Sunday Poster Session
Category: Practice Management
P1922 - Beyond the Endoscopy Suite: A Survey-Based Study of Microaggressions and Workplace Bias in Gastroenterology
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Chioma Owo, MD
University of Texas Health San Antonio
San Antonio, TX
Presenting Author(s)
Chioma Owo, MD1, Lavanya Viswanathan, MD, MS, FACG2
1University of Texas Health San Antonio, San Antonio, TX; 2UT MD Anderson Cancer Center, Houston, TX
Introduction: Gender- and race-based disparities persist in gastroenterology (GI), despite growing awareness of inequities in medicine. Women and underrepresented minorities (URMs) frequently face microaggressions, role misidentification, exclusion from advancement, and institutional inaction. Though awareness has grown, these experiences remain underreported. Under the ACG Summer Scholars Program, this study was developed to explore the impact of these challenges. We hypothesize that microaggressions are highly prevalent among women in GI, contributing to adverse emotional, professional, and institutional outcomes—particularly in clinical and educational settings—and that these experiences vary by age and practice setting.
Methods: An anonymous 33-question cross-sectional survey was distributed through GI-focused networks. It assessed demographics, familiarity with microaggressions, personal and witnessed experiences, perceived causes, responses, and institutional support. Quantitative data were analyzed descriptively, with subgroup comparisons by age (≤44 vs >44) and setting (academic vs private). Qualitative data underwent thematic analysis.
Results: Fifty-nine respondents—all women—completed the survey. Most were aged 35–44 (54%), mid-career (41%), and in academic (32%) or private (39%) practice. Overall, 92% reported experiencing microaggressions, mostly in clinical (89%) and admin (66%) settings. Perpetrators included patients (62.3%), senior GIs (54.7%), nurses (58.5%), and supervisors (41.5%). Microaggressions were verbal (83.3%) or non-verbal (77.8%) and attributed to gender (97.2%), age (63.9%), and race (38.9%).
