), global symptom control, and satisfaction. Paired pre-post comparisons were made using McNemar’s Chi-square tests.
Results: Of 356 enrolled clinic patients, 209 (59%) were female with a mean age of 68.8±4.6 years. The most common diagnoses were disorders of gut brain interaction (54%) and esophageal diseases (43%), with new GI diagnoses made in 30% (Table 1). Enrolled patients completed a mean of 7 visits (range: 2-48) and exchanged a mean of 44 messages (range: 3-792) with the care team. Most patients received care from dietitians (92%) and GI psychologists (47%) as part of the multidisciplinary team. Significant improvements were observed in symptom severity (n=184; 23% moderate-to-severe post-care vs. 72% at baseline; p< 0.0001), global symptom control (n=200; 95% post-care vs. 18% baseline; p< 0.0001), and satisfaction with care (n=115; 100% satisfied post-care vs. 44% baseline; p< 0.0001, Table 2).
Discussion: This virtual multidisciplinary GI care model was associated with frequent clinical engagement and significant improvements in patient-reported outcomes among Medicare-aged adults. These findings support the feasibility and clinical effectiveness of virtual integrated GI care in older adults, a population often underserved in traditional care models.
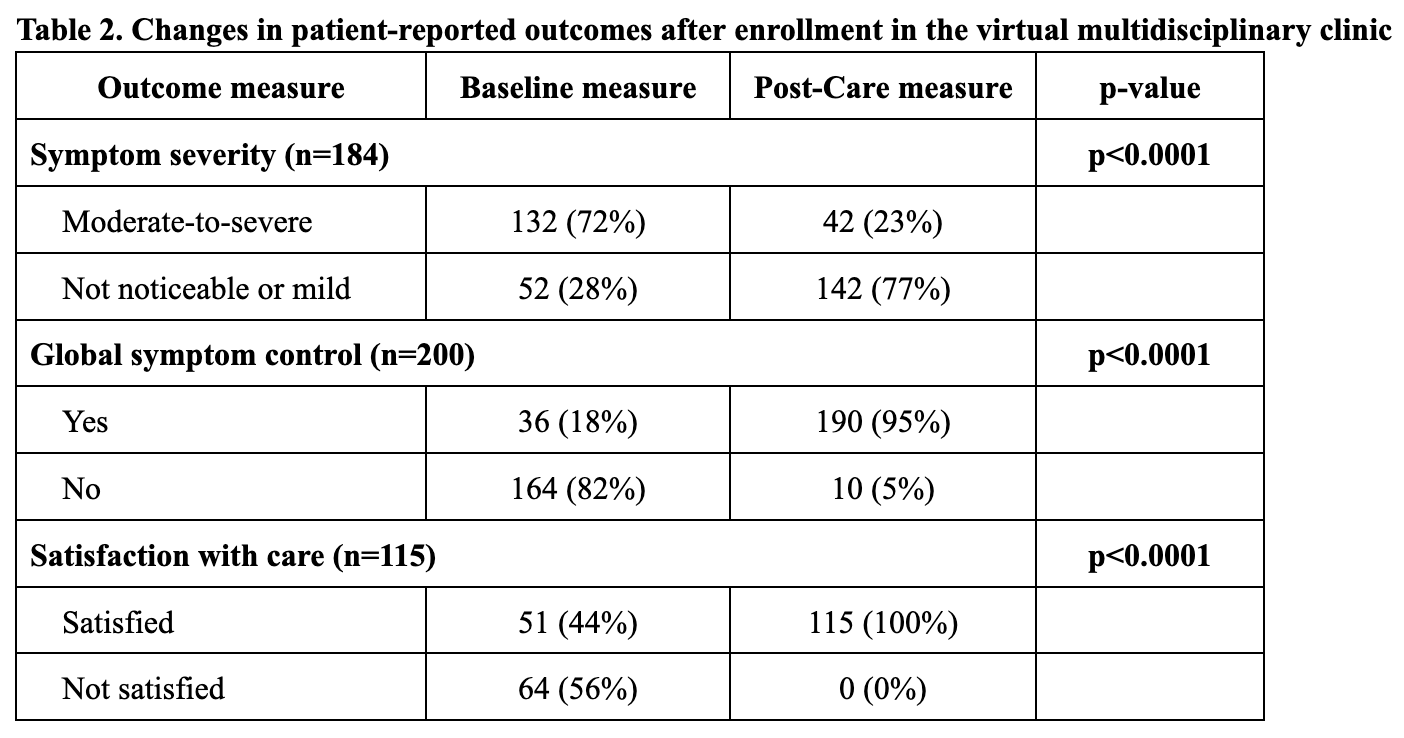
Figure: Values shown as N (%) or mean (standard deviation) for patients with documented diagnoses. Patients can have more than one condition and be classified multiple times. Diagnosis data is reflective of members who remained engaged in the clinic for at least 1 year.
