Sunday Poster Session
Category: Pediatrics
P1898 - Trusting Your Gut: A Hairy Situation
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Amy Yeung, DO (she/her/hers)
Valley Health System, Icahn School of Medicine at Mount Sinai
Paramus, NJ
Presenting Author(s)
Amy Yeung, DO, Lauren Dankner, MD, Eric Lazar, MD, Linda Li, MD, MS, Khadijah Walker, APN, Antonio Quiros, MD, Sita Chokhavatia, MD, MACG
Valley Health System, Icahn School of Medicine at Mount Sinai, Paramus, NJ
Introduction: Trichobezoar, derived from the Greek word trich, meaning hair, is a mass formed by the accumulation of ingested human hair within the gastric lumen. Continuous ingestion, often mixed with food particles, leads to an increase in volume, creating gastric outlet obstruction, abdominal pain, distension, and vomiting. Trichobezoars commonly affect young females and are associated with trichotillomania or trichophagia. Diagnosis can be established through endoscopy or imaging. We present a case of trichobezoar in a young girl, diagnosed only through endoscopy after multiple inconclusive imaging studies.
Case Description/
Methods: A 7-year-old previously healthy girl presented with a 3-week history of intermittent upper abdominal pain, early satiety, and 4.5-kilogram weight loss. There was no vomiting, diarrhea, or altered bowel habits. She was afebrile with normal vital signs. Lab work revealed normal white blood cell count (11.6 x 10³/μL), hemoglobin (13.1 g/dL), mild thrombocytosis (499 × 10³/μL), mildly elevated lipase (107 U/L) and iron deficiency (Fe 17 μg/dL, total iron-binding capacity 345 µg/dL, iron saturation 5%).
Abdominal radiography and ultrasound were normal. Abdominal and pelvic magnetic resonance imaging showed significant gastric and proximal duodenal distention, suggestive of superior mesenteric artery syndrome. A subsequent upper gastrointestinal series revealed duodenal dilation with a gastric filling defect. A diagnostic esophagogastroduodenoscopy (EGD) confirmed a large trichobezoar with surrounding ulceration (Figure 1a). She underwent a laparoscopic gastrotomy with removal of the mass (Figure 1b). Postoperatively, her parents reported a habit of sucking and ingesting her hair when anxious, with changes in her hairline suggesting trichotillomania. She was discharged home on a proton-pump inhibitor and referred to behavioral therapy. At follow-up, she regained 2.3 kilograms with no further reports of trichotillomania.
Discussion: Trichobezoar should be considered in the differential diagnosis of children with unexplained gastrointestinal symptoms, weight loss, or alopecia. Imaging may aid in diagnosis but is often inconclusive. EGD remains the gold standard for both diagnosis and potential treatment. Early recognition, surgical management, and appropriate psychiatric support are crucial to preventing complications and recurrence.
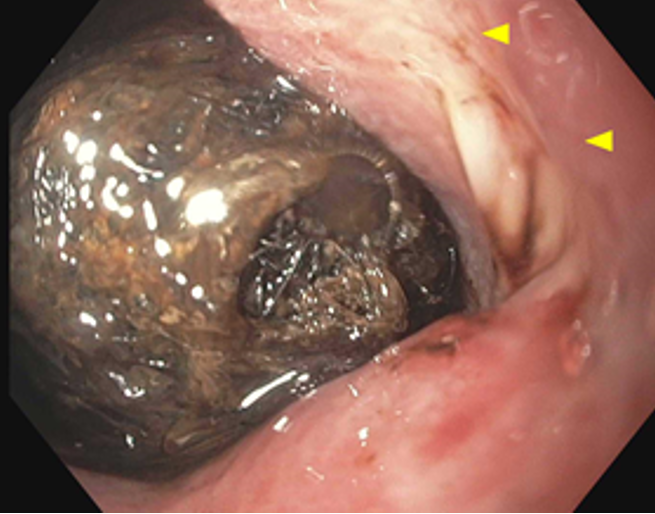
Figure: Figure 1a: Trichobezoar and adjacent gastric body ulceration.

Figure: Figure 1b: 10.0 x 3.2 x 3.0 cm gastric trichobezoar.
Disclosures:
Amy Yeung indicated no relevant financial relationships.
Lauren Dankner indicated no relevant financial relationships.
Eric Lazar indicated no relevant financial relationships.
Linda Li indicated no relevant financial relationships.
Khadijah Walker indicated no relevant financial relationships.
Antonio Quiros indicated no relevant financial relationships.
Sita Chokhavatia indicated no relevant financial relationships.