Younger respondents (< 45) reported more frequent, emotionally distressing experiences, including burnout and imposter syndrome. Those in private practice cited more patient-driven incidents; those in academia cited more peer- and trainee-related events. Only 41.7% felt moderately comfortable addressing bias. Of those who responded, 38.9% faced retaliation, exclusion, or poor evaluations. Only 14% had access to effective reporting systems.
Discussion: Microaggressions are pervasive in GI, particularly among women and younger professionals. Experiences vary by setting and age, often leading to emotional distress and professional isolation. Despite institutional diversity efforts, support systems remain inadequate. Addressing this gap requires leadership accountability, inclusive mentorship, responsive reporting structures, and a culture that empowers individuals to speak up safely.
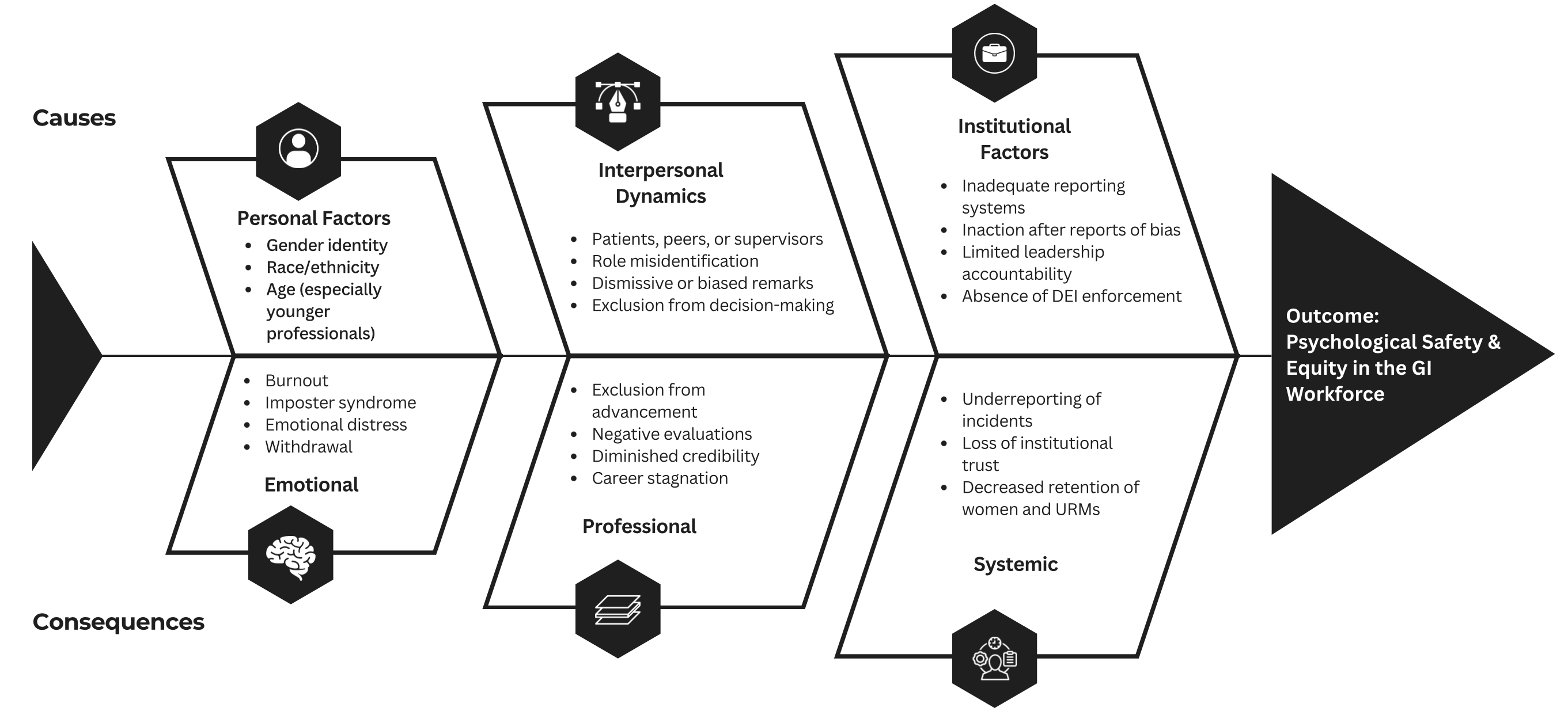
Figure: Figure 1. "Microaggressions in Gastroenterology: Drivers and Consequences"
Fishbone diagram illustrating the perceived causes and reported impacts of microaggressions experienced by women in gastroenterology based on survey responses.
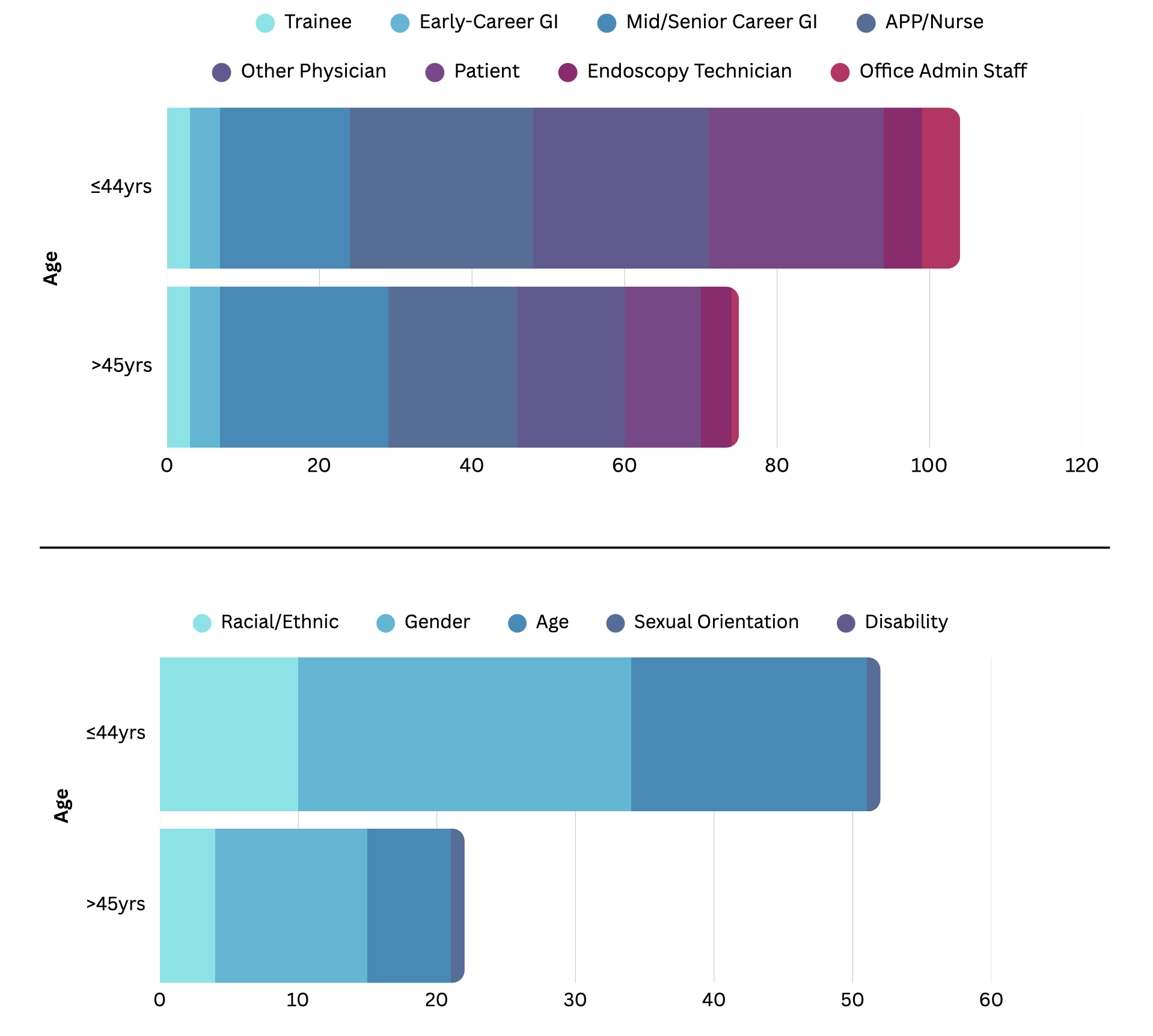
Figure: Figure 2. Age-stratified patterns of microaggressions reported by women in GI.
Top: "Perpetrators of Microaggressions by Age Group"
Perpetrators of microaggressions by age group, with respondents aged ≤44 more frequently identifying patients, nurses, and senior colleagues.
Bottom: "Types of Microaggressions Reported by Age Group"
Types of microaggressions reported by age group, with younger respondents more likely to report gender- and age-related bias.
Disclosures:
Chioma Owo indicated no relevant financial relationships.
Lavanya Viswanathan: Ardelyx, Inc. – Advisor or Review Panel Member, The above are unpaid., Speakers Bureau.
Chioma Owo, MD1, Lavanya Viswanathan, MD, MS, FACG2. P1922 - Beyond the Endoscopy Suite: A Survey-Based Study of Microaggressions and Workplace Bias in Gastroenterology, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas Health San Antonio, San Antonio, TX; 2UT MD Anderson Cancer Center, Houston, TX