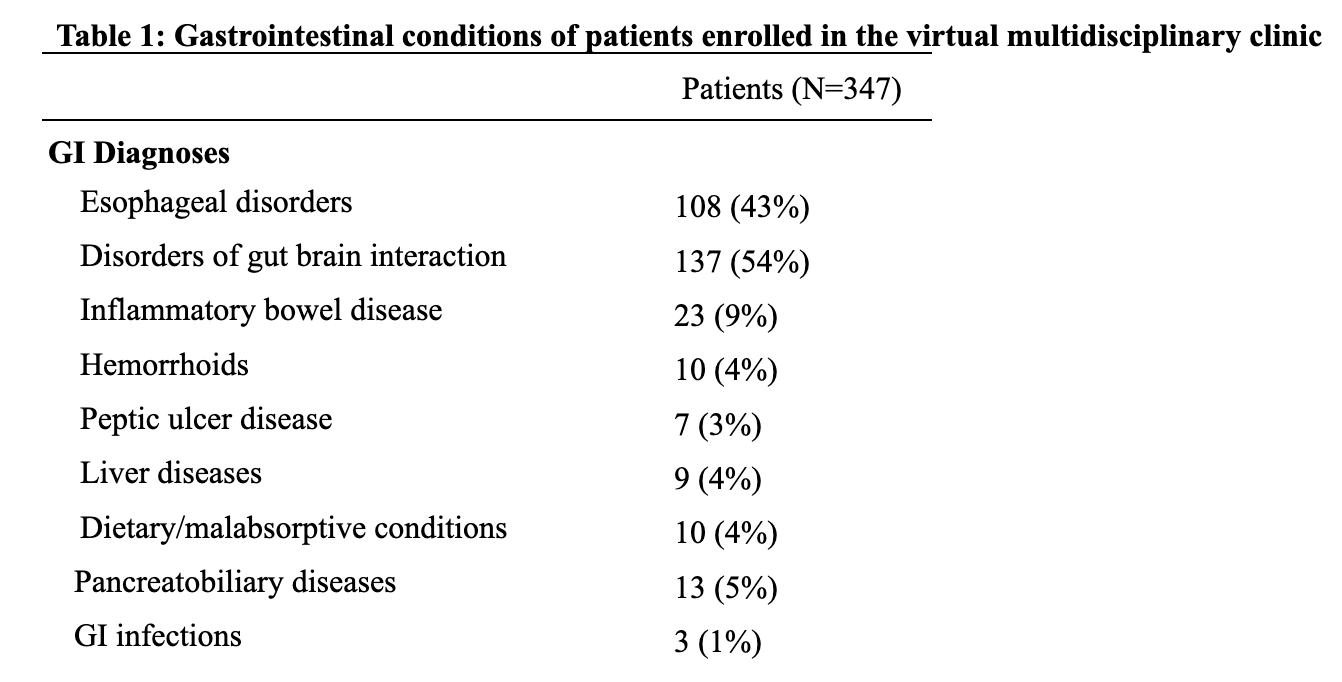
Figure: Symptom severity was assessed using a non-validated clinical questionnaire developed by Oshi Health for internal clinical use, and measured in the following categories: not noticeable, mild, moderate, severe. For the purposes of analyses, responses were grouped into “moderate/severe” or “not noticeable/mild”.
Global symptom control was assessed using a non-validated clinical questionnaire developed by Oshi Health for internal clinical use and measured in the following categories: yes, no.
Satisfaction with care was measured using the validated Customer Satisfaction Survey in the following categories: very dissatisfied, dissatisfied, neutral, satisfied, very satisfied. For the purposes of analyses, responses were grouped into “satisfied” if patients reported “satisfied” or “very satisfied” and “not satisfied” if patients reported “neutral”, “dissatisfied”, or “very dissatisfied”.