Amy Yeung, DO, Lauren Dankner, MD, Eric Lazar, MD, Linda Li, MD, MS, Khadijah Walker, APN, Antonio Quiros, MD, Sita Chokhavatia, MD, MACG. P1898 - Trusting Your Gut: A Hairy Situation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Valley Health System, Icahn School of Medicine at Mount Sinai, Paramus, NJ
Introduction: Trichobezoar, derived from the Greek word trich, meaning hair, is a mass formed by the accumulation of ingested human hair within the gastric lumen. Continuous ingestion, often mixed with food particles, leads to an increase in volume, creating gastric outlet obstruction, abdominal pain, distension, and vomiting. Trichobezoars commonly affect young females and are associated with trichotillomania or trichophagia. Diagnosis can be established through endoscopy or imaging. We present a case of trichobezoar in a young girl, diagnosed only through endoscopy after multiple inconclusive imaging studies.
Case Description/
Methods: A 7-year-old previously healthy girl presented with a 3-week history of intermittent upper abdominal pain, early satiety, and 4.5-kilogram weight loss. There was no vomiting, diarrhea, or altered bowel habits. She was afebrile with normal vital signs. Lab work revealed normal white blood cell count (11.6 x 10³/μL), hemoglobin (13.1 g/dL), mild thrombocytosis (499 × 10³/μL), mildly elevated lipase (107 U/L) and iron deficiency (Fe 17 μg/dL, total iron-binding capacity 345 µg/dL, iron saturation 5%).
Abdominal radiography and ultrasound were normal. Abdominal and pelvic magnetic resonance imaging showed significant gastric and proximal duodenal distention, suggestive of superior mesenteric artery syndrome. A subsequent upper gastrointestinal series revealed duodenal dilation with a gastric filling defect. A diagnostic esophagogastroduodenoscopy (EGD) confirmed a large trichobezoar with surrounding ulceration (Figure 1a). She underwent a laparoscopic gastrotomy with removal of the mass (Figure 1b). Postoperatively, her parents reported a habit of sucking and ingesting her hair when anxious, with changes in her hairline suggesting trichotillomania. She was discharged home on a proton-pump inhibitor and referred to behavioral therapy. At follow-up, she regained 2.3 kilograms with no further reports of trichotillomania.
Discussion: Trichobezoar should be considered in the differential diagnosis of children with unexplained gastrointestinal symptoms, weight loss, or alopecia. Imaging may aid in diagnosis but is often inconclusive. EGD remains the gold standard for both diagnosis and potential treatment. Early recognition, surgical management, and appropriate psychiatric support are crucial to preventing complications and recurrence.
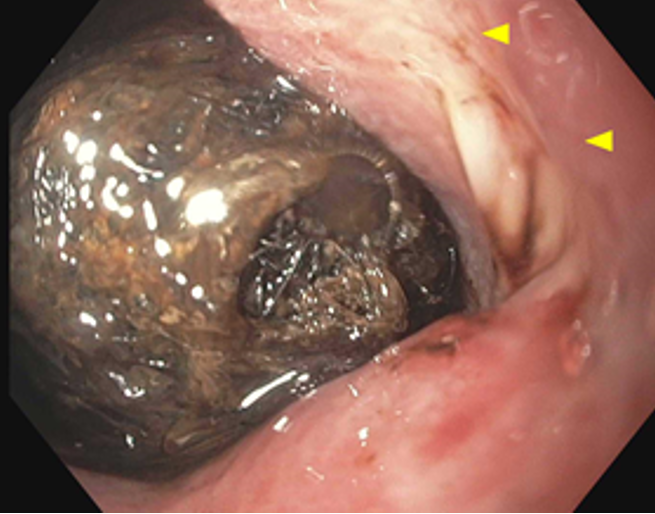
Figure: Figure 1a: Trichobezoar and adjacent gastric body ulceration.

Figure: Figure 1b: 10.0 x 3.2 x 3.0 cm gastric trichobezoar.
Disclosures:
Amy Yeung indicated no relevant financial relationships.
Lauren Dankner indicated no relevant financial relationships.
Eric Lazar indicated no relevant financial relationships.
Linda Li indicated no relevant financial relationships.
Khadijah Walker indicated no relevant financial relationships.
Antonio Quiros indicated no relevant financial relationships.
Sita Chokhavatia indicated no relevant financial relationships.
Amy Yeung, DO, Lauren Dankner, MD, Eric Lazar, MD, Linda Li, MD, MS, Khadijah Walker, APN, Antonio Quiros, MD, Sita Chokhavatia, MD, MACG. P1898 - Trusting Your Gut: A Hairy Situation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