Introduction: Gender- and race-based disparities persist in gastroenterology (GI), despite growing awareness of inequities in medicine. Women and underrepresented minorities (URMs) frequently face microaggressions, role misidentification, exclusion from advancement, and institutional inaction. Though awareness has grown, these experiences remain underreported. Under the ACG Summer Scholars Program, this study was developed to explore the impact of these challenges. We hypothesize that microaggressions are highly prevalent among women in GI, contributing to adverse emotional, professional, and institutional outcomes—particularly in clinical and educational settings—and that these experiences vary by age and practice setting.
Methods: An anonymous 33-question cross-sectional survey was distributed through GI-focused networks. It assessed demographics, familiarity with microaggressions, personal and witnessed experiences, perceived causes, responses, and institutional support. Quantitative data were analyzed descriptively, with subgroup comparisons by age (≤44 vs >44) and setting (academic vs private). Qualitative data underwent thematic analysis.
Results: Fifty-nine respondents—all women—completed the survey. Most were aged 35–44 (54%), mid-career (41%), and in academic (32%) or private (39%) practice. Overall, 92% reported experiencing microaggressions, mostly in clinical (89%) and admin (66%) settings. Perpetrators included patients (62.3%), senior GIs (54.7%), nurses (58.5%), and supervisors (41.5%). Microaggressions were verbal (83.3%) or non-verbal (77.8%) and attributed to gender (97.2%), age (63.9%), and race (38.9%).
Younger respondents (< 45) reported more frequent, emotionally distressing experiences, including burnout and imposter syndrome. Those in private practice cited more patient-driven incidents; those in academia cited more peer- and trainee-related events. Only 41.7% felt moderately comfortable addressing bias. Of those who responded, 38.9% faced retaliation, exclusion, or poor evaluations. Only 14% had access to effective reporting systems.