Disclosures:
Sameer Berry: Oshi Health – Employee.
Sanskriti Varma: Oshi Health – Consultant.
Chamara Basnayake indicated no relevant financial relationships.
Jeffrey Berinstein indicated no relevant financial relationships.
Walter Chan indicated no relevant financial relationships.
John Allen indicated no relevant financial relationships.
William Chey: Ardelyx – Consultant. Atmo – Consultant. Biomerica – Consultant. Commonwealth Diagnostics International – Grant/Research Support. Coprata – Stock Options. Dieta – Stock Options. Digital Manometry – Intellectual Property/Patents. Evinature – Stock Options. FoodMarble – Stock Options. Gemelli – Consultant. Kiwi BioScience – Stock Options. Modify Health – Stock Options. My Nutrition Health – Intellectual Property/Patents. Phathom – Consultant. Rectal Expulsion Device – Intellectual Property/Patents. Redhill – Consultant. Salix – Consultant, Grant/Research Support. Takeda – Consultant. Vibrant – Consultant.
Sameer Berry, MD1, Sanskriti Varma, MD2, Chamara Basnayake, MBBS3, Jeffrey Berinstein, MD, MS4, Walter Chan, MD, MPH, FACG5, John Allen, MD, MBA4, William Chey, MD, FACG4. P1930 - Virtual Multidisciplinary GI Clinic Improves Outcomes in Medicare-Aged Patients With Gastrointestinal Conditions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NYU Langone Health, New York, NY; 2Massachusetts General Hospital, Somerville, MA; 3St Vincent’s Hospital Melbourne – Department of Gastroenterology, Melbourne, Victoria, Australia; 4University of Michigan Health, Ann Arbor, MI; 5Brigham and Women's Hospital, Boston, MA
Introduction: Gastrointestinal (GI) disorders are highly prevalent in adults aged 65 and older, affecting more than half of the Medicare population and contributing to significant healthcare costs. This population faces unique care challenges, including increased symptom burden, higher complication rates, and frequent reliance on emergency services and advanced diagnostics. We evaluated the impact of a virtual multidisciplinary GI clinic on patient engagement and clinical outcomes in Medicare-aged adults.
Methods: In this prospective observational study, adults aged ≥65 years and insured by a national commercial health plan were enrolled in a virtual GI clinic between March 2021 and May 2025. Patients receiving ≥1 year of care were included in descriptive analyses of clinical engagement. All patients completed ≥4 clinical visits and provided self-reported outcomes at baseline and after the most recent visit, including symptom severity (of any GI-related symptom), global symptom control, and satisfaction. Paired pre-post comparisons were made using McNemar’s Chi-square tests.
Results: Of 356 enrolled clinic patients, 209 (59%) were female with a mean age of 68.8±4.6 years. The most common diagnoses were disorders of gut brain interaction (54%) and esophageal diseases (43%), with new GI diagnoses made in 30% (Table 1). Enrolled patients completed a mean of 7 visits (range: 2-48) and exchanged a mean of 44 messages (range: 3-792) with the care team. Most patients received care from dietitians (92%) and GI psychologists (47%) as part of the multidisciplinary team. Significant improvements were observed in symptom severity (n=184; 23% moderate-to-severe post-care vs. 72% at baseline; p< 0.0001), global symptom control (n=200; 95% post-care vs. 18% baseline; p< 0.0001), and satisfaction with care (n=115; 100% satisfied post-care vs. 44% baseline; p< 0.0001, Table 2).
Discussion: This virtual multidisciplinary GI care model was associated with frequent clinical engagement and significant improvements in patient-reported outcomes among Medicare-aged adults. These findings support the feasibility and clinical effectiveness of virtual integrated GI care in older adults, a population often underserved in traditional care models.