Discussion: Microaggressions are pervasive in GI, particularly among women and younger professionals. Experiences vary by setting and age, often leading to emotional distress and professional isolation. Despite institutional diversity efforts, support systems remain inadequate. Addressing this gap requires leadership accountability, inclusive mentorship, responsive reporting structures, and a culture that empowers individuals to speak up safely.
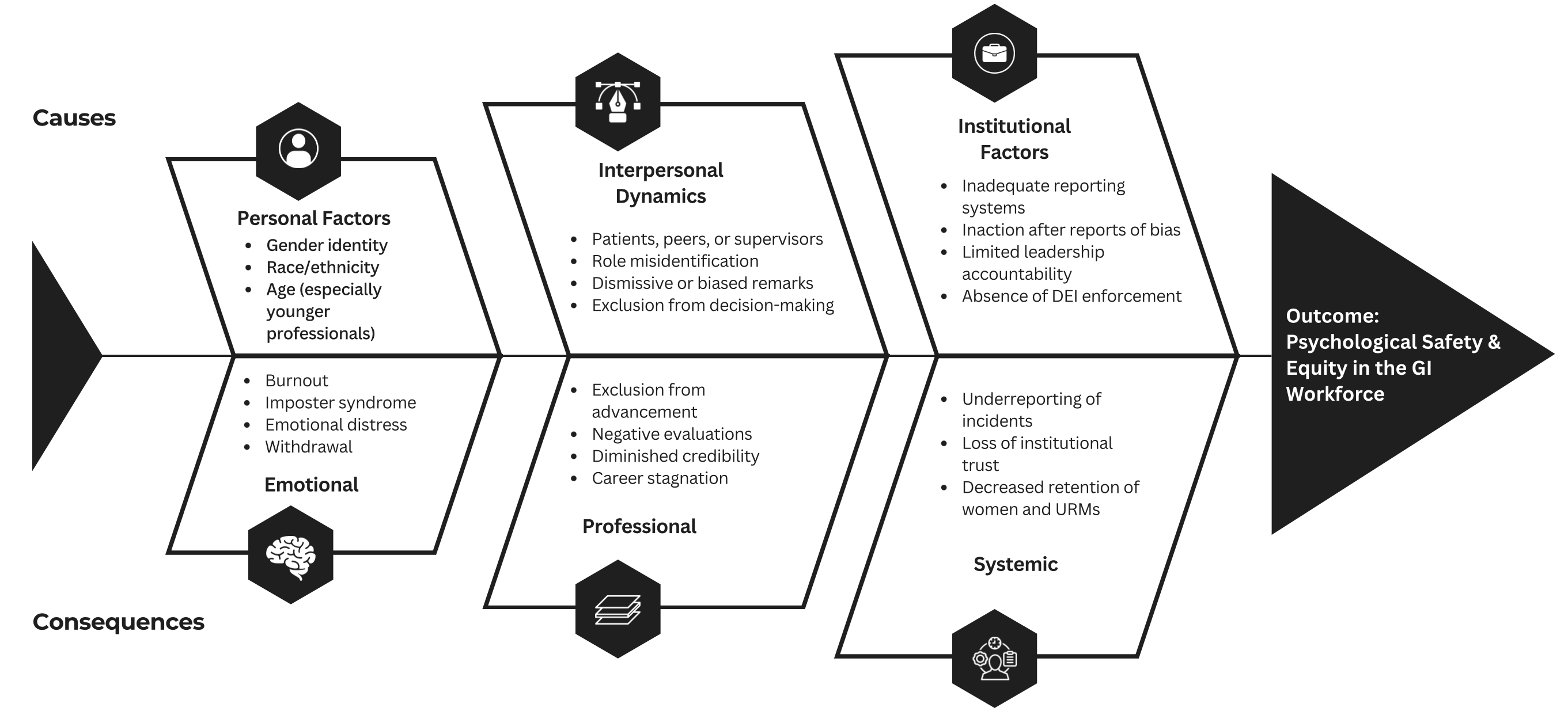
Figure: Figure 1. "Microaggressions in Gastroenterology: Drivers and Consequences"
Fishbone diagram illustrating the perceived causes and reported impacts of microaggressions experienced by women in gastroenterology based on survey responses.