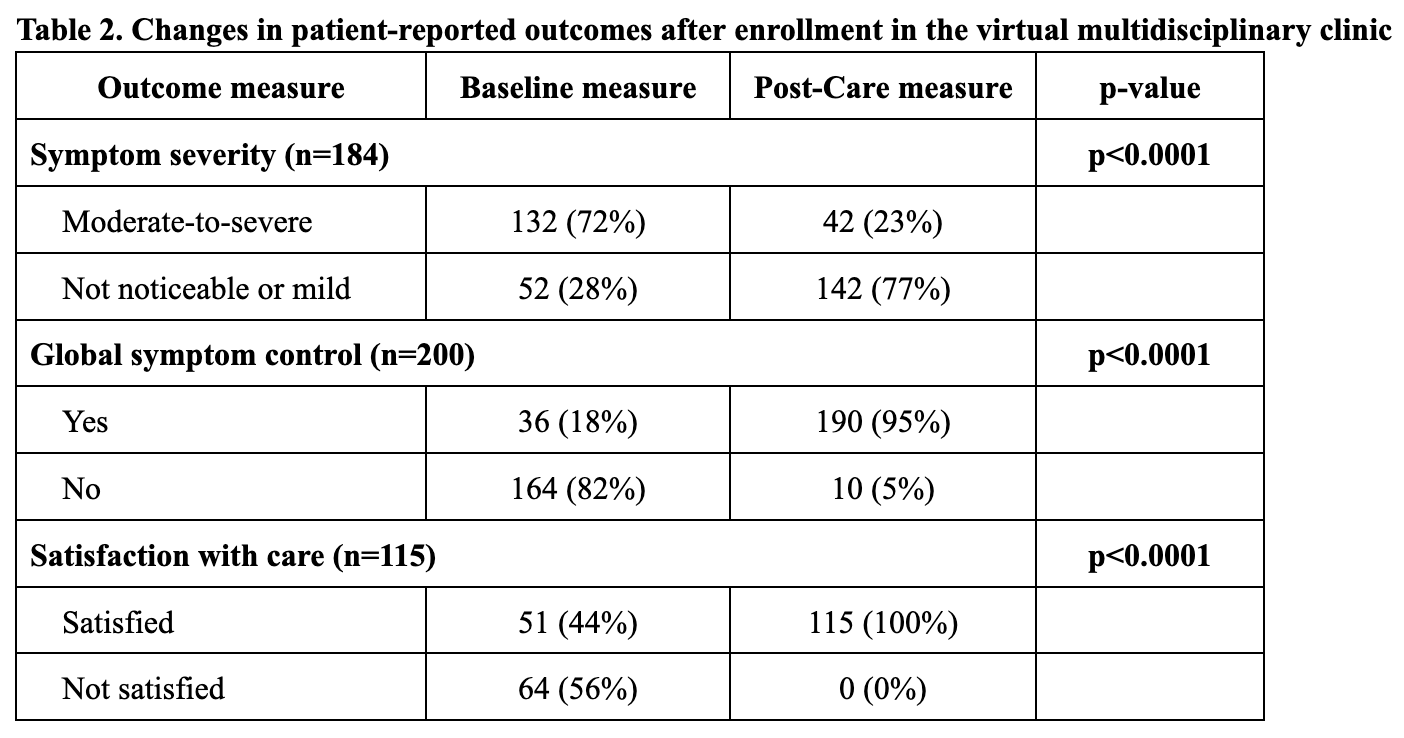
Figure: Values shown as N (%) or mean (standard deviation) for patients with documented diagnoses. Patients can have more than one condition and be classified multiple times. Diagnosis data is reflective of members who remained engaged in the clinic for at least 1 year.