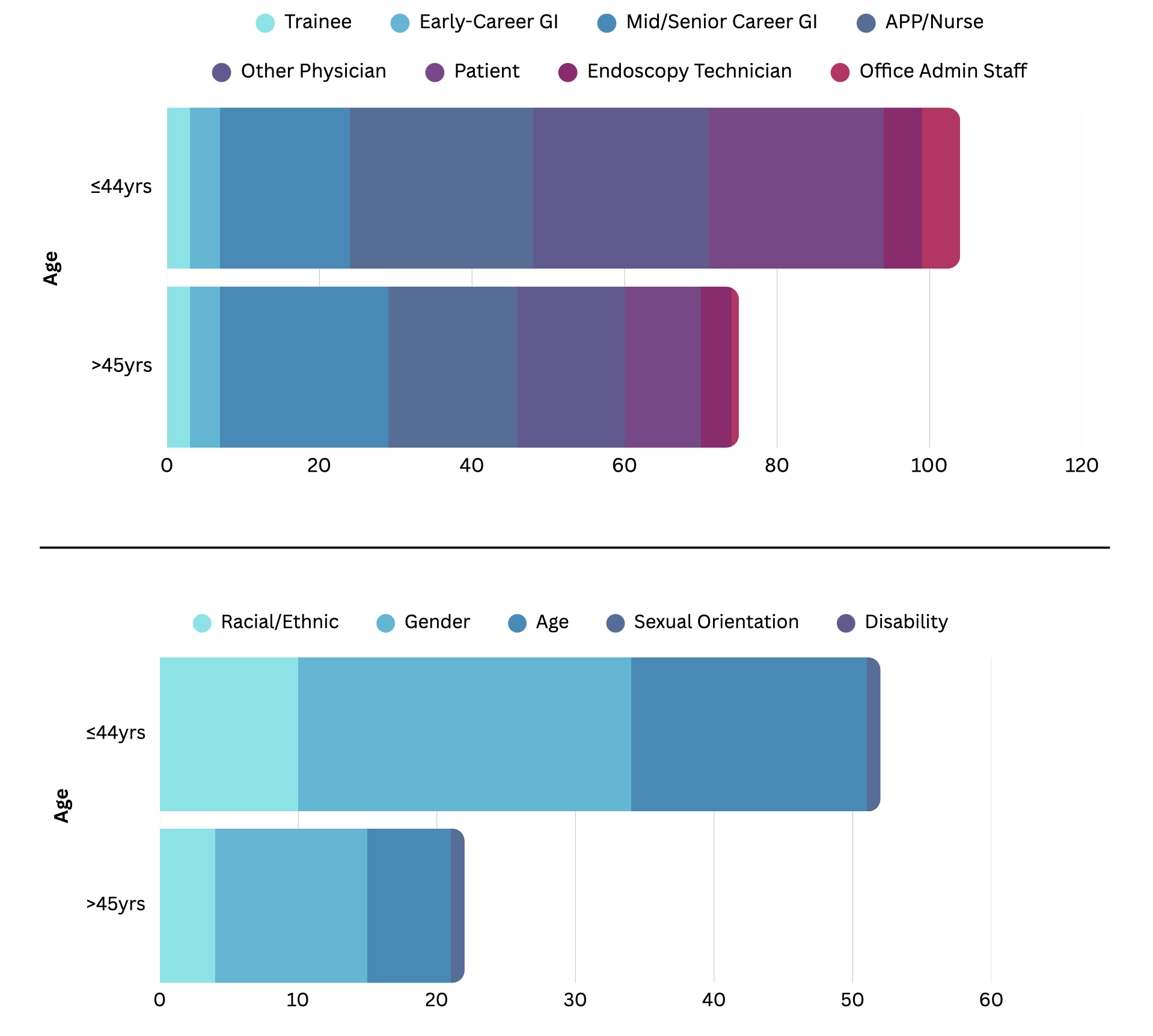
Figure: Figure 2. Age-stratified patterns of microaggressions reported by women in GI.
Top: "Perpetrators of Microaggressions by Age Group"
Perpetrators of microaggressions by age group, with respondents aged ≤44 more frequently identifying patients, nurses, and senior colleagues.
Bottom: "Types of Microaggressions Reported by Age Group"
Types of microaggressions reported by age group, with younger respondents more likely to report gender- and age-related bias.
Disclosures:
Chioma Owo indicated no relevant financial relationships.
Lavanya Viswanathan: Ardelyx, Inc. – Advisor or Review Panel Member, The above are unpaid., Speakers Bureau.
Chioma Owo, MD1, Lavanya Viswanathan, MD, MS, FACG2. P1922 - Beyond the Endoscopy Suite: A Survey-Based Study of Microaggressions and Workplace Bias in Gastroenterology, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