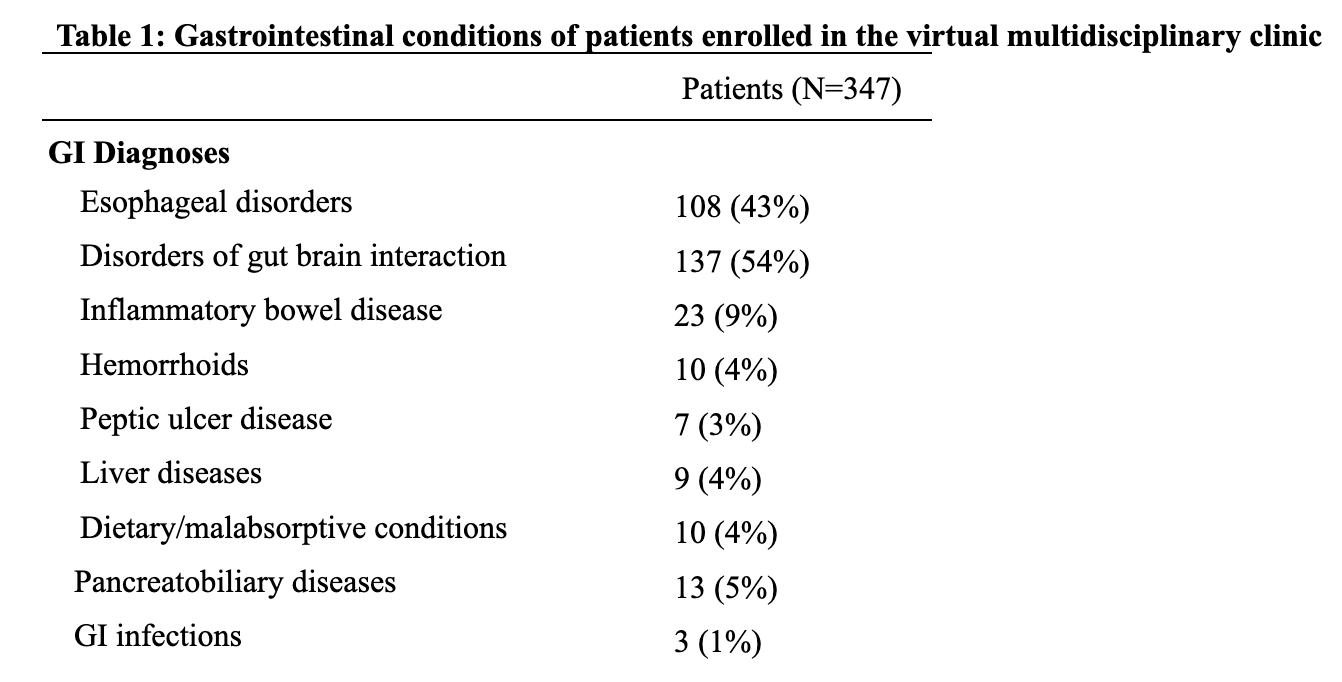
Figure: Symptom severity was assessed using a non-validated clinical questionnaire developed by Oshi Health for internal clinical use, and measured in the following categories: not noticeable, mild, moderate, severe. For the purposes of analyses, responses were grouped into “moderate/severe” or “not noticeable/mild”.
Global symptom control was assessed using a non-validated clinical questionnaire developed by Oshi Health for internal clinical use and measured in the following categories: yes, no.
Satisfaction with care was measured using the validated Customer Satisfaction Survey in the following categories: very dissatisfied, dissatisfied, neutral, satisfied, very satisfied. For the purposes of analyses, responses were grouped into “satisfied” if patients reported “satisfied” or “very satisfied” and “not satisfied” if patients reported “neutral”, “dissatisfied”, or “very dissatisfied”.
Disclosures:
Sameer Berry: Oshi Health – Employee.
Sanskriti Varma: Oshi Health – Consultant.
Chamara Basnayake indicated no relevant financial relationships.
Jeffrey Berinstein indicated no relevant financial relationships.
Walter Chan indicated no relevant financial relationships.
John Allen indicated no relevant financial relationships.
William Chey: Ardelyx – Consultant. Atmo – Consultant. Biomerica – Consultant. Commonwealth Diagnostics International – Grant/Research Support. Coprata – Stock Options. Dieta – Stock Options. Digital Manometry – Intellectual Property/Patents. Evinature – Stock Options. FoodMarble – Stock Options. Gemelli – Consultant. Kiwi BioScience – Stock Options. Modify Health – Stock Options. My Nutrition Health – Intellectual Property/Patents. Phathom – Consultant. Rectal Expulsion Device – Intellectual Property/Patents. Redhill – Consultant. Salix – Consultant, Grant/Research Support. Takeda – Consultant. Vibrant – Consultant.
Sameer Berry, MD1, Sanskriti Varma, MD2, Chamara Basnayake, MBBS3, Jeffrey Berinstein, MD, MS4, Walter Chan, MD, MPH, FACG5, John Allen, MD, MBA4, William Chey, MD, FACG4. P1930 - Virtual Multidisciplinary GI Clinic Improves Outcomes in Medicare-Aged Patients With Gastrointestinal Conditions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

